
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2024 | 65 (1) | 40-45
Case report
Non-surgical management of paresthesia induced by calcium hydroxide extrusion – a case report with a 4-year follow-up
Abordagem não cirúrgica de um caso de parestesia induzida pela extrusão de hidróxido de cálcio – caso clínico com 4 anos de controlo
a Department of Conservative Dentistry and Endodontics, Pacific Dental College and Hospital, Udaipur, Rajasthan, India
b Private Practice, Turkey
c Assistant Professor, Department of Restorative Dentistry, Faculty of Dental Medicine, Umm Al-Qura University, Makkah, Saudi Arabia
d Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
e Grupo de Investigação em Bioquímica e Biologia Oral, Unidade de Investigação em Ciências Orais e Biomédicas (UICOB), Lisbon, Portugal
f Centro de Estudo de Medicina Dentária Baseada na Evidência (CEMDBE), Lisbon, Portugal
g Department of Endodontics, Faculty of Dentistry, Medeniyet University, Istanbul, Turkey
Jorge N.R. Martins - jnr_martins@yahoo.com.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 65
Issue - 1
Case report
Pages - 40-45
Go to Volume
Article History
Received on 01/11/2023
Accepted on 15/02/2024
Available Online on 25/03/2024
Keywords
Clinical Case Report
�Non-surgical management of paresthesia induced by calcium hydroxide extrusion � a case report with a 4-year follow-up
Abordagem n�o cir�rgica de um caso de parestesia induzida pela extrus�o de hidr�xido de c�lcio � caso cl�nico com 4 anos de controlo
�
Afzal Ali1 0000-0002-0174-4656
Sevda Tok2 0000-0001-7909-8386
Abdulaziz Bakhsh3 0000-0003-3228-2025
Joge N.R. Martins4,5,6,* 0000-0002-6932-2038
Hakan Arslan7 0000-0003-4890-1062
�
1 Department of Conservative Dentistry and Endodontics, Pacific Dental College and Hospital, Udaipur, Rajasthan, India.
2 Private Practice, Turkey.
3 Assistant Professor, Department of Restorative Dentistry, Faculty of Dental Medicine, Umm Al-Qura University, Makkah, Saudi Arabia.
4 Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal.
5 Grupo de Investiga��o em Bioqu�mica e Biologia Oral, Unidade de Investiga��o em Ci�ncias Orais e Biom�dicas (UICOB), Lisbon, Portugal.
6 Centro de Estudo de Medicina Dent�ria Baseada na Evid�ncia (CEMDBE), Lisbon, Portugal.
7 Department of Endodontics, Faculty of Dentistry, Medeniyet University, Istanbul, Turkey.
�
�
Article history:
Received 1 November 2023
Accepted 15 February 2024
Available online 21 March 2024
�
Abstract
The present case report describes the non-surgical treatment of alveolar inferior nerve paresthesia caused by the extrusion of calcium hydroxide as intracanal medicament. A 45-year-old female patient had a chief complaint of numbness and pain in the left lower lip region for 2 months. Radiographic examination revealed calcium hydroxide overflow into the mandibular canal. Irrigation of the root canal system with saline using a 27-gauge needle was done to remove as much calcium hydroxide as possible but proved ineffective in removing material from the outside tissues. Root canal treatment was completed in 1 week, and non-surgical paresthesia treatment with steroids and pregabalin was done for one month. In the 1-year follow-up control, the paresthesia had reduced significantly. In a 4-year follow-up visit, there was a complete resolution of paresthesia, and the radiographic analysis showed that calcium hydroxide was completely resorbed.
Keywords: Calcium hydroxide,Endodontics, Material extrusion,Paresthesia,Root canal therapy
�
Resumo
O presente caso cl�nico descreve o tratamento n�o cir�rgico de uma parestesia do nervo alveolar inferior provocada pela extrus�o de medica��o intracanalar de hidr�xido de c�lcio. Uma paciente de 45 anos de idade apresentou-se referindo como queixa principal a dorm�ncia e dor na regi�o do l�bio inferior esquerdo com 2 meses de evolu��o. O exame radiogr�fico revelou a extrus�o de hidr�xido de c�lcio no canal mandibular. Irriga��o com soro fisiol�gico, usando uma agulha 27-G, foi usada para eliminar a maior quantidade poss�vel de hidr�xido de c�lcio do espa�o intracanalar, mas revelou-se ineficaz na elimina��o do material dos tecidos circundantes. O tratamento endod�ntico foi conclu�do no espa�o de uma semana, e o tratamento n�o cir�rgico da parestesia foi realizado recorrendo a esteroides e pregabalina por um per�odo de 1 m�s. No controlo de 1 ano, a parestesia havia regredido significativamente. Na visita de controlo dos 4 anos, constatou-se a completa resolu��o da parestesia, e o controlo radiogr�fico evidenciou a completa reabsor��o do hidr�xido de c�lcio
Palavras-chave: Hidr�xido de c�lcio,Endodontia, Extrus�o de material,Parestesia,Tratamento endod�ntico
�
Introduction
During the endodontic treatment, the overpreparation of mandibular premolars� and molars� root canals may facilitate further extrusion of the intracanal medicament (ICM) and/or root canal filling material from the root apices, causing neurological complications, such as Nicolau Syndrome also known as embolia cutis medicamentosa.1 Nicolau Syndrome consists of a cutaneous adverse reaction at the site of a particular drug application, such as hypoesthesia, dysesthesia, and anesthesia, in areas innervated by the inferior alveolar nerve (IAN).2 Injuries to the IAN during dental treatment are uncommon but represent a serious complication.3 Namely, they may result in permanent paresthesia, defined as a sensitivity loss lasting more than 6 months.4 Facial paresthesia is often felt via the mental, lingual, and IANs. The main symptom is a loss of sensation in the affected nerve area, although the patient may have also altered perceptions of hot and cold, tingling, itching, and numbness later on.5
Calcium hydroxide is used as an ICM during the endodontic procedure due to its high bactericidal effect and alkalinity.6 With Ca+2 and OH− ions, calcium hydroxide has an antibacterial effect and reduces the production of hard tissue.7 Moreover, some authors reported that it has an osteoblastic impact on inflamed tissue in the periapical region.8
Several possible mechanisms and treatment options exist when an endodontically treated tooth develops an atypical symptom.9 Possible injury mechanisms include pressure, neurotoxic effects, and mechanical trauma. Considering that trauma, pressure, and neurotoxicity during endodontic treatment procedures may cause nerve damage, the clinician should choose between eliminating and monitoring pain and inflammation and surgically removing the cause.10 - 13 However, some studies suggested a non-surgical approach for managing such complications.14 - 18
Pregabalin is a gamma-aminobutyric acid (GABA) analog with the same structure and action as gabapentin that is effective in chronic and neuropathic pain. It has an analgesic effect by reducing neurotransmitter release.19 - 21 The presente case report intends to debate the clinical condition of a patient who was presenting with pain and paresthesia caused by calcium hydroxide extrusion and who recovered completely with a non-surgical approach using pregabalin and steroids.
Case report
On May 27, 2019, a 45-year-old female patient attended na endodontic consultation with a chief complaint of pain and numbness over the left lower lip region for 2 months. The medical history and radiograph analysis revealed that a root canal treatment had been initiated on the mandibular left second molar (tooth 37). The patient had been experiencing left lower lip paresthesia since then. The periapical radiographic examination also revealed an apparent ICM extrusion on tooth 37 (Figure 1). Panoramic radiography was performed (Figure 2) to assess the degree of ICM extrusion, and the area of paresthesia was delimited by tactile exploration with the explorer (Figure 3). The patient was diagnosed with a previously initiated root canal treatment with symptomatic apical periodontitis associated with lower lip parestesia possibly provoked by ICM extrusion. The previous doctor later confirmed that the extruded material was calcium hydroxide. Root canal treatment continuation was recommended to the patient, associated with pharmacological therapy aiming to reverse the neurological damage. After the patient�s acceptance, anesthesia and isolation were performed, and acces� to the canal space was re-established. The ICM (Ca(OH)2) was removed from tooth 37�s root canal system space with a saline solution using a 37 gauge needle. However, the extruded ICM in the inferior alveolar canal could not be removed. Root canal treatment was performed for tooth 37 according to the European Society of Endodontology�s 2006 quality guidelines. Root canal instrumentation was performed using the Protaper Universal system (Dentsply, Ballaigues, Switzerland). Following the manufacturer�s instructions, the mesial root canals were prepared up to F2 and the distal ones up to F3. Irrigation was performed with sodium hypochlorite at 5.25% and saline solution. The tooth was obturated with gutta-percha and Sealapex (Sybron Kerr, Romulus, MI, USA) sealer with a continuous wave of condensation technique. Analgesics and antibiotics were prescribed for 3 days. Steroids (Predniheal 20mg SSR Healthcare, Nagpur, India; the dosage [two doses] was tapered and stopped in two weeks) and pregabalin (Lyrica 75mg Pfizer, Mumbai, India; 150 mg per day) were prescribed for 1 month. One week later, the root canal treatment was completed (June 2019).
�
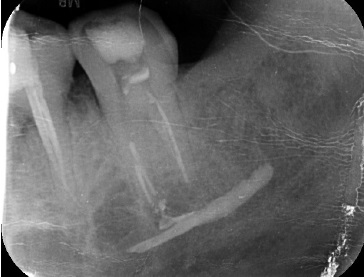
Figure 1. Pre-operative periapical radiograph evidencing the presence of an intracanal medicamente inside the mandibular canal
�

Figure 2. Pre-operative panoramic radiograph
�

Figure 3. Pre-operative clinical view delimiting the �rea of paresthesia.
�
In an 8-month follow-up visit (February 2020), the area of paresthesia was reduced (Figure 4), and tooth 35 was extracted for reasons non-related to the present report. Due to the Covid-19 pandemic, the patient could not perform the following evaluation visit. However, in a telephone conversation, she mentioned being asymptomatic and wanting further clinical evaluation. In September 2022, because the patient was bedridden due to a road traffic accident, a home visit was performed to assess the degree of paresthesia. Clinical examination suggested complete resolution of the paresthesia, and a periapical radiograph revealed the absence of ICM near the root apices of tooth 37 (Figure 5). In a 4-year follow-up (June 2023), the patient was asymptomatic. Prosthetic rehabilitation was done (Figure 6), and the complete resolution of calcium hydroxide was evident in the panoramic radiography (Figure 7).
�

Figure 4. Clinical view at the 8-month follow-up visit showing reduced area of paresthesia.
�

Figure 5. Periapical radiograph showing the absence of calcium hydroxide inside the mandibular canal
�

Figure 6. Periapical radiograph following prosthetic rehabilitation (4-year follow-up)
�

Figure 7. Panoramic radiograph at the 4-year follow-up showing the absence of intracanal medication inside the mandibular canal
�
Discussion and conclusions
Paresthesia is the permanent or temporary sensation of tingling, tickling, or prickling.22 Mechanical preparation with excessive root canal working length on mandibular molars and premolars and endodontic material extrusion are potential iatrogenic causes of IAN damage.23 Most cases of endodontic paresthesia result from an overpreparation or overfilling of the mandibular canal with endodontic materials.1, 24 These cases of paresthesia occurring during and after root canal treatment of molars and premolars have been the subject of previous reports.25, 26
At body temperature, calcium hydroxide has a low solubility. Serper et al.27 showed that calcium hydroxide may cause foreign body reactions, nerve inflammation, and bone necrosis.
In addition, when an excess of calcium hydroxide remains in the nerve tissue for more than 30 min, it may cause irreversible obstruction of nerve conduction, resulting in an imbalance in the nerve membrane potential. The first sign of calcium hydroxide extrusion in the mandibular canal is pain persisting after the anesthesia has disappeared.28 The literature shows that extrusion can induce transient inflammation ranging from mild to severe.29, 30 It may be accompanied by pain on percussion and palpation due to local inflammation and lower lip or ear pain or numbness, which is a combination of signs of mechanical trauma and inferior dental neuritis.31 In some patients, anesthesia may persist.2, 13, 23, 32
Pregabalin, an analog of the inhibitory neurotransmitter GABA, is mainly used in the treatment of trigeminal neuropathic pain and chronic pain.19, 33 It is also often used in peripheral neuropathic pain.17, 34 The United States Food and Drug Administration (FDA) (2004) has approved the use of two drugs for peripheral neuropathic pain: duloxetine and pregabalin. Pregabalin, which has an analgesic effect, improves symptoms significantly in 1 week and remains effective during the treatment.35, 36 Its oral bioavailability is approximately 90%, with peak plasma levels occurring after approximately 1 hour.
Pregabalin is not protein-dependent, with a plasma half-life of 6 hours that is not dose-dependent. It has fewer drug interactions and little effect on hepatic enzymes.35 While renal excretion accounts for 95% of the oral dose, hepatic metabolism is insignificant. Pregabalin administration is an effective and well-tolerated treatment for neuropathic pain.38 In the presente case, pregabalin treatment was initiated based on existing documented evidence, considering the nerve damage that causes neuropathic pain after calcium hydroxide extrusion to the mandibular canal.
The present 4-year follow-up case report revealed the complete resolution of paresthesia and the disappearance of ICM extrusion with the non-surgical approach. The combination of steroids and pregabalin may be considered a viable option for complete resolution of paresthesia.
In conclusion, ICMs are prone to induce neurotoxic effects following extrusion into the inferior alveolar canal. The clinician should be cautious while preparing the root canal system space to avoid apical violation or overfilling with the ICM or obturating materials. The non-surgical treatment should be considered a viable initial approach over surgical management.
�
References
1. Al-sheeb F, Al Mannai G, Tharupeedikayil S. Nicolau syndrome after endodontic treatment: a case report. J Endod. 2022;48:269-72.
2. Givol N, Rosen E, Bj�rndal L, Taschieri S, Ofec R, Tsesis I. Medico-legal aspects of altered sensation following endodontic treatment: a retrospective case series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:126-31.
3. �rstavik D, Brodin P, Aas E. Paraesthesia following endodontic treatment: survey of the literature and report of a case. Int Endod J. 1983;16:167-72.
4. Tilotta-Yasukawa F, Millot S, El Haddioui A, Bravetti P, Gaudy J-F. Labiomandibular paresthesia caused by endodontic treatment: an anatomic and clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e47-59.
5. Alves FR, Coutinho MS, Gon�alves LS. Endodontic-related facial paresthesia: systematic review. J Can Dent Assoc. 2014;80:e13.
6. Athanassiadis B, Abbott P, Walsh LJ. The use of calcium hydroxide, antibiotics and biocides as antimicrobial medicaments in endodontics. Aust Dent J. 2007;52:S64-82.
7. Fava L, Saunders W. Calcium hydroxide pastes: classification and clinical indications. Int Endod J. 1999;32:257-82.
8. Tronstad L, Andreasen J, Hasselgren G, Kristerson L, Riis I. pH changes in dental tissues after root canal filling with calcium hydroxide. J Endod. 1981;7:17-21.
9. Pogrel MA. Damage to the inferior alveolar nerve as the result of root canal therapy. J Am Dent Assoc. 2007;138:65-9.
10. Dempf R, Hausamen J. Lesions of the inferior alveolar nerve arising from endodontic treatment. Aust Endod J. 2000;26:67-71.
11. Montgomery S. Paresthesia following endodontic treatment. J Endod. 1976;2:345-7.
12. Pogrel MA. Neurotoxicity of available root sealant pastes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:385.
13. Gr�tz K, Al-Nawas B, De Aguiar E, Schulz A, Wagner W. Treatment of injuries to the inferior alveolar nerve after endodontic procedures. Clin Oral Investig. 1998;2:73-6.
14. Blanas N, Kienle F, Sandor GK. Injury to the inferior alveolar nerve due to thermoplastic gutta percha. J Oral Maxillofac Surg. 2002;60:574-6.
15. Froes FGB, Miranda �MMA, Abad EdC, Riche FN, Pires FR. Non‐surgical management of paraesthesia and pain associated with endodontic sealer extrusion into the mandibular canal. Aust Endod J. 2009;35:183-6.
16. Gonz�lez-Mart�n M, Torres-Lagares D, Guti�rrez-P�rez JL, Segura-Egea JJ. Inferior alveolar nerve paresthesia after overfilling of endodontic sealer into the mandibular canal. J Endod. 2010;36:1419-21.
17. L�pez‐L�pez J, Estrugo‐Devesa A, Jan�‐Salas E, Segura‐Egea J. Inferior alveolar nerve injury resulting from overextension of an endodontic sealer: non‐surgical management using the GABA analogue pregabalin. Int Endod J. 2012;45:98-104.
18. Poveda R, Bag�n JV, Fern�ndez JMD, Sanchis JM. Mental nerve paresthesia associated with endodontic paste within the mandibular canal: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e46-9.
19. Ferre-Corominas J, Chimenos-Kuestner E, L�pez-L�pez J. Odontologic considerations in fibromyalgia. Med Clin (Barc). 2011;137:27-9.
20. Jain P, Jolly A, Bholla V, Adatia S, Sood J. Evaluation of efficacy of oral pregabalin in reducing postoperative pain in patients undergoing total knee arthroplasty. Ind J Orthop. 2012;46:646-52.
21. Zareba G. Pregabalin: a new agent for the treatment of neuropathic pain. Drugs of Today. 2005;41:509-16.
22. Di Lenarda R, Cadenaro M, Stacchi C. Paresthesia of the mental nerve induced by periapical infection: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:746-9.
23. Escoda-Francoli J, Canalda-Sahli C, Soler A, Figueiredo R, Gay-Escoda C. Inferior alveolar nerve damage because of overextended endodontic material: a problem of sealer cement biocompatibility? J Endod. 2007;33:1484-9.
24. Ahonen M, Tj�derhane L. Endodontic-related paresthesia: a case report and literature review. J Endod. 2011;37:1460-4.
25. Lambrianidis T, Molyvdas J. Paresthesia of the inferior alveolar nerve caused by periodontal-endodontic pathosis. Oral Surg Oral Med Oral Pathol. 1987;63:90-2.
26. Giuliani M, Lajolo C, Deli G, Silveri C. Inferior alveolar nerve paresthesia caused by endodontic pathosis: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:670-4.
27. Serper A, ��er O, Onur R, Etikan Ib. Comparative neurotoxic effects of root canal filling materials on rat sciatic nerve. J Endod. 1998;24:592-4.
28. LaBanc JP, Epker BN. Serious inferior alveolar nerve dysesthesia after endodontic procedure: report of three cases. J Am Dent Assoc. 1984;108:605-7.
29. Scarparo RK, Grecca FS, Fachin EVF. Analysis of tissue reactions to methacrylate resin-based, epoxy resin-based, and zinc oxide�eugenol endodontic sealers. J Endod. 2009;35:229-32.
30. Zmener O, Banegas G, Pameijer CH. Bone tissue response to a methacrylate-based endodontic sealer: a histological and histometric study. J Endod. 2005;31:457-9.
31. Tamse A, Kaffe I, Littner M, Kozlovsky A. Paresthesia following overextension of AH-26: report of two cases and review of the literature. J Endod. 1982;8:88-90.
32. Rowe A. Damage to the inferior dental nerve during or following endodontic treatment. Br Dent J. 1983;155:306-7.
33. Zakrzewska JM. Medical management of trigeminal neuropathic pains. Expert Opin Pharmacother. 2010;11:1239-54.
34. Alonso-Ezpeleta O, Mart�n PJ, L�pez-L�pez J, Castellanos-Cosano L, Mart�n-Gonz�lez J, Segura-Egea JJ. Pregabalin in the treatment of inferior alveolar nerve paraesthesia following overfilling of endodontic sealer. J Clin Exp Dent. 2014;6:e197.
35. Bender G, Gosset J, Florian J, Tan K, Field M, Marshall S, et al. Population pharmacokinetic model of the pregabalinsildenafil interaction in rats: application of simulation to preclinical PK-PD study design. Pharm Res. 2009;26:2259-69.
36. Buvanendran A, Kroin JS, Kari MR, Tuman KJ. A new knee surgery model in rats to evaluate functional measures of postoperative pain. Anesth Analg. 2008;107:300-8
37. Cohen DM, Reinhardt RA. Systemic sarcoidosis presenting with Horner�s syndrome and mandibular paresthesia. Oral Surg Oral Med Oral Pathol. 1982;53:577-81.
38. Toth C. Pregabalin: latest safety evidence and clinical implications for the management of neuropathic pain. Ther Adv Drug Saf. 2014;5:38-56.
�
Jorge N.R. Martins
E-mail address: jnr_martins@yahoo.com.br
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Afzal Ali: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing � original draft, Writing � review & editing. Sevda Tok: Methodology, Writing � original draft, Writing � review & editing. Abdulaziz Bakhsh: Supervision, Visualization, Writing � review & editing. Jorge NR Martins: Validation, Supervision, Visualization, Writing � review & editing. Hakan Arslan: Validation, Writing � review & editing.
�
1646-2890/� 2024 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
