
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (1) | 16-22
Original research
Bond strength of orthodontic brackets to polymethylmethacrylate: effect of the surface treatment and adhesive system
Adesão de brackets ortodônticos a polimetilmetacrilato: Efeito do tratamento de superfície e do sistema adesivo
a Department of Orthodontics, Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
Rita Matos Cardoso - rita.matoscardoso@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 1
Original research
Pages - 16-22
Go to Volume
Article History
Received on 19/09/2020
Accepted on 24/12/2020
Available Online on 29/01/2021
Keywords
Original Research
�
Bond strength of orthodontic brackets to polymethylmethacrylate: effect of the surface treatment and adhesive system
Ades�o de brackets ortod�nticos a polimetilmetacrilato: Efeito do tratamento de superf�cie e do sistema adesivo Palavras-chave:
�
Rita Matos Cardosoa*, Joana Godinho, Lu�s Jardima
aDepartment of Orthodontics, Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal
�
�
Article history:
Received 19 September 2020
Accepted 24 December 2020
Available online 29 January 2021
�
Abstrac
Objectives:To evaluate the influence of the surface treatment and adhesive system on the shear bond strength and the failure mode of orthodontic brackets bonded to polymethylmethacrylate surfaces.
Methods:Ninety metal brackets (n=15) were bonded to aged discs of polymethylmethacrylate SR Ivocron subjected to three surface conditions (no treatment; sandblasting with 50-μm aluminum oxide; roughening with a tungsten bur), using two combinations of adhesives (methylmethacrylate monomer + Transbond XT Primer; Scotchbond Universal Adhesive) followed by the composite Transbond XT. In the control group, metal brackets were bonded with Transbond XT to 15 human mandibular incisors. The specimens were thermocycled, stored in distilled water (37oC, 7 days), and tested in shear, using an Instron universal machine. Failure mode was classified according to the adhesive remnant index using a stereomicroscope. The data were analyzed with an analysis of variance and posthoc tests (p<0.05).
Results:Significant differences were found between the bracket bond strength to polymethylmethacrylate with different surface treatments (p<0.001). Sandblasting with aluminum oxide was superior to tungsten bur roughening. The adhesive system did not significantly influence the shear bond strength nor the failure mode (p=0.8415). All experimental groups showed lower bond strengths than the control group (p=0.1566).
Conclusions:Mechanical surface treatment significantly influenced the bracket�s bond strength to polymethylmethacrylate. Sandblasting with aluminum oxide was the most effective mechanical treatment. The weakest adhesive link was found at the acrylic-adhesive interface. Orthodontic bonding to polymethylmethacrylate was weaker than bonding to enamel, regardless of the surface treatment and the adhesive used.
Keywords: Adhesion,Adhesive remnant index,Adhesives,Brackets,Orthodontics,Polymethylmethacrylate, Shear strength, Surface treatment
�
Resumo
Objetivos:Avaliar a influ�ncia do tratamento de superf�cie e de sistemas adesivos na resist�ncia adesiva e tipo de falha de brackets met�licos cimentados a superf�cies de polimetilmetacrilato.
M�todos: 90 brackets met�licos (n=15) foram cimentados a discos de polimetilmetacrilato SR Ivocron envelhecidos, usando 3 condi��es de superf�cie (sem tratamento; jato de �xido de alum�nio de 50 μm; broca de tungst�nio), utilizando 2 combina��es de adesivos (mon�mero de metilmetacrilato + Transbond XT Primer; Scotchbond Universal Adhesive) seguido do comp�sito Transbond XT. Brackets cimentados a 15 incisivos mandibulares humanos com Transbond XT foram usados como controlo. A resist�ncia adesiva ao cisalhamento foi avaliada com Instron, ap�s termociclagem e armazenamento em �gua destilada (37�C, 7 dias). O tipo de falha foi classificado pelo �ndice de adesivo residual, utilizando um estereomicrosc�pio. Os dados foram analisados com uma an�lise de vari�ncia e testes post-hoc (p<0,05).
Resultados: Verificaram-se diferen�as significativas na ades�o ao polimetilmetacrilato entre os tratamentos da superf�cie (p<0,001), sendo o jateamento com �xido de alum�nio superior � abras�o com broca de tungst�nio. O sistema adesivo n�o influenciou significativamente a resist�ncia adesiva nem o tipo de falha (p=0,8415). Os grupos experimentais obtiveram valores de ades�o inferiores aos do controlo (p=0,1566).
Conclus�es: O tratamento mec�nico da superf�cie influenciou significativamente a ades�o de brackets ao polimetilmetacrilato. O jato de �xido de alum�nio foi o tratamento mec�nico mais eficaz. A uni�o acr�lico-adesivo foi o elo mais fraco da interface adesiva. A ades�o ao polimetilmetacrilato foi inferior � ades�o ao esmalte, independentemente do tratamento de superf�cie e do adesivo.
Palavras-chave: Ades�o,�ndice de adesivo residual,Adesivos,Brackets,Ortodontia, Polimetilmetacrilato,Resist�ncia ao cisalhamento,Tratamento de superf�cie
�
Introduction
The evolution of orthodontic techniques over the last decades has led to a significant increase in the number of adults seeking treatment. These patients often have restored teeth, and, in many cases, orthodontic procedures are performed concurrently with other dental treatments.1, 2 The presence of surfaces restored with different materials makes it difficult to bond orthodontic brackets, which has motivated studies on adhesion to gold, amalgam, composite and ceramic surfaces.3 ‑ 8
In multidisciplinary treatments involving prosthodontics and orthodontics, the need for bonding brackets to temporary crowns arises to avoid damage to the final restoration.9 The materials used for manufacturing temporary crowns can be divided according to their chemical composition into two groups: methacrylate acrylic resins (polymethyl, polyethyl, and polyvinyl methacrylates) and Bis‑acryl and Bis‑GMA composite resins.10, 11 However, in more complex cases, namely multiple or long‑term provisional restorations, polymethylmethacrylate (PMMA) acrylic resins remain the materials of choice.12, 13
Previous studies have shown that brackets� bond strength to PMMA surfaces is lower than the clinically acceptable values.2, 14 In orthodontic practice, a weak adhesion of brackets to temporary materials leads to a high rate of adhesive failures, with adverse consequences on the cost and efficiency of orthodontic treatment and patient comfort.2 Brackets� bond strength to restorative materials should be strong enough to withstand the orthodontic forces but weak enough to allow for debonding without damaging the tooth surface.14
New universal adhesive systems aimed to improve the existing ones have been introduced in the market over the last decade. These adhesives are advertised as being effective for adhesion to various substrates due to various associated chemicals in their composition.15 ‑ 18 This versatility can be useful in bonding orthodontic brackets to PMMA crowns.
Although there are studies in the literature evaluating the influence of surface treatment on brackets� adhesion to provisional crowns,2 9, 14, 19 ‑ 21 no published research testing the new universal adhesives or the application of the methylmethacrylate monomer (MMA) combined with mechanical surface treatment was found. Therefore, the main objective of the present investigation was to evaluate the influence of surface treatment and two adhesive systems on the bond strength of metal brackets to PMMA surfaces, according to the following null hypotheses (H0): the adhesion of brackets to the PMMA surface is not significantly influenced by the adhesive system or the surface treatment. A secondary objective was to identify the types of bonding failure by comparing these different adhesive systems and surface treatrevments, testing the following hypotheses: the type of failure is not significantly influenced by the adhesive system or the surface treatment.
Material and methods
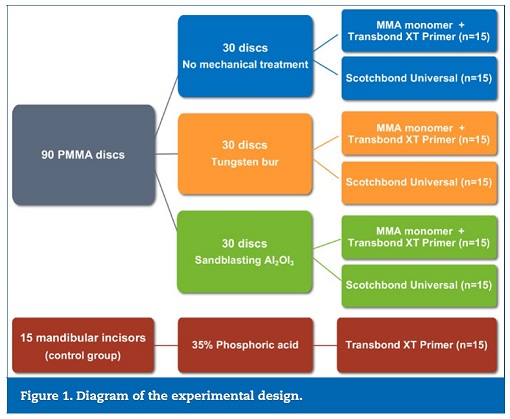
The study sample consisted of 90 self‑curing PMMA discs (SR Ivocron, Ivoclar Vivadent Inc, Amherst NY, USA) of standardized dimensions (7.5 x 3 mm), fabricated according to the manufacturer�s instructions. The PMMA discs were subjected to 500 cycles of thermocycling between 5oC and 55oC (20 seconds each bath) and stored in distilled water at 37oC for 55 days. The sample was randomly divided into three groups of 30 specimens each, depending on the surface treatment performed: no treatment, 50‑μm aluminum sandblasting (ASB group), or tungsten bur (TB group). Each group was then divided into two subgroups, according to the combination of adhesive materials to be tested: MMA monomer for 25 seconds followed by Transbond XT Primer (3M Unitek, St Paul MN, USA); or Scotchbond Universal Adhesive (3M ESPE, St Paul MN, USA).
The adhesive system was applied following a standardized protocol (Figure 1). A lower incisor metal bracket with a 0.018‑inch slot, 0� torque and angulation (Mini‑Twin, Ormco, Orange CA, USA), and a 9.9 mm2 base was bonded to each specimen.
�
�
Transbond XT Light Cure Adhesive composite (3M Unitek, St Paul MN, USA) was placed at the bracket base, and manual pressure was exerted to express excess adhesive, which was removed with a periodontal probe. The composite resin was polymerized with a 1200 mW/cm2 LED light (Bluephase 20i,
Ivoclar Vivadent Inc, Amherst NY, USA) for 20 seconds: 10 on the mesial side and 10 on the distal side of each bracket.
The control group consisted of 15 freshly extracted intact human mandibular incisors, which were stored in a bacteriostatic solution (0.5% chloramine) at 4�C, according to the ISO/TS 11405:2003.22 Their roots were sectioned, and their crowns were polished with a prophylactic brush using pumice and water. Their enamel was conditioned for 30 seconds with a 35% phosphoric acid solution (Transbond XT Etching Gel, 3M Unitek St Paul MN, USA), washed with running water for 15 seconds, and dried with an air spray for 5 seconds. The Transbond XT Primer adhesive was applied to the enamel surface, and the Transbond XT Light Cure Adhesive Paste composite to the bracket base. Excess removal and polymerization of the composite were performed as previously described for the experimental groups.
After bonding the brackets, all specimens were embedded in self‑curing PMMA (Orthocryl, Dentaurum GmbH & Co., Ipspringen, Germany), using steel cylinders (12‑mm high/13‑mm diameter) as casts for the acrylic. The sample was stored in distilled water at 37oC for 7 days, during which it was subjected to a new thermocycling process of 500 cycles in two distilled water baths at 5oC and 55oC.
Bond strength tests were performed using an Instron universal testing machine (model 4502, Instron Ltd., Bucks, UK) with a 1 kN load cell. Shear forces were applied to the brackets at a crosshead speed of 1 mm/min through a stainless‑steel loop placed under the gingival wings. The maximum forces at the moment of debonding were recorded in Newton (N) and divided by the bracket base�s nominal area, converting the values to MegaPascal (MPa).
The bases of the 105 brackets and their adhesion surfaces were examined with a stereomicroscope (Nikon SMZ‑2, Nikon Europe BV, P.O.B. 7609, The Netherlands) using a 20x magnification factor. The type of failure was scored between 0 and 3, according to the adhesive remnant index (ARI):23 Index 0 � 100% of adhesive remaining in the bracket base; Index 1 � mixed failure, with 50�100% of remaining adhesive on the bracket base; Index 2 � mixed failure, with 0�50% of remaining adhesive on the bracket base; Index 3 � 0% of adhesive remaining on the bracket base, corresponding to bracket‑adhesive interface failure. The presence of cohesive substrate failure (Yes / No) was also evaluated.
Statistical analysis was performed using Statview software (Abacus Concepts Inc., Berkeley, California, USA). The Shapiro‑Wilk test was used to assess normality in distribution, and the Levene test for homogeneity of variance. The adhesive strength values obtained in the experimental groups were evaluated by a two‑way analysis of variance (ANOVA), using the surface treatment and the adhesive system as independent variables. Comparisons between groups were performed with post‑hoc tests by the Student‑Newman‑Keuls method.
The control group and the experimental groups were compared with a one‑way ANOVA, using the combination surface treatment/adhesive system as a variable, followed by post‑hoc testing by the Dunnett method. The level of statistical significance was set at 5%.
Failure type (ARI) was subjected to a nonparametric analysis using the Kruskal‑Wallis and Mann‑Whitney U tests. Cohesive substrate failure was analyzed using chi‑squared tests.
Results
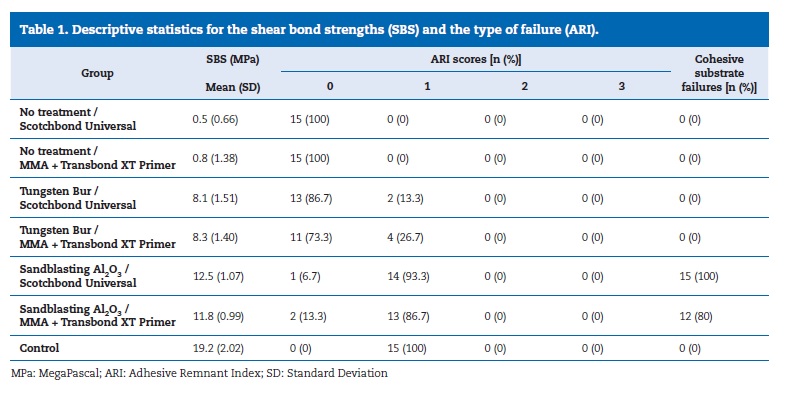
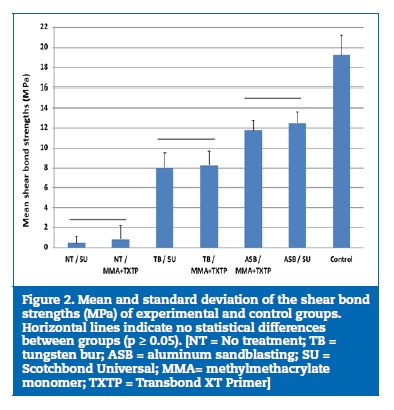
In the experimental groups, the mean shear bond strengths (Table 1 and Figure 2) ranged from 0.5 MPa (no treatment/Scotchbond Universal) to 12.5 MPa (ASB/Scotchbond Universal).
�
�
�
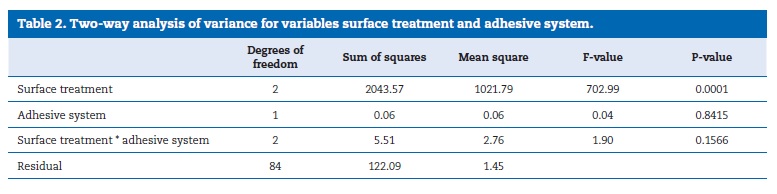
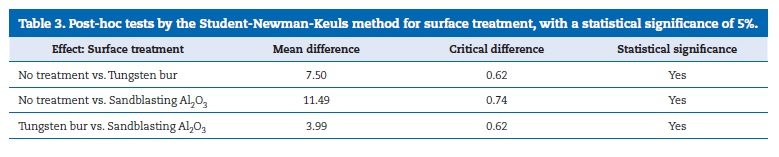
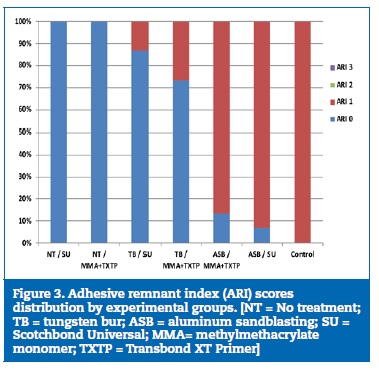
Surface treatment (Table 2) significantly influenced adhesion (p = 0.0001), with the ASB achieving values significantly higher than the other treatments (Table 3). There was no significant difference between the adhesive systems (p = 0.8415) and no significant interaction between the surface treatment and the adhesive system (p = 0.1566). The mean adhesion in the control group was 19.2 �} 2.02 MPa, while all surface treatment/adhesive system combinations of the experimental groups were significantly lower than the control (p = 0.1566). Failure type distribution is shown in Table 1 and Figure 3.
�
�
�
�
In the control group, 100% of the failures were classified as ARI 1. This index was also predominant in the groups submitted to ASB, with no significant difference from the control. The ARI 0 score was observed in 100% of specimens without mechanical treatment and in 80% of specimens subjected to TB abrasion.
None of the groups presented fractures at the adhesive‑bracket interface. Cohesive substrate failures were observed exclusively in the ASB‑treated groups, affecting 80�100% of these specimens (Table 1).
Discussion
The present study arose from the need to investigate orthodontic brackets� adhesion to PMMA since previous research and clinical practice point to a lower than clinically acceptable adhesive resistance.2, 14 Although there is no determined value for clinical bracket bond failure,24 many studies cite Reynolds�s suggestion,25 which considered tensile strengths between 5.9 and 7.8 MPa as adequate for orthodontic needs.
However, like the most recent studies, the present investigation evaluated shear rather than tensile strengths, as suggested by Reynolds.
Aging PMMA discs in water stored at 37oC for 55 days reduces the amount of free residual monomer, complicating adhesion.26 Additionally, all samples were thermocycled, which is another factor that reduces bond strength.6, 27 Both these procedures simulate what happens in the oral environment when temporary crowns have been cemented for some time. Although 500 is the number of cycles estimated to occur in less than 2 months in the mouth, in this study, it was chosen following the 1994 ISO/TR 11405,28 since there is still no standardized protocol in the literature for thermal cycling.29
By bonding brackets to PMMA using a Bis‑GMA resin, such as Transbond XT, materials with different chemical compositions are used, and consequently, adhesion forces are expected to diminish. Since these experimental conditions were the most adverse from the adhesion point of view, bond strength was expected to be significantly lower than in the control group. Mechanical surface treatment was the only factor that significantly influenced the adhesion of brackets to PMMA. This result agrees with other studies, which have shown that surface roughening, by increasing the area available for retention, increases the adhesion of acrylic resins to other materials.30, 31
In this study, ASB was the most effective surface treatment, being significantly superior to TB. No study evaluating bond strength after PMMA abrasion with a TB was found. However, a previous report32 found that aluminum oxide blasting of polycarbonate crowns before bracket bonding yielded higher adhesion values than those obtained when diamond‑bur abrasion was performed. Scanning electron microscopy studies6, 31 have also shown that the apparent roughness of diamond‑bur or green‑stone abrasion surfaces is only due to the presence of shallow ridges. By contrast, ASB creates thousands of microscopic retentions, resulting in a significantly more retentive surface.6
It is important to notice that the adhesion values in PMMA specimens submitted to ASB appear to have reached the material�s cohesive limit since most blasted discs presented cohesive substrate failures. No specimens from the remaining groups suffered a substrate failure. This observation has important clinical implications, particularly during the removal of brackets bonded to sandblasted PMMA temporary crowns, as the risk of crown fracture is considerable.
The literature is inconclusive regarding the effects of applying the MMA monomer to PMMA surfaces and its effective application time. Several exposure times to MMA have been proposed, from 15 to 6035 stated that, with a 180‑second application, MMA dissolves the surface structure of PMMA, increasing its potential for chemical adhesion. According to other researchers,37 the surface of dissolved PMMA provides free bonds that can copolymerize with composite resin. The polymerization process of MMA and composite matrix (Bis‑GMA) follows a similar pattern of activation and cross‑linking since the molecules� reactive methacrylate groups are similar. Thus, chemical adhesion could occur. However, this study�s results showed that the tested adhesive systems do not ensure clinically effective PMMA bracket adhesion, even when applying MMA for 25 seconds. In the absence of mechanical surface treatment, adhesion was very weak for both adhesive systems, suggesting that neither could achieve a chemical bond between the composite and the PMMA. No differences were found between adhesive systems, a result that was similar to a previous study using PMMA and sandblasting treatment.38
Regarding the type of failure, ARI 1, which corresponds to the largest amount of adhesive on the bracket base, was predominant in the groups submitted to sandblasting; this is in line with a previous report.22 However, another study14 found more ARI 0 failures when using this treatment. In the groups without mechanical treatment, 100% ARI 0 failures were observed; these correspond to the acrylic‑adhesive interface�s failure, with all the adhesive at the base of the bracket. In the groups with TB abrasion, the ARI 0 failures predominated, suggesting a lack of effectiveness of this treatment in obtaining a sufficiently retentive surface. The same researchers14 found that abrasion with a green stone also resulted mainly in ARI 0 failures. In vitro adhesion studies have as a limitation the impossibility of reproducing in the laboratory the conditions that occur in the individual�s mouth. In the oral environment, brackets are subject to different temperatures, degrees of humidity, and forces acting in various directions.39 Although thermocycling and shear tests simulate these conditions, in vitro values cannot be extrapolated to the clinical practice. Future studies are necessary to investigate simple methods of bonding brackets to PMMA crowns that ensure effective adhesion during the orthodontic treatment, as well as safety during debonding.
Conclusions
According to the objectives of this study, it can be concluded that bracket adhesion to PMMA was lower than adhesion to enamel. Surface treatment significantly increased bracket adhesion to PMMA, with ASB achieving better results than TB abrasion. The MMA monomer and the Scotchbond Universal Adhesive showed comparable bond strength to PMMA.
Overall, the weakest adhesive link was found at the acrylic‑adhesive interface, and the cohesive failures observed were associated with surface treatment with ASB.
�
Acknowledgements. The authors thank ORMCO, 3M, and Ivoclar Vivadent for the donation of products used in the study.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflict of interest. The authors have no conflicts of interest to declare.
�
References
1. Kokich VG, Spear FM. Guidelines for managing the orthodontic‑restorative patient. Semin Orthod. 1997;3:3-20.
2. Al Jabbari YS, Al Taweel SM, Al Rifaiy M, Alqahtani MQ, Koutsoukis T, Zinelis S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 2014;84:649-55.
3. Buyukyilmaz T, Zachrisson YO, Zachrisson BU. Improving orthodontic bonding to gold alloy. Am J Orthod Dentofacial Orthop. 1995;108:510‑8.
4. Zachrisson BU, Buyukyilmaz T, Zachrisson YO. Improving orthodontic bonding to silver amalgam. Angle Orthod. 1995;65:35‑42.
5. Zachrisson YO, Zachrisson BU, Buyukyilmaz T. Surface preparation for orthodontic bonding to porcelain. Am J Orthod
6. Jardim L. Estudo da adesao de bracketsortodonticos a materiais dentarios restauradores. Tese de Doutoramento, 1998, Universidade de Lisboa.
7. Zachrisson BU. Orthodontic bonding to artificial tooth surfaces: clinical versus laboratory findings. Am J Orthod Dentofacial Orthop. 2000;117:592‑4.
8. Abu Alhaija ES, Al‑Wahadni AM. Shear bond strength of orthodontic brackets bonded to different ceramic surfaces. Eur J Orthod. 2007;29:386‑9.
9. Goymen M, Topcuoglu T, Topcuoglu S, Akin H. Effect of different temporary crown materials and surface roughening methods on the shear bond strengths of orthodontic brackets. Photomed Laser Surg. 2015;33:55‑60.
10. Burns DR, Beck DA, Nelson SK. A review of selected dental literature on contemporary provisional fixed prosthodontics treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003;90:474‑97.
11. Balkenhol M, Ferger P, Mautner MC, Wostmann B. Provisional crown and fixed partial denture materials: Mechanical properties and degree of conversion. Dent Mater. 2007;23:1574‑83.
12. Christensen GJ. The fastest and best provisional restorations. J Am Dent Assoc. 2003;134:637‑9.
13. Mizrahi B. Temporary restorations: the key to success. Alpha Omegan. 2007;100:80‑4.
14. Chay SH, Wong SL, Mohamed N, Chia A, Yap A. Effects of surface treatment and aging on the bond strength of orthodontic brackets to provisional materials. Am J Orthod�� Dentofacial Orthop. 2007;132:e7‑e11.
15. Amaral M, Belli R, Cesar PF, Valandro LF, Petschelt A, Lohbauer U. The potential of novel primers and universal adhesives to bond to zirconia. J Dent. 2014;42:90‑8.
16. Isolan C, Valente L, Munchow E, Basso G, Pimentel A, Schwantz J, Silva A, Moraes R. Bond strength of a universal bonding agent and other contemporary dental adhesives applied on enamel, dentin, composite, and porcelain. Applied Adhesion Science. 2014;2:25.17. Pongprueksa P, Miletic V, De Munck J, Brooks NR, Meersman F, Nies E, Van Meerbeek B, Van Landuyt KL. Effect of evaporation on the shelf life of a universal adhesive. Oper Dent. 2014;39:500‑7.18. Chen C, Niu LN, Xie H, Zhang ZY, Zhou LQ, Jiao K, Chen JH, Pashley DH, Tay FR. Bonding of universal adhesives to dentine � Old wine in new bottles? J Dent. 2015;43:525‑36.19. Rambhia S, Heshmati R, Dhuru V, Iacopino A. Shear bond strength of orthodontic brackets bonded to provisional crown materials utilizing two different adhesives. Angle Orthod. 2009;79:784‑9.
20. Maryanchik I, Brendlinger EJ, Fallis DW, Vandewalle KS. Shear bond strength of orthodontic brackets bonded to various esthetic pontic materials. Am J Orthod Dentofacial Orthop. 2010;137:684‑9.
21. Almeida JX, Depra MB, Marquezan M, Retamoso LB, Tanaka O. Effects of surface treatment of provisional crowns on the shear bond strength of brackets. Dental Press J Orthod. 2013;18:29‑34.
22. International Standards Organization. Dental materials � Testing of adhesion to tooth structure. ISO/TS 11405:2003(E)
23. Artun J, Bergland S. Clinical trials with crystal growth conditioning as an alternative to acid‑ etch enamel pretreatment. Am J Orthod. 1984;85:333‑40.
24. Yamada R, Hayakawa T, Kasai K. Effect of using self‑etching primer for bonding orthodontic brackets. Angle Orthod. 2002;72:558‑64.
25. Reynolds I. A review of direct orthodontic bonding. Br J Orthod. 1975;18:171‑8.
26. Vallittu PK, Miettinen V, Alakuijala P. Residual monomer content and its release into water from denture base materials. Dent Mater. 1995;11:338‑42.
27. Saavedra G, Valandro LF, Leite FP, Amaral R, Ozcan M, Bottino MA, Kimpara ET. Bond strength of acrylic teeth to denture base resin after various surface conditioning methods before and after thermocycling. Int J Prosthodont. 2007;20:199‑201. PMID: 17455445
28. International Standards Organization. Dental materials � Guidance on testing of adhesion to tooth structure. ISO/TR11405:1994(E).
29. Morresi AL, D�Amario M, Capogreco M, Gatto R, Marzo G, D�Arcangelo C, Monaco A. Thermal cycling for restorative materials: does a standardized protocol exist in laboratory testing? A literature review. J Mech Behav Biomed Mater. 2014;29:295‑308.
30. Shen C, Colaizzi FA, Birns B. Strength of denture repairs as influenced by surface treatment. J Prosthet Dent. 1984;52:844‑8.
31. Bragaglia LE, Prates LH, Calvo MC. The role of surface treatments on the bond between acrylic denture base and teeth. Braz Dent J. 2009;20:156‑61.
32. Blakey R, Mah J. Effects of surface conditioning on the shear bond strength of orthodontic brackets bonded to temporary polycarbonate crowns. Am J Orthod Dentofacial Orthop. 2010;138:72‑8.
33. Chung RW, Clark RK, Darvell BW. The bonding of cold‑cured acrylic resin to acrylic denture teeth. Aust Dent J. 1995;40:241‑5.
34. Kawara M, Carter JM, Ogle RE, Johnson RR. Bonding of plastic teeth to denture base resins. J Prosthet Dent. 1991;66:566‑71.
35. Vallittu PK, Lassila VP, Lappalainen R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat‑polymerized resin. J Prosthet Dent. 1994;72:639‑43.
36. Papazoglou E, Vasilas AI. Shear bond strengths for composite and autopolymerized acrylic resins bonded to acrylic resin denture teeth. J Prosthet Dent. 1999;82:573‑8.
37. Chatterjee N, Gupta TK, Banerjee A. A Study on Effect of Surface Treatments on the Shear Bond Strength between Composite Resin and Acrylic Resin Denture Teeth. J Indian Prosthodont Soc. 2011;11:20‑5.
38. Rosca B, Ramalho S, Sampaio‑ Fernandes JC, Portugal J. Reparability of two different CAD/CAM polymer materials using a light‑cured composite and universal adhesives. Rev Port Estomatol Med Dent Cir Maxilofac. 2016;57:189‑ 96.
39. Littlewood SJ, Mitchell L, Greenwood DC, Bubb NL, Wood DJ. Investigation of a hydrophilic primer for orthodontic bonding: an in vitro study. J Orthod. 2000;27:181‑6
�
Rita Matos Cardoso
E-mail address: rita.matoscardoso@gmail.com
