
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (1) | 44-48
Case report
Non-surgical management of bilateral mandibular condyle fracture: Six-year follow-up. A case report
Tratamento não-cirúrgico de fratura bilateral de côndilo mandibular: Seis anos de acompanhamento
a Oral and Maxillofacial Surgery and Traumatology, University of Sagrado Coração, Bauru, SP, Brazil
b Stricto Sensu Post-graduate Program in Dentistry with Concentration Area Implantology, Latin American Institute for Research and Dental Education (ILAPEO), Curitiba, PR, Brazil
Gabriel Lucio Calazans Duarte - gabriel7duarte@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 1
Case report
Pages - 44-48
Go to Volume
Article History
Received on 08/11/2017
Accepted on 10/05/2018
Available Online on 30/05/2018
Keywords
Case report
�
Non-surgical management of bilateral mandibular condyle fracture: Six-year follow-up. A case report
Tratamento n�o-cir�rgico de fraturabilateral de c�ndilo mandibular: Seis anos de acompanhamento
�
Paulo Domingos Ribeiro-Juniora, Luis Eduardo Marques Padovanb, NatairaRegina Momessoa, Gabriel LucioCalazans Duartea,*, Ana Carolina Fichoa
a Oral and Maxillofacial Surgery and Traumatology, University of SagradoCora��o, Bauru, SP, Brazil.
b StrictoSensuPost-graduate Program in Dentistry with Concentration Area Implantology, Latin American Institute for Research and Dental Education (ILAPEO), Curitiba, PR, Brazil
�
�
http://doi.org/10.24873/j.rpemd.2018.05.215
�
Abstract
The mandibular condyle is the area most frequently affected by mandibular fractures. These fractures may be treated non-surgically, with closed reduction, or with open reduction and fixation with miniplatesand screws. This study reports the treatment selected for a patient affected by three mandibular fractures: a symphysealfracture and two bilateral subcondylarfractures after facial trauma. The mandibular symphysealfracture was treated with open reduction and internal fixation. The subcondylarfractures were treated non-surgically.
Keywords: Conservative management, Mandibular condyles, Mandibular fracture
�
Resumo
O c�ndilo mandibular � a �rea mais frequentemente afetada em fraturasmandibulares. O tratamento destas fraturaspode ser n�o cir�rgico, atrav�s da redu��o fechada, ou por redu��o aberta e fixa��o com mini-placas e parafusos. Este estudo relata o tratamento seleccionado para uma paciente com tr�s fraturasmandibulares, sendo uma fraturaem regi�o de s�nfise mandibular e as outras fraturasnas regi�es subcondilares bilateralmente ap�s trauma facial. A fraturade s�nfise foi tratada com redu��o aberta e osteoss�ntese. J� as fraturassubcondilares foram tratadas pelo m�todo n�o-cir�rgico.
Palavras-chave: Tratamento conservador, C�ndilo mandibular, Fraturamandibular
�
Introduction
The mandibular condyle (MC) is the area most frequently affected by mandibular fractures.1 Themost common etiologies of this type of fracture are interpersonal violence, accidents with motor vehicles and falls. Frequently, one of the most affected bones in facial trauma is the mandible, and 25-40% of mandibular fractures involve the condyle.2
Malocclusion, open bite, swelling, tenderness over the joint, loss of mandibular function, deviation of the chin, crepitus and laceration of the skin of the chin are clinical signs of this type of fracture.3
The treatment of mandibular condylar fractures depends on their extension, which may be unilateral or bilateral, the level of the fracture (condylar head, condylar neck or subcondylarfractures) and the degree of displacement3. The treatment of these fractures may be conservative, with closed reduction, or with open reduction and fixation with miniplatesand screws. Some complications may occur after open reduction, such as paresthesiaor paralysis of the facial nerve, infections, dysfunction of the auriculotemporal nerve, Frey syndrome and unsightly scars.4 On the other hand, the conservative or non-surgical treatment usually does not lead to such complications and has been effectively performed with good functional and esthetic outcomes.5
The aim of this study is to report the treatment selected for a patient affected by three mandibular fractures: two bilateral subcondylar fractures and a symphysealfracture.
Case Report
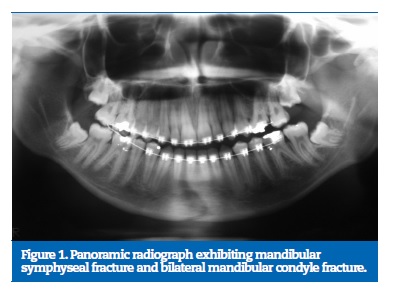
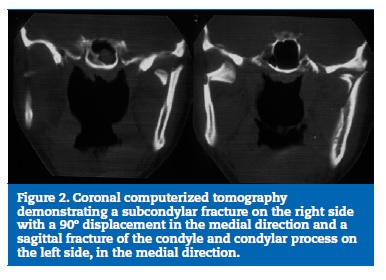
The patient was a victim of a motorcycle accident and presented with polytrauma affecting the face. Clinical examination revealed a contused lacerated wound on the chin area, bilateral preauricularedema, bone crepitation, and preservation of mandibular movements yet limited by pain. Image exams exhibited a mandibular fracture on the chin area, a subcondylarfracture on the right side and a sagittal fracture of the condyle and condylar process on the left side, both medially displaced (Figures 1 and 2).
�
�
�
Initially, the symphysealfracture was temporarily stabilized by tooth synthesis. After five days, transoperativeintermaxillaryfixation (IMF) and surgical reduction and fixation of the symphysealfracture were performed with miniplatesand screws of the 2.0-mm system by intraoral access; the bilateral subcondylarfractures were conservatively treated.
The patient was kept without IMF for 24 hours. After this period wearing the orthodontic appliance and tooth syntheses, two rubber appliances with nearly 5-mm height were placed on the posterior occlusalregion bilaterally, and IMF was performed with elastics involving primarily the anterior teeth. This fixation associated with posterior support was kept for two days.
After this period, the patient returned to the dentist�s office and the posterior support was removed. The intermaxillaryfixation with elastics was kept for seven days further.
After removal of the intermaxillaryfixation, the patient was referred to postoperative physiotherapy, including opening, bilateral laterality and protrusion exercises, of which the last two were performed with the help of manual force. The number of repetitions of the exercises was 40 times for opening, 20 times for laterality for each side and 20 times for protrusion. Physiotherapy was performed for 90 days.
The patient presented satisfactory postoperative evolution.
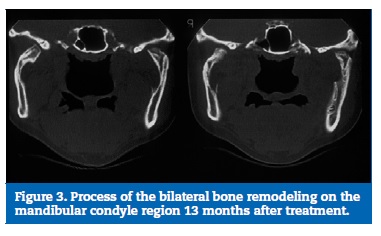
A new CT scan obtained at 13 months postoperatively revealed remodeling of the mandibular condyles to reach the ideal position in the mandibular fossa (Figure 3).
�
�
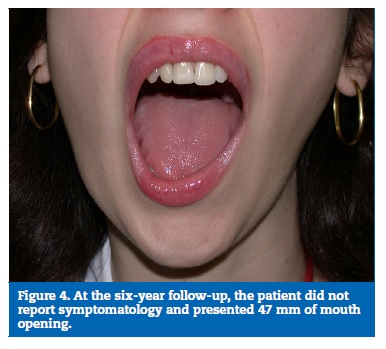
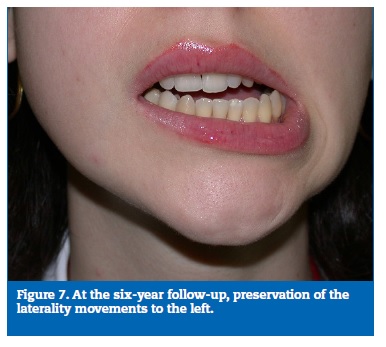
At the six-year follow-up, the patient did not report symptomatology, presented 47mm of mouth opening and preservation of laterality and protrusion movements (Figures 4, 5, 6 and 7).�
�

�

�
�
Discussion
The treatment options for MC fractures are quite controversial in the literature. It is believed that the particularities and functional and aesthetic characteristics of each case should be evaluated before the treatment is selected. The procedures used during the closed treatment of condylar fractures are not adequately described in the literature. There is no consensus when it comes to indications, treatment protocols, and lengths of treatment.6 Conservative treatment isprofitable and scientifically grounded. It may be performed using intermaxillaryfixation modalities (arch bars, interdental wirings or orthodontic appliance).7
Several studies have grouped precise clinical indications for the surgical management of MC fractures. An author reported two clinical indications for open treatment, namely condylar displacement laterally or superiorly to the zygomatic arch and condylar intrusion into the cranial fossa. 8, 13
The authors of a study compared the mandibular and facial symmetry of 146 patients with condylar fractures after undergoing conservative treatment with reduction and surgical fixation of the fracture. They concluded that patients treated with the conservative approach developed asymmetries characterized by a reduction in posterior facial height on the affected side, which may result from an attempt to reestablish the new position of the temporomandibularjoint. However, some patients did not notice this asymmetry.9
In another study with 20 patients with subcondylarfractures,10were submitted to conservative treatment and 10 to the surgical approach. After a six-month follow-up, the authors did not observe statistically significant differences between groups regarding mouth opening, laterality and protrusion movements, deviation in mouth opening and occlusion5, and pain in the TMJ.10 These results are consistent with the present case report.
A study that compared performing the open reduction with internal fixation with the closed reduction for the management of a unilateral displaced subcondylar and condylar neck fracture in 50 patients found no clinical differences in terms of functional movements and pain in the temporomandibular joints.3
The conservative treatment of MC fractures may involve absolute rest of the joint by following a liquid diet, and may be performed by intermaxillary fixation for 7 to 14 days or by intermaxillary fixation with posterior support for 12 to 48 hours followed by conventional intermaxillaryfixation. 11
Researchers observed some differences, even if statistically irrelevant, between the surgical and conservative treatments when evaluating mouth opening. These differences were probably due to the surgical trauma, which may be an additional factor for mouth opening restriction.12
In a comparative study of treatments with open and closed reduction with a follow-up period of six months, the angulation and height of the mandibular branch improved in both groups. This result was probably due to the influence of the functional forces, and no statistical differences with respect to the angulation and height of the mandibular branch were found. Occlusalalterations can be recovered if appropriate care is taken.10
The treatment option for condylar fractures should allow the least morbidity with stable and predictable functional and esthetic outcomes. The clinical evaluation of mandibular movements and type of displacement are the most important parameters for this decision. During initial planning for conservative treatment, if the occlusion between the arches is not ideal, the most indicated treatment would be an open reduction with internal fixation. In the present case report, despite the displacement observed in image exams, this displacement occurred in a medial direction, and the clinical signs of the patient did not allow a surgical management.
Conclusion
Based on the present case report, it can be concluded that non-surgical treatment may be adequate even in cases of severe bone displacement of MC fractures, especially if the mandibular function is preserved.
�
Refer�ncias
1. OlsonRA, Fonseca RJ, Zeitler DL, OsbonDB. Fractures of the Mandible: A Review of 580 Cases. J Oral MaxillofacSurg. 1982;40(1):23-8.
2. De RiuG, GambaU, AnghinoniM, SesennaE. A comparison of open and closed treatment of condylar fractures: A change in philosophy. IntJ Oral Maxillofac Surg. 2001;30(5):384-9.
3. ShijuM, RastogiS, GuptaP, KukrejaS, Thomas R, BhugraAK, etal. Fractures of the mandibular condyle � openversus closed � a treatment dilemma. J CraniomaxillofacialSurg. 2015;43(4):448-51.
4. Ellis E, McFadden D, Simon P, Throckmorton G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58(9):950-8.
5. HaugRH, AssaelLA. Outcomes of open versus closed treatment of mandibular subcondylar fractures. J Oral MaxillofacSurg. 2001;59(4):370-5.
6. RozeboomAVJ, Dubois L, BosRRM, SpijkerR, de Lange J. Closed treatment of unilateral mandibular condyle fractures in adults: a systematic review, IntJ Oral MaxillofacSurg. 2016;46(4):456-64.
7. Van den Bergh B, BlankestijnJ, Van der Ploeg T, TuinzingDB, Forouzanfar DB, Conservative treatment of a mandibular condyle fracture: Comparing intermaxillaryfixation with screws or arch bar. A randomisedclinical trial, J Craniomaxillofacial Surg. 2015;43(5):671-76
8. ZideMF. Outcomes of open versus closed treatment of mandibular subcondylarfractures. J Oral Maxillofac Surg. 2001;59(4):375-6.
9. Ellis E, Throckmorton G. Facial Symmetry AfterClosed and Open Treatment of Fractures of the Mandibular Condylar Process. J Oral MaxillofacSurg. 2000;58(7):719-28.
10. RastogiS, Sharma S, Kumar S, Reddy MP. Fracture of mandibular condyle � to open or not open: an attempt to settle the controversy. Oral SurgOral Med Oral PatholOral RadiolEndod.2015;119(6):608-13.
11. Rowe NL. Fractures of the jaws in children.J Oral Surg. 1969;27(7):497-507.
12. MonnazziMS, GabrielliMAC, GabrielliMFR, TrivellatoAE. Treatment of mandibular condyle fractures. A 20-year review.Dent Traumatol. 2017;33(3):175-80.
13. ZideF, Kent JN. Indications for Open Reduction of Mandibular Condyle Fractures.J Oral Maxillofac Surg. 1983;41:89-98.
�
Gabriel LucioCalazans Duarte
E-mail address: gabriel7duarte@gmail.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article
�
Conflicts of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 8 November 2017
Accepted 10 May 2018
Available online 22 May 2018
