
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 85-90
Case report
Occlusive denture for the management of medication-related osteonecrosis of the jaw with oronasal communication: A case report
Prótese obturadora no manuseamento da osteonecrose dos maxilares relacionada com medicamentos e comunicação oronasal: Caso clínico
a Dentistry School of Federal University of Uberlândia, Uberlândia, Minas Gerais, Brazil
Arthur Augusto Martins e Silva - arthur.amsilva@usp.br
Andréa Gomes de Oliveira - andrea.gomes@ufu.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Case report
Pages - 85-90
Go to Volume
Article History
Received on 11/06/2024
Accepted on 11/03/2025
Available Online on 30/05/2025
Keywords
Clinical Case Report
�
Occlusive denture for the management of medication-related osteonecrosis of the jaw with oronasal communication: A case report
Pr�tese obturadora no manuseamento da osteonecrose dos maxilares relacionada com medicamentos e comunica��o oronasal: Caso cl�nico
�
Arthur Augusto Martins e Silva1,* 0000-0003-2334-2989
Andr�a Gomes de Oliveira1,*000-0002-2737-1843
1 Dentistry School of Federal University of Uberl�ndia, Uberl�ndia, Minas Gerais, Brazil
�
�
Article history:
Received 11 June 2024
Accepted 11 March 2025
Available online 28 May 2025
�
Abstract
Medication-related osteonecrosis of the jaw (MRONJ) is a complex condition often associated with bisphosphonates, such as zoledronic acid, affecting patients with osteolytic diseases like multiple myeloma. This case report presents the use of an occlusive denture with a soft liner for managing MRONJ in a patient with oronasal communication. Na 81-year-old female patient with multiple myeloma was diagnosed with MRONJ, which led to significant oronasal communication, after two years of zoledronic acid treatment. She was referred for oral rehabilitation. Due to limited prior documentation and challenges with follow-up appointments, a conservative treatment approach was chosen. The patient received an occlusive upper complete denture with a soft liner to minimize mucosal trauma, restore stomatognathic functions, and enhance comfort. Follow-up evaluations at 30 days, 9 months, and 16 months showed significant improvements in the inflammatory process and a reduction in exposed necrotic bone. While research on soft liner-coated dentures for MRONJ is limited, this approach proved beneficial for the patient by reducing discomfort and promoting mucosal healing. The findings suggest that occlusive dentures with soft liners could be a viable treatment option in MRONJ cases, especially when other treatment options are not feasible. Further studies are needed to validate this approach and establish consistent guidelines for its use.
Keywords: Bisphosphonate-associated osteonecrosis of the jaw; Complete denture;Denture liners; Mouth rehabilitation; Multiple myelom;Osteonecrosis
�
Resumo
A osteonecrose dos maxilares relacionada com medicamentos (ONMRM) � uma condi��o complexa frequentemente associada ao uso de bifosfonatos, como o �cido zoledr�nico, e afeta pacientes com doen�as osteol�ticas, como o mieloma m�ltiplo. Este caso cl�nico apresenta o uso de uma pr�tese obturadora com rebasamento macio no tratamento da ONMRM numa paciente com comunica��o oronasal. Uma paciente feminina de 81 anos, com mieloma m�ltiplo, foi diagnosticada com ONMRM, que provocou uma comunica��o oronasal significativa, ap�s dois anos de tratamento com �cido zoledr�nico. A paciente foi encaminhada para reabilita��o oral. Devido � documenta��o pr�via limitada e dificuldades no seguimento, optou-se por uma abordagem conservadora. A paciente recebeu uma pr�tese total superior obturadora com rebasamento macio para minimizar o trauma mucoso, restaurar as fun��es estomatogn�ticas e melhorar o conforto. As avalia��es de acompanhamento realizadas aos 30 dias, 9 meses e 16 meses mostraram melhorias significativas no processo inflamat�rio e redu��o da exposi��o de osso necr�tico. Embora haja poucas investiga��es sobre pr�teses revestidas com rebasamentos macios para ONMR, esta abordagem mostrou-se ben�fica para a paciente, reduzindo o desconforto e promovendo a cicatriza��o da mucosa. Os achados sugerem que pr�teses obturadoras com rebasamento macio possam ser uma op��o vi�vel de tratamento em casos de ONMRM, especialmente quando outras op��es terap�uticas n�o s�o vi�veis. S�o necess�rios estudos adicionais para validar esta abordagem e estabelecer diretrizes consistentes para o seu uso.
Palavras-chave:Osteonecrose dos maxilares associada aos bifosfonatos; Pr�tese Total;Materiais de rebasamento; Reabilita��o oral; Mieloma M�ltiplo;Osteonecrose
�
Introduction
Medication-related osteonecrosis of the jaw (MRONJ) is a complex and challenging condition that affects patients undergoing treatment with medications such as bisphosphonates, denosumab, and, to a lesser extent, angiogenesis inhibitors.1, 2 These medications are widely used to manage osteolytic diseases, including osteoporosis, metastatic bone cancer, and multiple myeloma, due to their effectiveness in reducing bone resorption.3
Multiple myeloma is a malignant neoplasm characterized by the clonal proliferation of abnormal plasma cells within the bone marrow. These cells secrete monoclonal proteins and disrupt the normal hematopoietic environment, resulting in complications such as anemia, leukopenia, and thrombocytopenia.
Additionally, the interaction between myeloma cells and the bone marrow microenvironment stimulates osteoclast activity, leading to excessive bone resorption.4 Zoledronic acid, a powerful bisphosphonate, is a cornerstone in the management of multiple myeloma. It effectively inhibits osteoclast activity and reduces bone resorption.
However, its use is associated with an increased risk of MRONJ5 because it suppresses bone remodeling and hinders the healing of microtraumas in the jawbone, potentially leading to bone exposure and necrosis. Even minor trauma, such as that caused by poorly fitting dentures, can exacerbate the condition.6
Although bisphosphonates are highly effective in managing osteolytic diseases and preventing bone loss, their prolonged use requires careful monitoring. Bisphosphonates must be administered for limited periods to maximize their benefits for bone mass gain while minimizing the risks of adverse effects, such as fractures and MRONJ.3, 5 The literature suggests that bisphosphonates should not be used for longer than 3�5 years in the treatment of osteoporosis, and their prolonged use, especially in cancer patients, may require careful reevaluation to weigh the potential benefits against the risks.3, 5
The management of MRONJ requires a multidisciplinar approach, with treatment strategies ranging from conservative to surgical interventions, depending on the severity of the condition.
The initial management focuses on symptom control and prevention of lesion progression, often achieved through rigorous oral hygiene and the use of antiseptic mouthwashes, such as chlorhexidine, to reduce bacterial load. Systemic antibiotics and analgesics are commonly prescribed for pain and infection control. In more severe cases, surgical interventions, such as necrotic tissue resection and closure with mucosal flaps, may be necessary.7, 8 However, these treatments pose significant limitations, including the need to avoid invasive procedures like dental extractions and implants, which complicate dental management. These challenges underscore the importance of prevention, early diagnosis, and treatment planning to preserve the patient�s quality of life and minimize complications.4
In advanced cases, MRONJ may lead to oronasal communication, an abnormal connection between the oral and nasal cavities. This condition profoundly affects the patient�s quality of life, causing functional impairments such as difficulties with chewing, phonetics, and breathing, as well as aesthetic alterations that may affect facial appearance.9 Additionally, bone fragility and recurrent complications, including pain and further bone exposure, can hinder rehabilitation by reducing support areas, retention, and stability for prosthetic solutions.10
Since there is no gold-standard treatment for MRONJ, partly due to its poorly understood etiopathogenesis,3 and given the need to address oronasal communication,10 alternative therapeutic approaches must be explored. One approach involves using an occlusive denture with a soft liner coated to the denture base. The viscoelastic properties of soft liners help distribute chewing forces evenly, restore stomatognathic functions such as chewing and phonetics, and provide comfort. This material is particularly advantageous for patients with compromised basal structures. Since their first mention in 1869 as soft rubber and the subsequente introduction of silicone-based materials in 1958, soft liners have been recognized for their durability and improved mechanical properties, making them suitable for prosthetic rehabilitation.10, 11 By preventing inflammatory and traumatic processes related to poor denture fit and microtraumas, soft liners contribute to enhanced comfort and functional restorations.12
Despite these potential benefits, there are few studies on soft liner-coated dentures for patients with MRONJ, particularly those with oronasal communication. This report presents a clinical case where a patient with MRONJ and significant oronasal communication received an occlusive upper complete denture coated with a soft liner. The aim was to restore stomatognathic functions, including aesthetics, phonetics, and chewing, while ensuring comfort, protecting the affected area, and improving the patient�s overall quality of life.
Case report
An 81-year-old Caucasian female patient was diagnosed with MRONJ after complaining of pain in the maxillary ridge region for about six months, which was initially perceived as a mouth ulcer. She had been using her old, poorly fitting upper denture and had not received adequate management. Her MRONJ likely resulted from two years of continuous intravenous treatment with zoledronic acid (Zometa�, Novartis Bioci�ncias S.A., S�o Paulo, SP, Brazil), administered as part of her previous treatment for multiple myeloma, as reported by her family.
In November 2021, she was referred to the Dentistry School of the Federal University of Uberl�ndia (FOUFU) for appropriate treatment and oral rehabilitation after developing significant oronasal communication as a consequence of MRONJ. Unfortunately, detailed information regarding her prior diagnosis, management, treatments, medication dosages, and the exact start and end dates of her zoledronic acid use was unavailable. Additionally, no medical records, reports, or supporting documentation were provided upon her referral to FOUFU.
Given the limited information and the condition of her oral tissues, a non-invasive approach was chosen for the initial phase of treatment. It focused on oral rehabilitation to restore stomatognathic functions, eliminate trauma caused by chewing, and alleviate the patient�s discomfort.
This conservative approach also enabled the evaluation of the mucosal response, guiding potential future treatment decisions.
The patient resided outside Uberl�ndia and depended on family members for transportation, making it challenging to attend weekly appointments. The timing of her referral coincided with the year-end break, which further complicated immediate treatment initiation. Imaging exams were deferred to later treatment stages. Considering these factors, along with the patient�s report of experiencing no pain during the evaluation, a decision was made to fabricate an occlusive denture with a soft liner. This approach aimed to minimize mucosal trauma, enhance her quality of life, and allow condition monitoring until a routine care schedule with a specialized team could be established.
Following anamnesis and clinical examinations, the extent of basal structure loss, the depth of the oronasal communication, and the presence of exposed necrotic bone were assessed (Figure 1). The rehabilitation process adhered to conventional protocols for complete denture fabrication but included modifications to incorporate a soft liner (Ufi Gel P, VOCO GmbH, Porto Alegre, RS, Brazil) during the hydraulic pressing step, following the manufacturer�s instructions, aiming to enhance patient comfort (Figure 2).
�

Figure 1. Clinical condition of the oral cavity at the initial appointment.
�
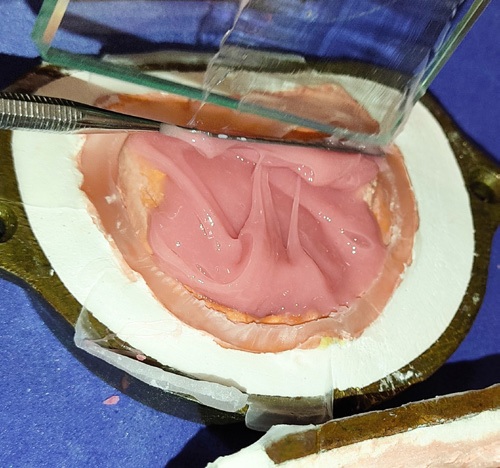
Figure 2. Application of the soft liner (Ufi Gel P, VOCO GmbH) to the denture base.
�
The occlusive denture was placed in April 2022. Figure 3 presents a preview of the unfinished denture. The healing process and mucosal appearance were documented during follow-up evaluations at 30 days, 9 months, and 16 months post-rehabilitation, based on the patient�s availability, as shown in Figures 4, 5, and 6, respectively.
�
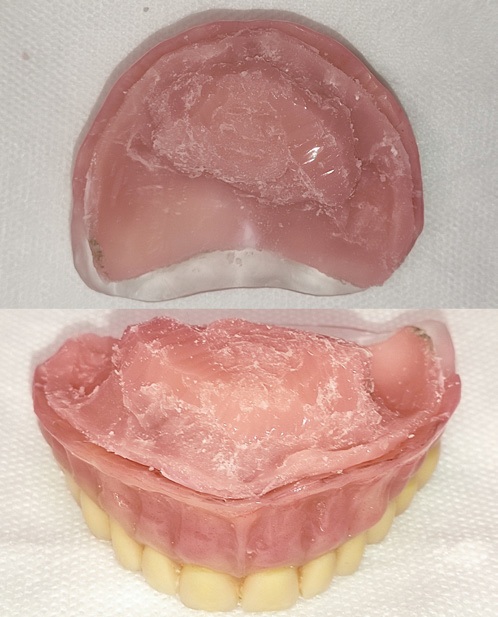
Figure 3. Denture after processing, prior to final finishing and installation.
�

Figure 4. Post-rehabilitation assessment: 30 days after denture installation.
�

Figure 5. Post-rehabilitation assessment: 9 months after denture installation.
�

Figure 6. Post-rehabilitation assessment: 16 months after denture installation.
�
Following prosthetic treatment, the patient expressed difficulties in maintaining weekly follow-up appointments due to travel constraints and decided to continue her care in her hometown. She received detailed instructions on proper denture use and care, oral hygiene practices, and the importance of maintaining regular follow-up appointments for the upkeep of the soft liner. She was also advised to return for evaluations whenever possible to ensure continued monitoring and optimal outcomes.
Discussion and Conclusions
Although the literature suggests treatment options such as laser therapy, hyperbaric oxygen, and ozone,13, 14 most people in Brazil rely on the public healthcare system for their medical and dental care. Therefore, proposing a more affordable treatment option provides valuable insights for oral rehabilitation and MRONJ management.15
In this case, managing the condition by fabricating na occlusive upper complete denture coated with a soft liner�a relatively straightforward procedure�led to a significant remission of the superficial inflammatory process. The substantial reduction in areas of exposed necrotic bone may be associated with the occlusive denture lined with the soft material. However, the direct effects of the soft liner cannot be scientifically verified due to the lack of research and case reports in this area. Nevertheless, the literature highlights the importance of using obturator prostheses to reduce mucosal trauma and support the progression of clinical conditions such as MRONJ.16
Although no specific examinations were conducted to scientifically validate these effects, the observed clinical improvements strongly suggest that this approach may play a pivotal role in reducing mucosal trauma, enhancing patient comfort, and promoting healing. These preliminary findings provide compelling evidence for the potential of occlusive dentures as a therapeutic tool for managing oronasal communication caused by MRONJ, emphasizing the need for further research on this topic.
The decision to use a soft liner was supported by findings that emphasizes its use with denture bases in cases requiring impact reduction or when addressing retention issues, exostosis, or sensitivity to acrylic resin. It has also been recommended for patients with malignant swelling in the oral cavity or in situations where trauma must be avoided to promote mucosal healing.17 - 19 Additionally, the literature indicates that, regardless of the polymerization method, relining with resiliente silicone-based materials is a viable alternative for improving patient quality of life and satisfaction, particularly for individuals facing challenges with conventional complete dentures.20 However, the literature reveals some controversy regarding the definitive indications for this type of material and the recommended maximum duration of use,17, 21 underscoring the need for further research to establish more consistente guidelines.
We conclude that successful oral rehabilitation was achieved by fabricating an occlusive upper complete denture coated with a soft liner. This approach effectively restored stomatognathic system functions, including chewing, aesthetics, and phonetics, significantly enhancing the patient�s Comfort and well-being, as reported during follow-up appointments.
Additionally, we observed a substantial reduction in inflammatory processes on the mucosal surface, suggesting a promising avenue for further exploration and in-depth study, particularly in cases where other treatments for MRONJ are not feasible.
�
References
1. Shibahara T. Antiresorptive Agent-Related Osteonecrosis of the Jaw (ARONJ): A Twist of Fate in the Bone. Tohoku J Exp Med. 2019;247:75�86.
2. Brijs K, Miclotte I, Vermeire S, Darche V, Politis C. Osteonecrosis of the jaw in patients with inflammatory bowel disease treated with tumour necrosis factor alfa inhibitors. Int J Oral Maxillofac Surg. 2020;49:317�24.
3. Nogueira D, Caldas IM, Dinis-Oliveira RJ. Bisphosphonates and osteonecrosis of the jaws: Clinical and forensic aspects. Arch Oral Biol. 2023;155:105792.
4. Cowan AJ, Green DJ, Kwok M, Lee S, Coffey DG, Holmberg LA, et al. Diagnosis and Management of Multiple Myeloma: A Review. JAMA. 2022;327:464�77.
5. Morgan GJ, Child JA, Gregory WM, Szubert AJ, Cocks K, Bell SE, et al. Effects of zoledronic acid versus clodronic acid on skeletal morbidity in patients with newly diagnosed multiple myeloma (MRC Myeloma IX): secondary outcomes from a randomised controlled trial. Lancet Oncol. 2011;12:743�52.
6. Bullock G, Miller CA, McKechnie A, Hearnden V. A Review Into the Effects of Pamidronic Acid and Zoledronic Acid on the Oral Mucosa in Medication-Related Osteonecrosis of the Jaw. Front Oral Health. 2022;2:822411.
7. Otto S, Pautke C, Van den Wyngaert T, Niepel D, Schi�dt M. Medication-related osteonecrosis of the jaw: Prevention, diagnosis and management in patients with cancer and bon� metastases. Cancer Treat Rev. 2018;69:177�87.
8. Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D. American Association of Oral and Maxillofacial Surgeons� Position Paper on Medication-Related Osteonecrosis of the Jaws-2022 Update. J Oral Maxillofac Surg. 2022;80:920�43.
9. Esen A, Akkulah S. Management of Large Oroantral Fistulas Caused by Medication-Related Osteonecrosis with the Combined Sequestrectomy, Buccal Fat Pad Flap and Platelet-Rich Fibrin. J Maxillofac Oral Surg. 2021;20:76�82.
10. Troeltzsch M, Probst F, Troeltzsch M, Ehrenfeld M, Otto S. Conservative management of medication-related osteonecrosis of the maxilla with an obturator prosthesis. J Prosthet Dent. 2015;113:236�41.
11. Goiato MC, Guiotti AM, Ribeiro PP, Santos DM, Antenucci RMF. Materiais reembasadores: estudo da deforma��o inicial, permanente e porosidade. Cienc Odontol Bras. 2007;10;44-52.
12. Neville BW, Damm DD, Allen CM, Chi AC editors. Oral and Maxillofacial Pathology. 4th ed. St. Louis :Elsevier, 2016.
13. Laputkov� G, Talian I, Schwartzov� V. Medication-Related Osteonecrosis of the Jaw: A Systematic Review and a Bioinformatic Analysis. Int J Mol Sci. 2023;24:16745.
14. Goker F, Grecchi E, Grecchi F, Francetti L, Del Fabbro M. Treatment of medication-related osteonecrosis of the jaw (MRONJ). A systematic review. Eur Rev Med Pharmacol Sci. 2021;25:2662�73.
15. Lima-Costa MF, de Andrade FB, de Souza Jr PRB, Neri AL, Duarte YAO, Castro-Costa E, et al. The Brazilian Longitudinal Study of Aging (ELSI-Brazil): Objectives and Design. Am J Epidemiol. 2018;187:1345�53.
16. Ali IE, Sumita Y. Medication-related osteonecrosis of the jaw: Prosthodontic considerations. Jpn Dent Sci Rev. 2022;58:9�12.
17. Palla ES, Karaoglani E, Naka O, Anastassiadou V. Soft denture liners� effect on the masticatory function in patients wearing complete dentures: A systematic review. J Dent. 2015;43:1403�10.
18. Ortman HR. Discussion of �impact reduction in complete and partial dentures, a pilot study.� J Prosthet Dent. 1966;16:246�50.
19. Griem ML, Robinson Jr JE, Barnhart GW. The Use of a Soft Denture-Base Material in the Management of the Post- Radiation Denture Problem. Radiology. 1964;82:320�1.
20. Goiato MC, S�nego MV, Gonfiantini AF, Santos DM. Satisfa��o e qualidade de vida em pacientes desdentados ap�s reembasamento com material resiliente. Rev Odontol Ara�atuba. 2018;39:28-32.
21. Shinde J, Mowade T, Gupta P, Tekale R, Pande N, Deshmukh K, et al. Satisfaction in conventional acrylic complete denture patient with and without denture liners - a systematic review. Pan Afr Med J. 2022;42:296.
�
Arthur Augusto Martins e Silva
E-mail address: arthur.amsilva@usp.br
Andr�a Gomes de Oliveira
E-mail address:�andrea.gomes@ufu.br
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Arthur Augusto Martins e Silva: Conceptualization, Investigation, Methodology, Writing � original draft, Writing � review & editing. Andr�a Gomes de Oliveira: Conceptualization, Project administration, Supervision, Writing � review & editing.
�
� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria.
Published by SPEMD. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
