
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 78-84
Case report
Effect of diode laser frenectomy on tongue anatomy and function – Clinical cases
Efeito na anatomia e função da língua após frenectomia a laser díodo – Casos clínicos
a Faculdade de Ciências da Saúde (FCS-UFP), Universidade Fernando Pessoa, Porto, Portugal
b Instituto de Investigação, Inovação e Desenvolvimento (FP-I3ID), Universidade Fernando Pessoa, Porto, Portugal
Catarina Teixeira Alves - catarinateixeira@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Case report
Pages - 78-84
Go to Volume
Article History
Received on 23/04/2024
Accepted on 10/03/2025
Available Online on 12/05/2025
Keywords
Case Report
�
Effect of diode laser frenectomy on tongue anatomy and function � Clinical cases
Efeito na anatomia e fun��o da l�ngua ap�s frenectomia a laser d�odo � Casos cl�nicos
�
Catarina Teixeira Alves1,* , 0009-0006-2091-5752
Cristina Cardoso1,2 Silva 0000-0003-3757-596X
Ot�lia Pereira-Lopes1,2 0000-0002-6199-4091
1 Faculdade de Ci�ncias da Sa�de (FCS-UFP), Universidade Fernando Pessoa, Porto, Portugal
2 Instituto de Investiga��o, Inova��o e Desenvolvimento (FP-I3ID), Universidade Fernando Pessoa, Porto, Portugal
�
�
Article history:
Received 23 April 2024
Accepted 10 March 2025
Available online 8 May 2025
�
Abstract
This article describes two clinical cases of pediatric patients aged 9 years who were diagnosed with alteration of the lingual frenulum and subsequently underwent diode laser frenectomy after multidisciplinary clinical evaluation. Post-surgical functional and phonetic changes were evaluated using the Marchesan Protocol for Lingual Frenulum Assessment and the Wong-Baker Pain Face Scale. The cases presented showed improvements in anatomical parameters and tongue motricity after frenectomy. However, analysis of phonetic changes revealed that immediate improvements were most evident in the less complex sounds, while more challenging phonetic changes (such as reservation, omission, and substitutions and phonemes) required further rehabilitation. This result reinforces that surgical intervention is only one component of the therapeutic process and must be complemented by an interdisciplinary approach that includes speech therapy adapted to the patient's specific needs to improve clinical and functional results.
Keywords: Ankyloglossia, Laser, Lingual frenulum, Speech, Surgery
�
Resumo
O presente artigo descreve dois casos cl�nicos de pacientes com 9 anos de idade, diagnosticados com altera��o do freio lingual e subsequentemente submetidos a frenectomia a laser d�odo ap�s avalia��o cl�nica multidisciplinar. Para avaliar as altera��es funcionais e fon�ticas p�s-cir�rgicas foi utilizado o Protocolo de Marchesan para Avaliação do Freio Lingual juntamente com a Escala de Faces de Dor de Wong-Baker. Nos casos apresentados, verificaram-se melhorias nos par�metros anat�micos e de motricidade lingual ap�s a cirurgia. Contudo, a an�lise das altera��es fon�ticas demonstrou que as melhorias imediatas foram mais evidentes nos sons menos complexos, enquanto as altera��es fon�ticas mais desafiantes (como distor��o, omiss�o e substitui��o e fonemas) exigem reabilita��o adicional. Este resultado refor�a que a interven��o cir�rgica � apenas um componente do processo terap�utico e deve ser complementada por uma abordagem interdisciplinar que inclua terapia da fala adaptada �s necessidades espec�ficas do paciente, para otimizar os resultados cl�nicos e funcionais.
Palavras-chave: Anquiloglossia, Laser, Freio lingual, Fala, Cirurgia
�
Introduction
Ankyloglossia (from the Greek �ankylo,� meaning �rigid,� and �glossa,� meaning �tongue�) is a partial or complete congenital anomaly of the lingual frenulum, where it is abnormally short or inserted too close to the lingual apex.1 According to the International Affiliation of Tongue-Tie Professionals (IATP), this condition is also known as �symptomatic tonguetie� or �symptomatic ankyloglossia.� It can be classified as anterior or posterior. In anterior ankyloglossia, the tongue�s protrusion movements are restricted and originate a �heartshaped� appearance due to the involvement of the tip of the tongue. Posterior ankyloglossia is difficult to identify and, unlike the former, does not involve the tip of the tongue but rather the thickening of the frenulum, which shows a fibrous appearance.2
Ankyloglossia�s prevalence varies from 0.1% to 10.7%,3 and its incidence from 0.02% to 5%.4 - 6 Clinically, it results in restriction of normal lingual movements and can be associated with functional limitations, such as interference with feeding, sucking, and swallowing, and phonetic disorders with speech imprecision due to exchange or distortion of lingual sounds, among others.7 These phonetic and functional challenges underline the importance of a multidisciplinary approach, where dentistry and speech therapy intervention play key roles.
While the speech therapist addresses the functional rehabilitation of speech and swallowing, the dentist focuses on the structural and surgical correction of the lingual frenulum. This collaboration is particularly critical in pediatric cases, where early intervention can have a significant impact on developmental outcomes.
There are three main surgical options to correct the altered lingual frenulum: frenotomy, frenectomy, and frenuloplasty. In summary, frenotomy is most commonly used in neonates and infants due to its simplicity and effectiveness, while frenectomy and frenuloplasty are the procedures of choice for corrective therapy in children, adolescents, and adults.8
The most common technique to correct tongue-tie is using a conventional scalpel. However, several clinicians have suggested using a soft-tissue laser as a favorable technique for correcting short lingual and/or labial frenulae.9, 10 Laser technology can provide a more precise incision in a shorter operative time, cauterize small blood and lymphatic vessels through its hemostatic and anti-inflammatory effects, minimize discomfort and pain during the intraoperative period, significantly reduce postoperative discomfort, and facilitate the healing process of the surgical wound.11 Moreover, numerous studies have documented that the incision in the soft tissues of the oral cavity with a laser is less painful than the incision with a scalpel and that patients treated with a laser have less pain and fewer functional complications after surgery than those who underwent conventional surgery. However, no specific surgical approach has been shown to be superior to the others to the point of being recommended as a gold standard.12
Ideally, this condition should be diagnosed shortly after birth. It may also be diagnosed during the baby�s first dental visit, which, according to the European Academy of Paediatric Dentistry (EAPD) and the American Academy of Pediatric Dentistry (AAPD), should be at the time of eruption of the first primary tooth or one year of age, if no teeth have erupted.
Numerous diagnostic instruments are available to the dentist for lingual frenulum anomalies, the most notable of which is the Marchesan�s Lingual Frenulum Assessment Protocol (hereafter, Marchesan Protocol),< 13 - 15 whose primary objective is to evaluate and score the various lingual frenular characteristics, normal or abnormal.
The integration of dentistry and speech therapy is crucial in managing tongue-tie cases, as these professionals address different but complementary aspects of the condition. While dentists provide surgical solutions, speech therapists ensure proper functional rehabilitation through exercises to optimize oral-motor skills. This multidisciplinary approach is essential to achieving structural correction and long-term functional improvement likewise, particularly in children whose speech and feeding skills are still developing.
We present two clinical cases to measure and compare the functional and/or phonetic activity before and after the surgical treatment of altered lingual frenula in two children.
Our aim was to monitor the postoperative condition after laser frenectomy and quantify the patients� discomfort by understanding the substantial differences felt in their functional and/or phonetic activity after the therapeutic approach.
�
Clinical Cases
Two 9-year-old pediatric patients, named Clinical Case 1 (C1) and Clinical Case 2 (C2), were evaluated at the Pedagogical Clinic of Dental Medicine at Fernando Pessoa University for difficulties in speech and tongue mobility due to short lingual frenula. Both patients had no previous surgical intervention and were undergoing regular speech therapy.
The Marchesan Protocol was used to evaluate the lingual frenulum at three different time points: preoperatively and postoperatively at 1 and 4 weeks. Photographs were taken for comparative analysis. Frenectomy with the Lasotronix Smart M� diode laser (Lasotronix, Poland) at 980 nm was the procedure chosen after obtaining informed consent from the parents.
In C1, no systemic pathology was reported. The patient had been bottle-fed for up to 2 years and had onychophagia. Clinical evaluation revealed significant phonetic changes without affecting chewing or swallowing and confirmed anterior ankyloglossia with a short and anteriorized frenulum (Figure 1). Before the procedure, local anesthesia was performed using 2% lidocaine with epinephrine (1:100000), applied through infiltration. The procedure lasted 15 minutes.
�

Figure 1. Initial situation of patient C1 � maximum lingual elevation achieved with the mouth open
�
In C2, the patient had a history of atopic skin and had been breastfed and then bottle-fed. There was a family history of ankyloglossia. Clinical evaluation indicated posterior ankyloglossia with a fibrous frenulum (Figure 2). Similar to C1, phonetic changes were noted without affecting other oral functions. Before the procedure, local anesthesia with 2% lidocaine and epinephrine (1:100000) was used. The procedure lasted 15 minutes.
�

Figure 2. Initial situation of patient C2 � maximum lingual elevation achieved with the mouth open.
�
Laser frenectomy was performed in both cases, using local anesthesia and lingual stabilization techniques for surgical precision. The laser was adjusted to specifications that minimize discomfort and maximize effectiveness. Postoperative medication included paracetamol for pain control, and no additional medications were necessary.
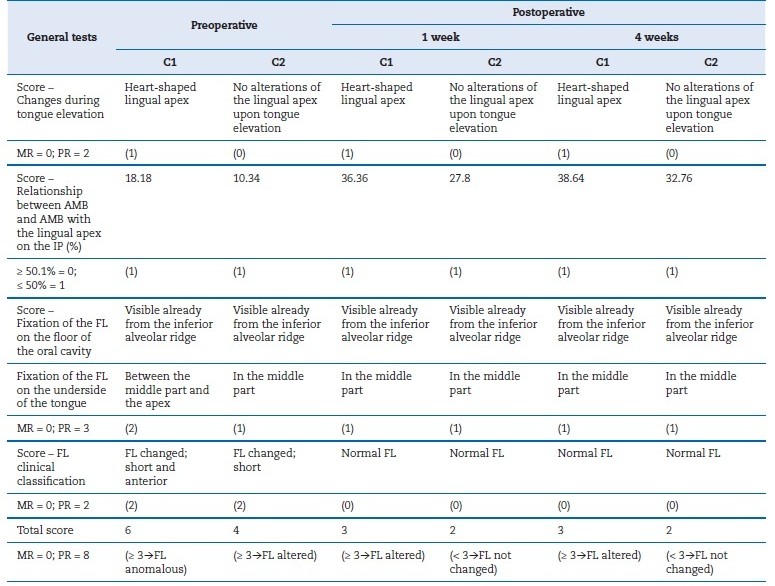
Preoperative analysis using the Marchesan Protocol revealed an abnormal lingual frenulum with scores of 6 for C1 and 4 for C2. A score of 6 in the Marchesan Protocol indicates a severe limitation in tongue mobility, while a score of 4 represents a moderate limitation. Postoperative evaluations showed improvement, with C1 maintaining an altered frenulum (score 3) and C2 being completely corrected (score 2). A score of 3 reflects mild restriction of tongue movement, and a score of 2 indicates normal mobility.
Postoperative care included the administration of paracetamol and detailed instructions for pain control and oral hygiene.
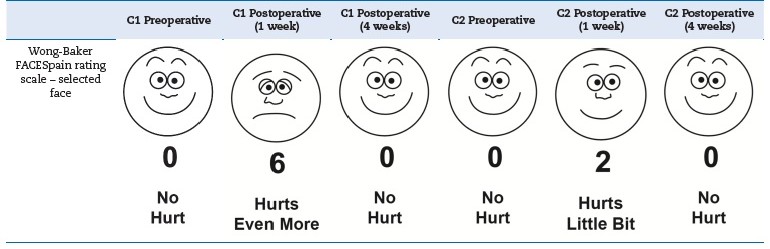
Follow-up consultations revealed progress in healing and tongue mobility, using the Marchesan Protocol and the Wong-Baker FACES pain rating scale to monitor patients� well-being (Tables 11, 2, and 3).
�
Table 1. Description of the preoperative general tests and the postoperative general test after 1 week and after 4 weeks.
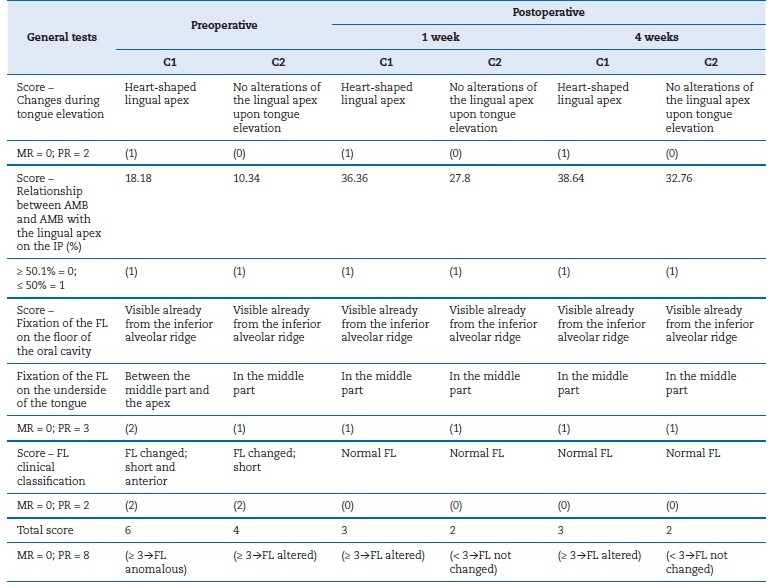
C1 � Clinical Case 1; C2 � Clinical Case 2; AMB � maximum mouth opening; PI � incisive papilla; FL � lingual frenulum; % � percentage;
mm � millimeters; MR � best result; PR � worst result.
�
Table 2. Description of functional tests conducted preoperatively and postoperatively after 1 week and 4 weeks.
�
Table 3. Description of the results of the Wong-Baker FACES pain rating scale concerning the preoperative period and the postoperative periods after 1 week and 4 weeks.
�
Re-evaluations confirmed significant functional and anatomical improvements, validating the intervention performed. Both patients showed progressive recovery with a reduction in the lingual limitations initially observed (Figures 3, 4, and 5).
�

Figure 3. 1-week post-operative control of patient C1 � maximum lingual elevation achieved with the mouth open.
�

Figure 4. 4-week post-operative control of patient C1 � maximum tongue elevation achieved with the mouth open.
�

Figure 5. 1-week post-operative control of patient C2 � clinical appearance of the fibrin clot formed in the surgical site treated.
�
Discussion and Conclusions
The effect on tongue anatomy and function after diode laser frenectomy in the two clinical cases presented, C1 and C2, resulted in improvements. The use of the Marchesan Protocol proved essential for the systematical and reliable measurement of changes in tongue anatomy and function after diode laser frenectomy. This finding reinforces the validity of this protocol and highlights its clinical relevance in understanding the results obtained.
Regarding the postoperative morphological and anatomical parameters of the Marchesan Protocol, the lingual frenulum was still classified as altered in C1, while it was classified as unchanged in C2. Given the persistence of lingual frenulum alterations in C1, it may be pertinent to consider what benefit could have been achieved by a deeper intervention, namely, the dissection of the genioglossus muscle.
Postoperative evaluations revealed no lingual frenulum change in C2. Despite expectations that this patient would exhibit the greatest phonetic potential improvement, C1 showed the most functional gains, with complete correction of the preoperative phonetic changes. Conversely, C2 continued to experience difficulty with correctly pronouncing some isolated and combined phonemes, such as [s], [z], [ch], and the persistence of possible compensatory mechanisms (such as mandibular deviation) was noted.
The dichotomy and apparent lack of agreement between the anatomic-morphological and functional parameters observed in these clinical cases raise doubts about the strictly linear relationship between lingual frenulum morphology and phonetic adequacy. It also questions the contributing factors, besides the frenulum anatomy, capable of influencing speech and other functional activities of the stomatognathic system, confirming what has already been reported by other authors.16
The tailored approach to C1 and C2 highlights the importance of customizing surgical techniques to individual needs.
For instance, in C1, where some alteration of the lingual frenulum persisted postoperatively, a more invasive surgical option, such as dissection of the genioglossus muscle, could have been considered to achieve better anatomical and functional outcomes. Both cases benefited from diode laser frenectomy, which ensured precise cutting with minimal discomfort, but postoperative care, including pain management with paracetamol and oral hygiene guidance, was critical to optimizing recovery. Adjunctive surgical techniques, such as lingual stabilization during the procedure, enhanced precision, and minimized postoperative complications, were also crucial. These elements underscore the importance of a comprehensive and individualized approach to clinical intervention in managing ankyloglossia.
Nevertheless, multidisciplinary involvement between the dentist and the speech therapist is highly advisable to alleviate functional and phonetic consequences that persist after surgery, as has been so widely advocated in the most recent literature on the subject.17, 18 The speech therapist�s intervention is a fundamental part of the treatment process. Speech therapy, both preoperatively and postoperatively, plays a key role in addressing compensatory mechanisms, improving articulation, and optimizing the functional outcomes of surgical intervention.
In these cases, the integration of speech therapy could have further supported C2 in overcoming phonetic difficulties and reducing compensatory mandibular deviations observed postoperatively. The collaboration between dentists and speech therapists is crucial to achieving both anatomical correction and functional rehabilitation, ensuring comprehensive care for patients with ankyloglossia. Diode laser frenectomy ensured a cleaner, drier operative field with better visualization, as the hemostatic cut was immediate and limited to the site of contact between the optical fiber and the most superficial blood vessels. The diode laser has increasingly demonstrated its potential as an ideal alternative to conventional frenectomy.9, 10 Additionally, the literature has described other advantages of the diode laser when compared to the conventional or electric scalpel, such as the following: superior precision; lower risk of inducing unwanted
damage to adjacent tissues; significantly reduced operation duration due to not needing suture and sterilization of the surgical site; minimization of bacterial proliferation; less painful intra and postoperative periods; better acceptance by pediatric dentistry patients; absence of postincisional adhesions, thus not compromising lingual mobility in the immediate postoperative period.11
It should be noted that although the risk of complications resulting from this surgical procedure is reduced, it is not nonexistent; i.e., the patient may feel slight edema on the oral cavity floor and moderate pain in the region. The most serious risks are injury to Wharton�s ducts, damage to the anastomoses of the branches of the lingual nerves, and even damage to the deep lingual vein, which can cause profuse venous hemorrhage.19 - 21
Since the fixation site and the histological composition of the lingual frenulum cannot be modified by mobilization exercises, surgical intervention should be considered a fundamental part of the treatment plan. However, integrating speech therapy into the treatment plan is equally fundamental, as it complements surgical intervention by enhancing functional outcomes and addressing compensatory mechanisms that surgery alone cannot resolve. This multidisciplinary approach ensures a more effective and holistic resolution of the challenges posed by ankyloglossia.
In the clinical cases presented, lingual anatomy and motricity aspects improved after lingual frenectomy. However, no improvements were observed in the more complex phonetic changes, such as distortion, omission, and replacement of phonemes associated with an altered lingual frenulum. Thus, coordinated articulation with speech therapy for functional re-education becomes essential.
�
References
1. Fujinaga CI, Chaves JC, Karkow IK, Klossowski DG, Silva FR, Rodrigues AH. Lingual frenum and breast feeding:descriptive study. Audiol Commun Res. 2017;22:e1762.
2. Arruda EMG, Campos F, Vasconcelos RG, Vasconcelos MG. Repercussão da anquiloglossia em neonatos: diagnóstico, classificação, consequências clÍnicas e tratamento. Ver Salusvita (Bauru). 2019;38:1107-26.
3. Suter VGA, Bornstein MM. Ankyloglossia: facts and myths in diagnosis and treatment. J Periodontol. 2009;80:1204-19.
4. Kupietzky A, Botzer E. Ankyloglossia in the infant and young child: clinical suggestions for diagnosis and management. Pediatr Dent. 2005;27:40-6.
5. Buryk M, Bloom D, Shope T. Efficacy of neonatal release of ankyloglossia: a randomized trial. Pediatrics 2011;128:280-8.
6. Edmunds J, Miles SC, Fulbrook P. Tongue-tie and breastfeeding: a review of the literature. Breastfeed Rev. 2011;19:19-26.
7. Braga LAS, Silva J, Pantuzzo CL, Motta AR. Preval�ncia de altera��o no fr�nulo lingual e suas implica��es na fala de escolares. Ver. CEFAC. 2009;11(suppl 3):378-90.
8. Tuli A, Singh A. Monopolar diathermy is used for the correction of ankyloglossia. J Indian Soc Pedod Prev Dent. 2010;28:130-3.
9. Fioravanti M, Zara F, Vozza I, Polimeni A, Sfasciotti GL. The efficacy of lingual laser frenectomy in pediatric OSAS: A randomized double-blinded and controlled clinical study. Int J Environ Res Public Health. 2021;18:6112.
10. Nunes JEP, Silva AL, Nunes GP, Fagundes CF, Souza MR, Navarro RS. Lasers aplicados � frenectomia em pacientes pedi�tricos com anquiloglossia. Research, Society and Development. 2021;10:e19210210434.
11. Melo AJB, Santos GM, J�nior MBS, Mendes VCO, Melo PHB. Lasers de alta pot�ncia na frenectomia, seus benef�cios e limita��es: revis�o integrativa. Research, Society and Development. 2022;11:e506111234806.
12. Lima CB, Maranh�o VF, Botelho KVG, Junior VES. Avaliação da anquiloglossia em neonatos por meio do teste da linguinha: um estudo de prevalência. RFO (Passo Fundo). 2018;22:294-7.
13. Marchesan IQ. Lingual frenulum: quantitative evaluation porposal. Int J Orofacial Myology. 2005;31:39-48.
14. Marchesan IQ. Protocolo de avalia��o do fr�nulo da l�ngua. Rev CEFAC. 2010;12:977-89.
15. Marchesan IQ. Lingual frenulum: classification and speech interference. Int J Orofacial Myology. 2004;30:31-8.
16. Pereira TS, Oliveira F, Cardoso MCAF. Association between harmful oral habits and the structures and functions of the stomatognathic system: perception of parents/guardians. CoDAS; 2017;29,e20150301.
17. Gomes E, Ara�jo FBD, Rodrigues J�. Freio lingual: abordagem cl�nica interdisciplinar da Fonoaudiologia e Odontopediatria. Revista da Associa��o Paulista de Cirurgi�es Dentistas. 2015;69:20-4.
18. Miranda PP, Cardoso CL, Gomes E. Interventions in the Alteration on Lingual Frenum: Systematic Review. Int Arch Otorhinolaryngol. 2016;20:275-80.
19. Hall DMB, Renfrew MJ. Tongue tie. Arch Dis Child. 2005;90:1211-5.
20. Lalakea ML, Messner AH. Frenotomy And Frenuloplasty: If, When, And How. Operative Techniques in Otolaryngology � Head and Neck Surgery. 2002;13:93-7.
21. Yang H, WooY, Won S, Kim D, Hu K, Kin H.. Course and Distribution of the Lingual Nerve in the Ventral Tongue Region: Anatomical Considerations for Frenectomy. J Craniofac Surg. 2009;20:1359-63.
�
Catarina Teixeira Alves
E-mail address: catarinateixeira@hotmail.com
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Catarina Teixeira Alves: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing � original draft. Cristina Cardoso Silva: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing � review & editing. Ot�lia Pereira-Lopes: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization,Writing � review & editing.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
