
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (2) | 114-120
Case report
The importance of cone-beam computed tomography for the diagnosis and treatment plan of florid cemento-osseous dysplasia: a case report
A importância da tomografia computadorizada de feixe cónico para o diagnóstico e plano de tratamento da displasia cemento-óssea florida: relato de caso
a Faculdade de Odontologia, Universidade Veiga de Almeida (UVA), Rio de Janeiro, RJ, Brasil
b Departamento de Patologia e Diagnóstico Oral, Faculdade de Odontologia, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil
Eduardo Murad Villoria - d.villoria82@yahoo.com.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 2
Case report
Pages - 114-120
Go to Volume
Article History
Received on 17/08/2020
Accepted on 20/02/2021
Available Online on 30/06/2021
Keywords
Case Report
�
The importance of cone-beam computed tomography for the diagnosis and treatment plan of florid cemento-osseous dysplasia: a case report
A import�ncia da tomografia computadorizada de feixe c�nico para o diagn�stico e plano de tratamento da displasia cemento-�ssea florida: relato de caso
�
Nat�llia Medeiros Corr�a1 0000‐0002‐4960‐2366
Hary Wanzeller da Silva1 0000‐0001‐9608‐8809
Cristine da Silva Furtado Amaral1 0000‐0003‐0412‐6332
Claudia Bragan�a do Valle1 0000‐0003‐4259‐2502
Maria Augusta Visconti2 0000‐0002‐8837‐8387
Eduardo Murad Villoria1,* 0000‐0002‐4671‐3650
1 Faculdade de Odontologia, Universidade Veiga de Almeida (UVA), Rio de Janeiro, RJ, Brasil.
2 Departamento de Patologia e Diagn�stico Oral, Faculdade de Odontologia, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil
�
�
Article history:
Received 17 August 2020
Accepted 20 February 2021
Available online 30 June 2021
�
Abstract
Cone-beam computed tomography (CBCT) provides images without overlapping anatomical structures, which is important for the diagnosis and assessment of florid cemento-osseous dysplasia. This fibro-osseous lesion that affects the alveolar process without compromising the teeth� pulp vitality is usually asymptomatic, and bone expansion, cortical disruption, and root resorption are uncommon. Due to its avascular characteristic, surgical procedures are often contraindicated. In this case, a 59-year-old female patient presented with a complaint of pain in the right maxillary central incisor. Panoramic and periapical radiographs showed florid cemento-osseous dysplasia in some regions. The right maxillary central incisor showed an extensive radiolucent image suggestive of root resorption but without fibro-osseous lesion. For better evaluation and implant planning, CBCT was performed and demonstrated florid cemento-osseous dysplasia adjacent to the right maxillary central incisor, contraindicating implant placement. In other regions, CBCT enabled the identification of the expansive features of this fibro-osseous lesion.
Keywords: Case report, Cone-beam computed tomography, Diagnostic imaging, Florid cemento-osseous dysplasia, Radiography.
�
Resumo
A tomografia computadorizada de feixe c�nico (TCFC) fornece imagens sem sobreposi��o, sendo importante para o diagn�stico e avalia��o da displasia cemento-�ssea florida. Esta les�o fibro-�ssea, que acomete o processo alveolar sem comprometer a vitalidade pulpar dos dentes, costuma ser assintom�tica, sendo incomum a expans�o �ssea, o rompimento cortical e a reabsor��o radicular. Devido � caracter�stica avascular, procedimentos cir�rgicos s�o muitas vezes contraindicados. No presente caso, uma paciente do sexo feminino, 59 anos, apresentava dor no incisivo central superior direito. As radiografias panor�mica e periapical demonstraram displasia cemento-�ssea florida em algumas regi�es. O incisivo central superior direito apresentava imagem radiol�cida extensa, sugestiva de reabsor��o radicular interna, mas sem les�o fibro-�ssea. Para melhor avalia��o e planeamento do implante, a TCFC foi realizada e demonstrou displasia cemento-�ssea florida adjacente ao incisivo central superior direito, contraindicando a coloca��o do implante. Em outras regi�es, a TCFC permitiu a identifica��o de caracter�sticas expansivas dessa les�o fibro-�ssea.
Palavras-chave: Caso cl�nico, Tomografia computadorizada de feixe c�nico, Diagn�stico por imagem, Displasia cemento-�ssea florida, Radiografia.
�
Introduction
In 1998, in Japan, Arai and his team developed a cone-beam computed tomography (CBCT) system with a smaller field of view than previously available. It received regulatory approval in 2000 and has been widely used since approval for coverage by the National Health Insurance system in 2012.1 This imaging technique allows dental practitioners to observe and diagnose lesions in the dental hard tissue in three dimensions without the overlapping of anatomical structures and with a lower radiation dose compared to multislice computed tomography (CT).2, 3 It offers greater accuracy in the diagnosis and evaluation of odontogenic cysts, odontogenic tumors, and fibro-osseous lesions, such as cemento-osseous dysplasia (COD).4 5
COD is a non‑neoplastic fibro‑osseous lesion seen more frequently in black women, with a peak incidence in the fourth and fifth decades of life.6 - 8 Although its etiology is uncertain, it is believed to originate from the periodontal ligament,6 affecting the alveolar process without compromising the pulp vitality of the teeth involved. COD is usually asymptomatic, and bone expansion, cortical rupture, and root resorption are uncommon.5 - 7 This fibro-osseous lesion is classified into three types: periapical, focal, and florid. Florid cemento-osseous dysplasia (FLCOD) shows a tendency to bilateral involvement, differing radiographically from periapical (PCOD) and focal (FCOD) cemento‑osseous dysplasias, which are associated with anterior and posterior teeth in a single quadrant, respectively.8
Radiographically and histologically, FLCOD shows a pattern of maturation similar to that observed in PCOD and FCOD.
The initial osteolytic stage involves bone tissue reabsorption and the presence of fibrous tissue rich in cells and vessels, providing a radiolucent or hypodense image. As maturation progresses over time, cement-like formations and irregular trabeculae appear, causing a mixed pattern image. In the final matured osteogenic stage, radiographically characterized by radiopaque or hyperdense patterns, these structures are connected, and few cellular elements are visible.6, 7
As FLCOD does not require treatment and its diagnosis can be performed only with clinical and imaging examinations, some authors do not recommend biopsy due to this lesion�s avascular characteristics, which could increase the risk of osteomyelitis after surgical procedures.9 Elective surgeries, such as implant placement, are contraindicated due to the increased risk of bone infection and osseointegration failure.10
On the other hand, studies have demonstrated success in dental implant placement in areas close to the fibro-osseous lesion, offering a possibility to patients affected by FLCOD.10, 11
Thus, the present case report aimed to describe the importance of CBCT in the diagnosis of FLCOD and the choice of the appropriate treatment plan for the patient.
Case report
A 59‑year‑old black female patient complaining of pain in her right maxillary central incisor visited the School of Dentistry of Veiga de Almeida University for evaluation in March 2018.
On extraoral clinical examination, no changes were seen. On the other hand, intraoral clinical examination revealed a poorly adapted total crown and gum with a swollen aspect on the right maxillary central incisor.
As a protocol of the Veiga de Almeida University, digital panoramic radiography (DPR) had been performed in the prerevvious year�s dental screening (May 8, 2017), using the Orthopantomograph OP300 (Instrumentarium, Tuusula, Finland) at 66 kVp, 10 mA, and 14.1 seconds. The DPR showed a radiolucent image surrounded by a radiopaque halo associated with the roots of the right maxillary first molar, which was vital, and radiopaque images in the maxilla�s and mandible�s bilateral regions compatible with different stages of FLCOD. However, no changes were observed in the right maxillary central incisor (Figure 1).
�

Figure 1. Initial digital panoramic radiography.
�
For a better evaluation of the right maxillary central incisor, periapical radiography (PR) was performed using the D 700 device (Dabi Atlante, Ribeir�o Preto, SP, Brazil) at 70 kVp, 8 mA, and 0.4 seconds, and an E-speed radiographic film, size 2 (Carestream Health, Inc, NY, USA). The PR showed the right maxillary central incisor with filling material below the root apex, a discrete radiolucent image adjacent to the root�s apex, na extensive radiolucent image suggestive of internal root resorption or drill wear, and deviation of the intrarradicular pin. Additionally, FLCOD was observed adjacent to the lateral incisors� and left maxillary central incisor�s roots (Figure 2).
�

Figure 2. Initial periapical radiography.
�
As the PR did not demonstrate an image compatible with FLCOD adjacent to the right maxillary central incisor�s root, the patient was referred to the specialization course in implantology for implant placement planning in the region. For a better evaluation, the patient was referred to an Oral Radiology center to perform CBCT on May 2, 2018, using an i‑CAT Next Generation device (Imaging Sciences International, Hatfield, PA, USA) with a medium field of view (FOV) of 16�6 cm, isotropic voxel of 0.25 mm, 120 kVp, 5 mA, and 26.9 seconds. The images were analyzed using the On‑Demand 3D software (Cyber Med, Seoul, South Korea).
In CBCT reconstructions of the maxilla, hyperdense images were observed, surrounded by a discrete hypodense halo in some regions, associated with the roots of canines, lateral incisors, central incisors, right first molar, and left second molar, and a hypodense image associated with the roots of the right second molar compatible with FLCOD at diferente stages of maturation (Figure 3). The right first molar showed a hyperdense image surrounded by a hypodense halo, with a fusion between the fibro-osseous lesion and the roots, causing external root resorption and vestibular bone expansion.
�
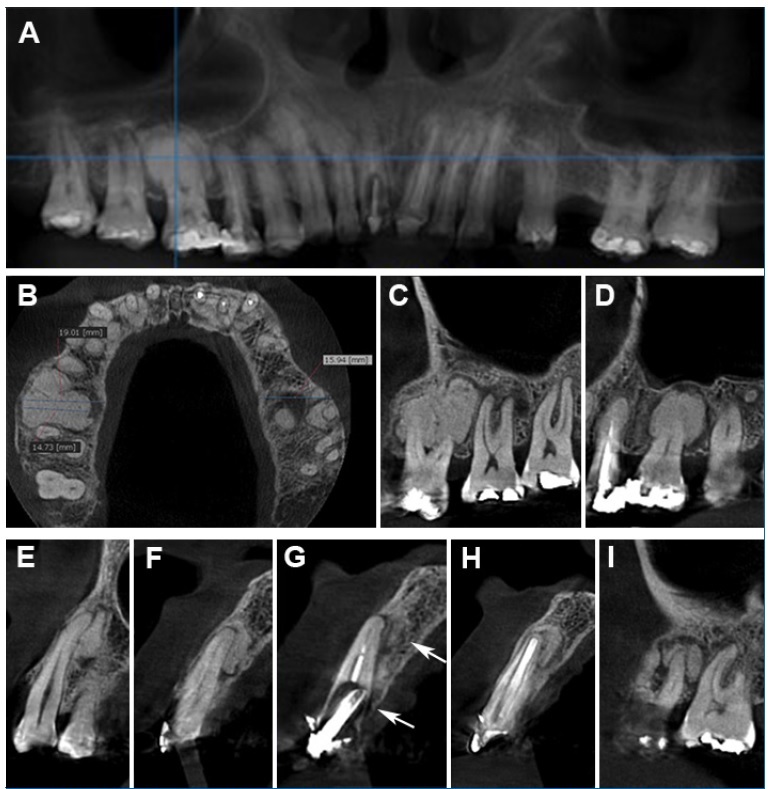
Figure 3. Initial cone‑beam computed tomography. A - Panoramic reconstruction, with a thickness of 15 mm. B, C, and D - Axial and sagittal slices showing a hyperdense image delimited by a hypodense halo in some regions associated with the right maxillary first molar�s roots. Bone expansion was observed in the region (19.01 mm). E‑ I - Sagittal slices showing hyperdense images associated with roots of the right canine (E), right lateral incisor (F), right central incisor (G) (arrow), left central incisor (H), and left second molar (I), compatible with FLCOD in the sclerotic phase.
�
Additionally, the FLCOD associated with this tooth was close to the alveolar bone crest (Figure 3). The sagittal slice of the right central incisor showed an inclination of the intrarradicular pin and a discrete periradicular bone rarefaction by the palate, suggesting root crack or perforation, as well as a hyperdense image adjacent to the root compatible with FLCOD (Figure 3).
Therefore, after the tomographic diagnosis of FLCOD associated with the right maxillary central incisor, it was decided not to perform surgery for dental implant placement due to the risk of developing osteomyelitis and osseointegration failure.10, 12 However, due to the diagnosis of root crack or perforation and incipient periradicular bone rarefaction, extraction and rehabilitation using a removable partial denture was performed.
As the patient�s FLCOD had an expansive pattern but no symptoms associated, only clinical and CBCT follow‑up was indicated without the need for biopsy or other surgical procedure. Monitoring of the hyperdense image at the right maxillary first molar and the bone condition after the extraction of the right maxillary central incisor was done by a new CBCT scan on June 19, 2019, using an i-CAT Classic device (Imaging Sciences International, Hatfield, PA, USA) with a FOV of 16 � 13 cm, isotropic voxel of 0.25 mm, 120 kVp, 36 mA, and 40 seconds. The images were analyzed using the same software used for the first CBCT. Due to the previous diagnosis of FLCOD close to the alveolar bone crest causing cortical expansion and root resorption in a maxillary tooth, it was decided to perform a CBCT scan with a larger FOV to assess the lesions in the mandible.
In CBCT reconstructions of the mandible, FLCOD was observed associated with the anterior teeth� and left second premolar�s roots and the edentulous regions in both sides (Figure 4). The panoramic and three‑dimensional volumetric reconstructions demonstrated FLCOD close to the alveolar bone crest in the regions of the missing left first molar and right second premolar (Figure 4). The axial and oblique slices showed FLCOD close to the cortical bone, causing expansion and disruption of the lingual bone cortex in the regions of the left and right canines (Figure 4).
�
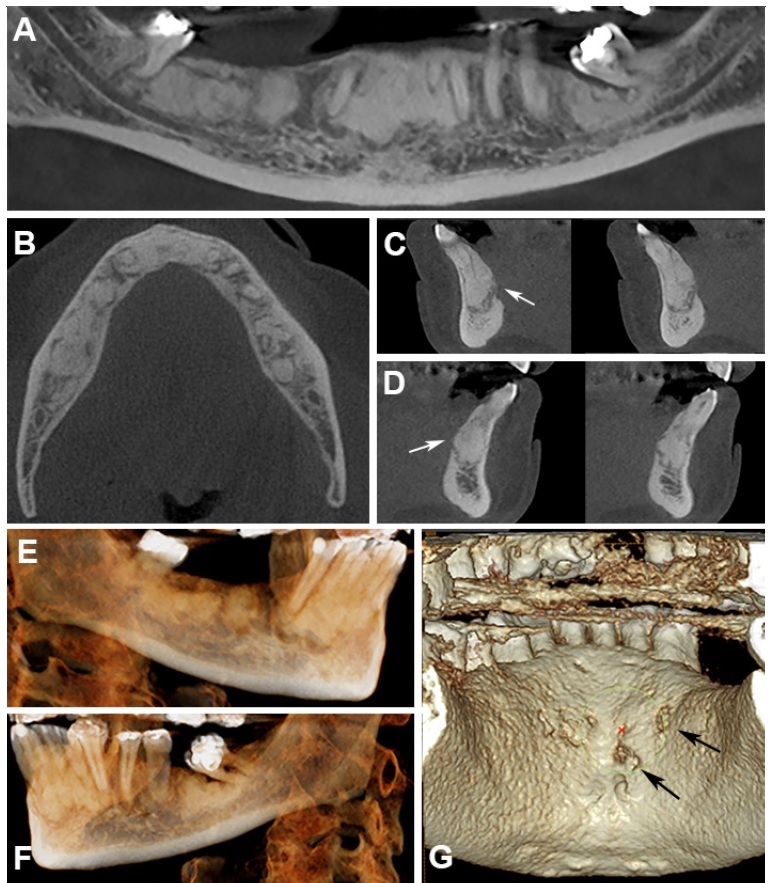
Figure 4. Second cone-beam computed tomography, one year after the first exam, demonstrating FLCOD in the mandible. A - Panoramic reconstruction, with a thickness of 5 mm. B, C, and D - Axial and oblique slices showing FLCOD close to the cortical bone, causing expansion and disruption of the lingual bone cortex in the regions of the right (C) and left (D) canines (arrows). E, F, and G - Three‑dimensional volumetric reconstructions demonstrating FLCOD close to the alveolar bone crest in the regions of the missing right second premolar (E) and left first molar (F), as well as images that may suggest disruption of the lingual bone cortex in the region of the anterior teeth (G) (arrows).
�
Regarding the CBCT monitoring of lesions associated with the maxillary teeth, there were no dimensional changes in the FLCOD associated with the right first molar nor expansion of the buccal bone cortex, maintaining a thickness of 19 mm in the alveolar bone (Figure 5). Additionally, we observed that the patient had undergone endodontic treatment in a private clinic without our knowledge. The sagittal and oblique slices of the missing right central incisor showed a hypodense image suggestive of a postoperative bone defect or alveolar bone in the healing process and a hyperdense image surrounded by a hypodense halo compatible with FLCOD (Figure 5).
�
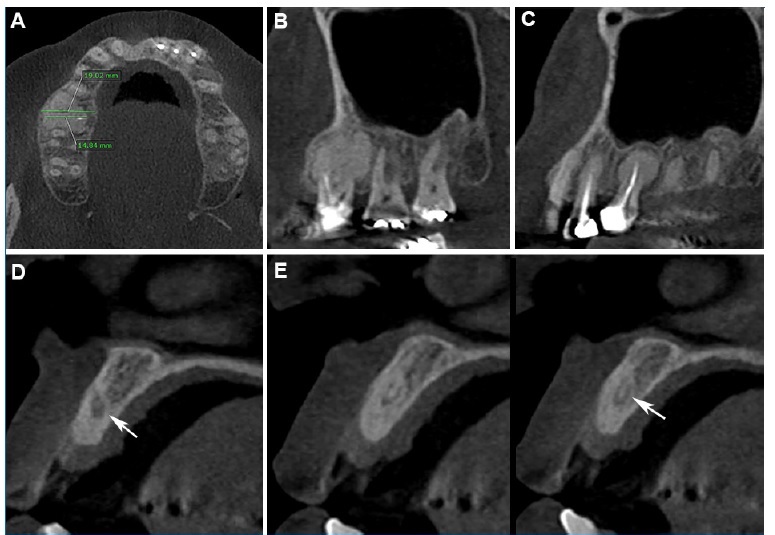
Figure 5. Second cone-beam computed tomography one year after the first exam, demonstrating multiplanar reconstructions in the regions of the right maxillary first molar and right maxillary central incisor. A, B, and C - Axial and sagittal slices of right maxillary first molar demonstrating that the fibro‑osseous lesion and the adjacent bon� structure did not change. D - Sagittal slice presenting hypodense image compatible with a postoperative bone defect or alveolar bone in the healing process (arrow). E - Oblique slices showing FLCOD in the region of the missing right maxillary central incisor (arrow).
�
Discussion and conclusions
The present clinical case was written according to the CARE guidelines (www.care‑statement. org), which propose the improvement, integrity, and transparency of case reports.13
The initial diagnosis of FLCOD was performed by clinical and radiographic examinations of the patient, which shows the importance of associating information from both, since, depending on its stage, FLCOD may be radiographically similar to periapical lesions, Gardner�s syndrome, diffuse sclerosing osteomyelitis, cemento-ossifying fibroma, fibrous7, 14 In this study, the patient had undergone endodontic treatment on maxillary central incisors, left maxillary lateral incisor, and left maxillary canine, suggesting that these interventions were performed when the FLCOD was in its osteolytic phase, resembling a periapical lesion, without performing the pulp vitality test. Additionally, the extensive hyperdense image at the right maxillary first molar showed tomographic characteristics similar to cementoblastoma since it was fused to the roots, reabsorbing them and causing bone expansion. However, as the DPR from the previous year showed a radiolucent lesion with a radiopaque halo and the 59-year-old patient had no symptoms in the maxillary lesion, which are uncommon in cementoblastoma, and the FLCOD can have characteristics of external root resorption and bone expansion, we suggest the diagnosis of this type of fibroosseous lesion for this region.5, 6, 15
In the present study, CBCT was performed to confirm the radiographic diagnosis of absence of fibro‑osseous lesion in the region of the right maxillary central incisor, which was suspected of having internal root resorption or drill wear and root crack, as well as to evaluate the bone structure for dental implant planning. Contrary to radiographic examinations, CBCT demonstrated FLCOD associated with the root, contraindicating the implant placement. Due to the COD�s avascular characteristics, surgical procedures such as biopsy, extraction, and dental implants should be avoided.10 COD, especially in the mixed and sclerotic phases, shows a small amount of vascularized connective tissue and a large volume of avascular or dense hypovascular osteo-cementoid structures. This tissue can compromise post‑surgical repair, directly affecting osseointegration and leading to a greater risk of osteomyelitis.10
However, other authors found success in implant placement in a patient with FLCOD in regions where the fibro-osseous lesion was absent.12 In the region where the lesions were present, the authors indicated rehabilitation with a fixed prosthesis,12 corroborating the procedure adopted in the present study.
Due to this risk of postoperative infection and because it is a bone pathology that, in most cases, does not require treatment, the diagnosis of COD should be based only on clinical and imaging assessment.9 Previous studies have highlighted the importance of CBCT for the diagnosis, assessment, and monitoring of COD because it allows greater accuracy in visualizing this fibroosseous lesion and its relationship with adjacent anatomical structures, which is essential to choose the adequate therapy and prevent exposure of avascular mineralized tissue in the oral cavity and consequent infection.5, 6 As previously described,5, 6 in the present case, CBCT helped identify expansive and aggressive features of FLCOD, such as external root resorption in the right maxillary first molar, bone expansion, and cortical rupture.
This study�s limitations are related to the patient having sought dental care in a private clinic without our knowledge, where she underwent endodontic treatment on the right maxillary first molar, which was vital, extraction of the right maxillary central incisor, and rehabilitation with a removable partial denture.
In conclusion, in the present case report, CBCT enabled the diagnosis of FLCOD in a region where PR did not provide a conclusive image, avoiding dental implant placement and helping choose the best treatment for the patient. In addition, CBCT enabled the visualization of FLCOD�s expansive and aggressive features, such as external root resorption, bone expansion, and cortical disruption, and also allowed a better assessment of the proximity of the fibro‑osseous lesion to the alveolar bone crest. It is important to monitor FLCOD to avoid exposure of avascular tissue and infection.
�
References
1. Hayashi T, Arai Y, Chikui T, et al. Clinical guidelines for dental cone-beam computed tomography. Oral Radiol. 2018;3:89-104.
2. Tanimoto H, Arai Y. The effect of voxel size on image reconstruction in cone‑beam computed tomography. Oral Radiol. 2009;25:149-53.
3. Nasseh I, Al‑Rawi W. Cone Beam Computed Tomography. Dent Clin North Am. 2018;62:361-91.
4. Lee JH, Kim DH, Jeong SN. Diagnosis of cystic lesions using panoramic and cone beam computed tomographic images based on deep learning neural network. Oral Diseases. 2020;26:152-8.
5. Kato CNAO, Barra SG, Amaral TMP, et al. Cone‑beam computed tomography analysis of cemento‑osseous dysplasia-induced changes in adjacent structures in a Brazilian population. Clin Oral Invest. 2020;24:2899-908.
6. Cavalcanti PHP, Nascimento EHL, Pontual MLDA, et al. Cemento‑osseous dysplasias: imaging features based on cone beam computed tomography scans. Braz Dent J. 2018;29:99-104.
7. Brody A, Zalatnai A, Csomo K, Belik A, Dobo-Nagy C. Difficulties in the diagnosis of periapical translucencies and in the classification of cemento‑osseous dysplasia. BMC Oral Health. 2019;19:139-47.
8. Speight PM, Takata T. New tumour entities in the 4th edition of the World Health Organization Classification of Head and Neck tumours: odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472:331-9.
9. Moreti LCT, Barbosa PAC, Boer NCP, Fernandes KGC, Ogata M. Displasia cemento‑�ssea florida: relato de caso. Arch Health Invest. 2016;5:120-5.
10. Oliveira MTF, Cardoso SV, Silva CJ, Barbosa DZ, Loyola AM. Failure of dental implants in cemento‑osseous dysplasia: a critical analysis of a case. Rev Odontol UNESP. 2014;43:223-7.
11. Shin HS, Kim BC, Lim HJ, Jo SY, Lee J. Chronic osteomyelitis induced by the placement of dental implants on cementoosseous dysplasia. Br J Oral Maxillofac Surg. 2019;57:268-70.
12. Esfahanizadeh N, Yousefi H. Successful implant placement in a case of florid cemento‑osseous dysplasia: a case report and literature review. J Oral Implantol. 2018;44:275-9.
13. Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-35.
14. Yildirim E, Bağlar S, Ciftci ME, Ozcan E. Florid cemento‑osseous dysplasia: A rare case report evaluated with cone-beam computed tomography. J Oral Maxillofac Pathol. 2016;20:329-39.
15. Sankari LS, Ramakrishnan K. Benign cementoblastoma. J Oral Maxillofac Pathol. 2011;15:358-60.
�
Eduardo Murad Villoria
E-mail address: d.villoria82@yahoo.com.br
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
1646-2890/� 2021 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
