
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (2) | 109-113
Case report
Removable partial denture metal framework manufactured by selective laser melting technology – A clinical report
Esqueleto metálico de prótese parcial removível produzido por tecnologia Selective Laser Melting – Caso clínico
a Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
Joana Paulos Cabrita - joanacabrita@campus.ul.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 2
Case report
Pages - 109-113
Go to Volume
Article History
Received on 07/04/2021
Accepted on 08/05/2021
Available Online on 08/06/2021
Keywords
Case Report
�
Removable partial denture metal framework manufactured by selective laser melting technology - A clinical report
Esqueleto met�lico de pr�tese parcial remov�vel produzido por tecnologia Selective Laser Melting - Caso cl�nico
�
Joana Paulos Cabrita1* 0000-0002-4869-1053
Teresa Almeida Mendes1 0000-0001-6232-0251
Jo�o Paulo Martins1 0000-0001-9330-772X
Lu�s Pires Lopes1 0000-0001-8633-827X
1Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal
�
�
Article history:
Received 7 April 2020
Accepted 8 May 2021
Available online 8 Junho 2021
�
Abstract
The selective laser melting technology is an additive digital method that permits producing metal frameworks for removable partial dentures. The existing literature has compared this technique with the classic technique in terms of precision, quality of fit, and function. This work describes a clinical case of a metal framework produced by the selective laser melting technique in a patient rehabilitated with a removable partial denture.
No adjustments were required when the metal framework was inserted, showing good adaptation and stability to the abutment teeth and surrounding tissues. Further studies are necessary for a significant assessment of this technique�s clinical applicability.
Keywords: Computer-Aided Design, Computer-Aided Manufacturing, Metal frameworks, Removable partial dentures, Selective laser melting.
�
Resumo
A tecnologia selective laser melting � um m�todo digital aditivo que permite a produ��o de estruturas met�licas para pr�teses dent�rias parciais remov�veis. Esta t�cnica tem sido comparada na literatura existente com a t�cnica cl�ssica, em termos de precis�o, qualidade de ajuste e fun��o. O presente trabalho descreve um caso cl�nico de estrutura met�lica produzida pela t�cnica selective laser melting num paciente reabilitado com pr�teses dent�rias parciais remov�veis. N�o foram necess�rios ajustes quando a estrutura met�lica foi inserida, mostrando boa estabilidade e adapta��o aos dentes pilares e aos tecidos circundantes. Mais estudos s�o necess�rios para poder avaliar com signific�ncia a aplicabilidade cl�nica dessa t�cnica.
Palavras-chave: Computer-Aided Design, Computer Aided Manufacturing, Estrutura met�lica, Pr�tese parcial remov�vel, Selective laser melting.
�
Introduction
Computer‑aided design and computer‑aided manufacturing (CAD/CAM) technology became one of the most important developments in the dental field in the 21st century,1, 2, 3, 4 and presents several advantages over traditional methods. The main advantages are reducing the time and intermediary steps of the manufacturing process of prosthetic rehabilitation and reducing the material lost in the intermediary steps as waxing, investing, and casting. Other great advantages are human error elimination and the accuracy guaranteed by the CAD software.3, 5, 6
The CAM digital technologies can be divided into two methods: subtractive or additive.3 The subtractive method consists of reducing the framework from a block to the final shape designed by the CAD, and this process can be done by spark erosion or milling techniques.4 The additive methods consist of adding material and can be further divided into SLA (stereolithography), DLP (digital light projection), PolyJet / Pro-Jet (jet printing), SLM (selective laser melting), SLS (selective laser sintering), and DLMS (direct laser metal sintering).3 The SLM technology is already applied in the production of metal frameworks for removable partial dentures (RPDs).3 This technology creates three‑dimensional metal parts using a laser that melts metal powder layer by layer according to the CAD instructions.3, 6 The SLM technique�s effectiveness in terms of precision, quality of fit, and function is comparable to the frameworks produced by the classic method.3 However, there are few in vitro and in vivo studies evaluating the SLM technology.3, 7 Thus, the objective of the present work is to describe a clinical case evaluating the effectiveness of metal frameworks produced with SLM.
Case report
A 74‑year‑old female patient, systemically healthy, presented at the Faculty of Dental Medicine, University of Lisbon. The primary reason for the dental appointment was to rehabilitate the lower arch after having already undergone a well‑adapted superior rehabilitation without complaints. The patient presented a Kennedy Class I (Figure 1). The treatment plan, for economic reasons, was a mandibular RPD replacing teeth 37, 36, 35, 45, 46, and 47.
�
�

Figure 1. Initial intra‑oral photography.
�
Firstly, both maxillary and mandibular alginate preliminar impressions were taken with an irreversible hydrocolloid impression material (Turboprint, R&S) and poured with dental stone Type III (Ventura Stone, Madespa) to obtain diagnostic casts. The mandibular cast was surveyed to determine the location of teeth undercuts and guide plans, allowing the correct metal framework design with the lingual bar being the most suitable as the major connector. Dental preparations were performed following the design outlined on the diagnostic cast to produce guide planes in teeth 34 and 44, occlusal rests in teeth 34 and 44, and cingulum rests in teeth 33 and 43.
After the dental preparations, a definitive impression was performed with the customized tray in alginate (Turboprint, R&S), as well as a preliminary registration with wax occlusal rim (Metrowax) (Figure 2). This impression was poured (Type III, Ventura Stone, Madespa) to obtain the master cast. The master casts were then scanned (D700 3D scanner, 3shape, Denmark), and the metal framework was digitally drawn (Phibo developed by 3shape, Barcelona). The software used has tools similar to those of physical sculpting and enables working in a manner that mimics that of the conventional technician working in the laboratory, finding the best insertion path (Figure 3). The design used in this case is shown in Figure 4.
�

Figure 2. Final impression in irreversible hydrocolloid impression material.
�
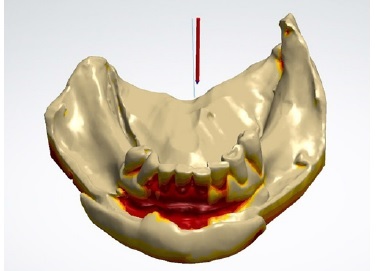
Figure 3. Best insertion path with retention depth.
�
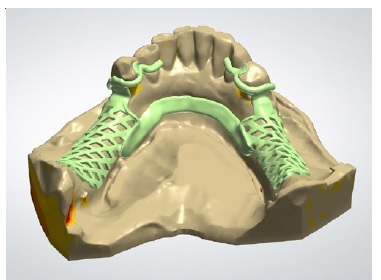
Figure 4. Saddle, major connector, and claps placement.
�
The next step included building the RPD framework on the SLM machine (EOS GmbH, Phibo, Barcelona) with a cobalt‑chromium alloy powder. Firstly, adequate supports had to be created to provide a firm base for the part to be built onto while separating it from the substrate plate. Because the supports need to be removed with tools, the part was oriented so that the supports avoided the RPD�s fitting surface and, thus, the resultant framework would not be affected or damaged by the supports or their removal.8 The framework was finished and polished using traditional dental laboratory procedures.
Subsequently, the intraoral metal framework try‑in was performed. The framework proved to have an excellent fit in the patient�s cast (Figure 5). When tested intraorally, the framework was passive and stable, adapted well to hard and soft tissues, and no occlusal adjustments were necessary. The wax occlusal rim (Metrowax) was placed on the edentulous regions of the framework, and an interocclusal record was made. Both maxillary and mandibular casts were mounted on an articulator (Asa, 5010), and artificial teeth (Stein Vit, New Stetic) were arranged (Figure 6). After the try‑in, the RPD was processed with heat‑curing acrylic resin (Probase Hot, Ivoclar Vivadent) and delivered to the patient with proper care instructions (Figures 7, 8, 9 and 10). At the post‑insertion appointment, the patient did not have any complaints regarding the prosthetic adaptation. The clinical case had a follow‑up of 2 years, during which the patient was checked every 6 months with oral hygienist and dentist control appointments, including observation of oral soft and hard tissues, teeth, and prosthetic rehabilitation.
�

Figure 5. Metal framework.
�

Figure 6. Teeth arrangement.
�

Figure 7. Mandibular occlusal view.
�

Figure 8. Frontal view.
�

Figure 9. Right buccal view.
�

Figure 10. Left buccal view.
�
Discussion and Conclusions
The present work describes the clinical and lab steps of the fabrication of an RPD whose metal framework was obtained through the SLM technique. This technique was less time‑and material‑consuming and reduced the risk of human error.
The metal framework had a correct settling, and no changes in the structure were required. These results are similar to those of Hussein & Hussein and Mansour et al., safeguarding that the former used the SLM technique and the second used the SLA technique.1, 8
The SLM technique has the key advantage of directly producing high‑precision metal components in their full density,9 which contributes to the excellent mechanical properties of the metal framework produced compared with the ones produced by traditional methods.7, 10 One of these properties is the increased resistance to distortion, which can lead to favorable occlusal force distribution among the remaining teeth and supporting tissues.11 Other advantages are the reduced manufacturing time, the automatic behavior of the technique, which reduces human error,7, 10, 11 and the possibility of recycling the remaining unprocessed metal powder to prevent material waste.10 Nonetheless, the laboratory technician requires skill, knowledge, and expensive equipment to apply this technique, and there are still gaps in this area.12
The conventional technique - the lost wax technique, is still the gold standard, but it is time‑consuming, requires multiple steps, and is technique‑ sensitive.1, 10 On the other hand, there are still few clinical studies reporting the clinical application, passivity, efficacy, and longevity of the SLM technique.
Therefore, further studies on the clinical results obtained with this technique are needed, especially in cases of more complex structures.1, 10, 11
The present clinical case study aimed to describe the effectiveness of the SLM technique in producing a Cr‑Co metal framework of a mandibular RPD. No adjustments were required when the metal framework was inserted, showing good stability and adaptation to the abutment teeth and surrounding tissues. More experimental and clinical studies are needed to evaluate this technique. Also, additional studies are needed to compare RPD frameworks fabricated by conventional, milling and SLM technique.10
�
References
1. Hussein MO, Hussein LA. Novel 3D Modeling Technique of Removable Partial Denture Framework Manufactured by 3D Printing Technology. Int J Adv Res. 2014;2:686-94.
2. Koutsoukis T, Zinelis S, Eliades G, Al‑Wazzan K, Al‑Rifaiy M, Al‑Jabbari YS. Selective Laser Melting Technique of Co‑Cr Dental Alloys: A Review of Structure and Properties and Comparative Analysis with Other Available Techniques. J Prosthodont. 2015;24:303-12.
3. Kajima Y, Takaichi A, Nakamoto T, Kimura T. Fatigue strength of Co‑Cr‑Mo alloy clasps prepared by selective laser melting. J Mech Behav Biomed Mater. 2016;59:446-58.
4. Bilgin MS, Baytaroğlu EN, Erdem A, Dilber E. A review of computer‑aided design/computer‑aided manufacture techniques for removable denture fabrication. Eur J Dent. 2016;10:286-91.
5. Sun J, Zhang FQ. The application of rapid prototyping in prosthodontics. J Prosthodont . 2012;21:641‑4.
6. Torabi K, Farjood E, Hamedani S. Rapid Prototyping Technologies and their Applications in Prosthodontics, a Review of Literature. J Dent (Shiraz). 2015;16:1‑9.
7. Kim SY, Shin S, Lee JH. Effect of cyclic bend loading on a cobalt‑chromium clasp fabricated by direct metal laser sintering. J Prosthet Dent. 2018;119:1027.e1‑7.
8. Mansour M, Sanchez E, Machado C. The use of Digital Impressions to fabricate Tooth‑Supported Partial Removable Dental Prostheses: A Clinical Report. J Prosthodont . 2015;25:495‑7.
9. Bajunaid SO, Altwaim B, Alhassan M, Alammari R. The Fit Accuracy of Removable Partial Denture Metal Frameworks Using Conventional and 3D Printed Techniques: An In Vitro Study. J Contemp Dent Pract. 2019;20:476‑81.
10. Soltanzadeh P, Suprono MS, Kattadiyil MT, Goodacre C, Gregorius W. An In Vitro Investigation of Accuracy and Fit of Conventional and CAD/CAM Removable Partial Denture Frameworks. J Prosthodont . 2019;28:547‑55.
11. Eggbeer D, Bibb R, Williams R. The computer‑aided design and rapid prototyping fabrication of removable partial denture frameworks. Proc Inst Mech Eng H. 2005;219:195‑202.
12. Alifui‑Segbaya F, Williams R, George R. Additive Manufacturing: A Novel Method for Fabricating Cobalt‑Chromium Removable Partial Denture Frameworks. Eur J Prosthodont Rest Dent. 2017;25:73-8.
�
Joana Paulos Cabrita
Correio eletr�nico: joanacabrita@campus.ul.pt
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
1646-2890/� 2021 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
