
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (1) | 42-49
Case report
Oral findings in Coffin-Siris syndrome: A case report
Abordagem odontológica na síndrome de Coffin Siris: Relato de caso
a Dental School, Federal University of Amazonas, Manaus, Amazonas, Brazil
Emílio Carlos Sponchiado Júnior - spemilio@ufam.edu.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 1
Case report
Pages - 42-49
Go to Volume
Article History
Received on 18/08/2020
Accepted on 11/03/2021
Available Online on 26/03/2021
Keywords
Case Report
�
Oral findings in Coffin-Siris syndrome: A case report
Abordagem odontol�gica na s�ndrome de Coffin Siris: Relato de caso
�
Heliton Siqueira Figueiraa, Pollyanna Oliveira Medinaa, Giorge Pessoa de Jesusa, Aida Ren�e Assayag Hanana, Em�lio Carlos Sponchiado J�niora*, Simone Assayag Hanana
aDental School, Federal University of Amazonas, Manaus, Amazonas, Brazil�
�
Article history:
Received 18 August 2020
Accepted 11 March 2021
Available online xx March 2021
�
AbstractThis paper reports the oral health approach of a child with Coffin-Siris syndrome. This syndrome is a multisystem congenital anomaly caused by mutations in genes of BRG- 1-associated factors complex. Individuals with this syndrome have been described with hypoplasia or aplasia of the fifth digit nails or phalanges. Other features include growth deficiency, developmental and intellectual delay, and other organ-system abnormalities. Clinical examination revealed gingival hyperplasia in the upper arch, dental biofilm, and dental caries on the lower deciduous and permanent molars. Guidelines on oral hygiene and dietary habits were provided to the guardians, and tooth extraction and restoration with glass-ionomer cement were performed. This case suggests that these patients require home care and periodic dental consultations for preventive and systematic dental treatment and quality of life improvement. The patient is being monitored, and her oral condition has improved.
Keywords: Case report,Coffin-Siris syndrome,Dental care for children,Fifth-digit syndrome
�
Resumo
Este artigo relata a abordagem da sa�de oral de uma crian�a com a s�ndrome de Coffin Siris. Esta s�ndrome � uma anomalia cong�nita multi-sist�mica causada por muta��es em genes do complexo BRG-1. Os indiv�duos com esta s�ndrome apresentam hipo ou aplasia das unhas ou das falanges do quinto dedo. Outras caracter�sticas incluem defici�ncia de crescimento, atraso de desenvolvimento intelectual e anormalidades do sistema de �rg�os. O exame cl�nico revelou hiperplasia gengival na arcada superior, presen�a de biofilme e c�rie dent�ria nos molares dec�duos e permanentes inferiores. Orienta��es sobre higiene oral e h�bitos alimentares foram fornecidas aos respons�veis, al�m da extra��o e restaura��o dos dentes com cimento de ion�mero de vidro. Este caso sugere que esses pacientes necessitam de atendimento domiciliar e consultas odontol�gicas peri�dicas para tratamento preventivo e sistem�tico para que se alcance a melhoria da qualidade de vida. A paciente est� sendo monitorizada e sua condi��o oral melhorou.
Palavras-chave: Relato de caso,S�ndrome de Coffin Siris,Tratamento odontol�gico de crian�as,S�ndrome do quinto d�gito
�
Introduction
Coffin-Siris syndrome (CSS), also known as the fifth-digit syndrome, was described in 1970 as a rare genetic disease.1 Since its first report in the literature, approximately 200 individuals were described worldwide with CSS;2 however, its prevalence and features have not been thoroughly investigated.3 It is characterized by intellectual disability, microcephaly, coarse facial features, cleft lip and palate, short stature, ectodermal defects (hypertrichosis, hirsutism, sparse hair, and dental anomalies), scoliosis, loose joints, and hypoplastic fifth-digit nails. It may also be accompanied by respiratory tract infections, hearing loss, congenital heart defects, ophthalmic anomalies, and feeding difficulties. During growth, the affected individual shows motor and language delay.1, 4, 5
CSS�s etiology has not yet been fully established, but it may be related to possible autosomal dominant or recessive inheritance.6 Recently, mutations in the genes encoding the BRG1-associated factor (BAF) chromatin-remodeling complex (also known as the SWI/SNF-A complex), such as ARID1A, ARID1B, ARID2, SMARCB1, SMARCA4, and SMARCE1, have been pointed out as the cause of the syndrome. Mutations in the ARID1B gene have been accounted for 76% of mutations that cause mild phenotypes.2, 7 - 9 The SOX11 gene, which participates in the transcriptional regulation of the BAF complex and plays an important role in neurodevelopment, has also been identified.10 It is more prevalent in females, in a ratio of 4:1, although clinical characteristics are similar in both sexes.1
Currently, the diagnosis of CSS is based on clinical findings.4 The combination of characteristics such as coarse facial features, hypoplasia of the fifth-digit nail, and development delay suggests the presence of the syndrome.6 It has become important to rule out disorders that present with similar clinical characteristics, such as the Coffin-Lowry and Cornelia de Lange syndromes.4
Due to the syndrome�s low frequency, diversity of symptoms, �and variability, definitive diagnosis is difficult.11 Since dental management of these patients is not widely discussed in the literature, knowledge and identification of its main clinical and oral manifestations, such as delayed dentition, presence of crowding or diastemas, and atypical dental defects, is of great importance to establish an early diagnosis and rehabilitation, as well as family referral to genetic services.12
Dental treatment of these patients must consider the degree of intellectual disability, clinical oral manifestations, such as possible cardiovascular anomalies, and oral impact and influence of possible medications. The literature gap of studies on the dental treatment approach in individuals with this syndrome is noteworthy. The present study reports a case of a patient with CSS submitted to dental treatment.
Case Report
The authors obtained written informed consent from the patient�s parents. This study is reported following the CARE guidelines (The CAse REport guidelines).13
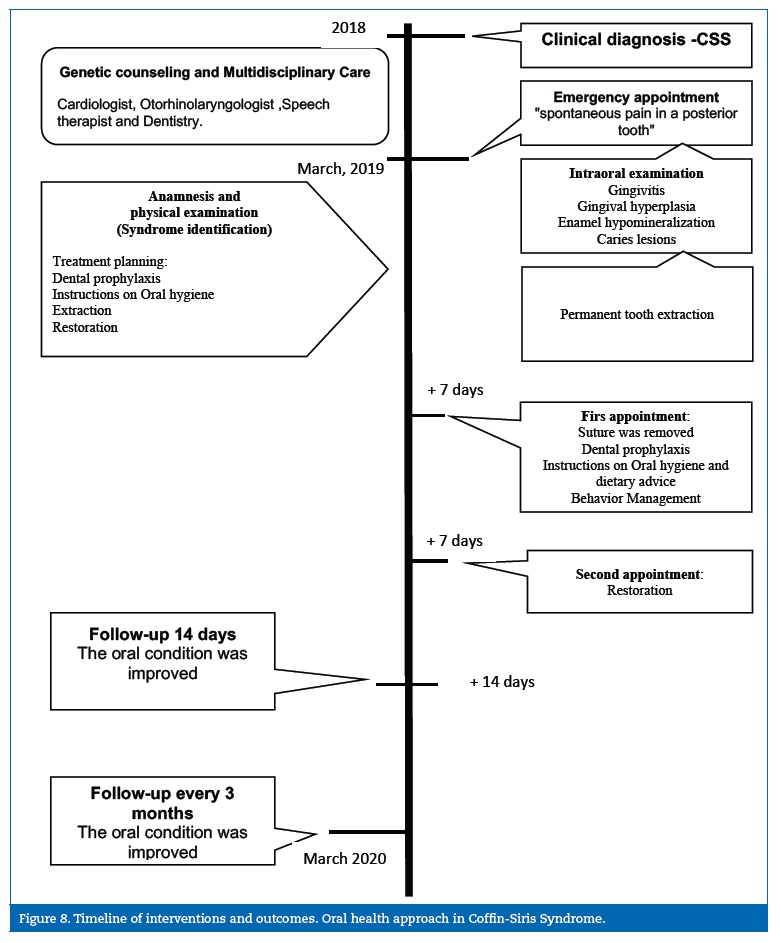
An eight-year-old female patient diagnosed with CSS sought treatment at the School of Dentistry�s outpatient clinic, accompanied by her father, with the main complaint of spontaneous pain in a posterior tooth. During anamnesis, her father reported that the geneticist had referred the child to dental treatment and that she was born with physical deformities, moderate mental retardation, and frequent upper respiratory tract infections. The patient had also been diagnosed with an atrial septal defect, repaired without residual shunts.
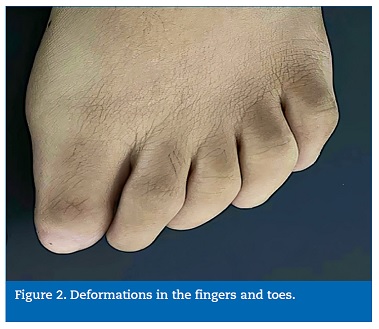
She had not been on any continuous medication. The patient had undergone genetic counseling, and the clinical diagnosis was CSS. She had also been referred to a cardiologist, otorhinolaryngologist, and speech therapist. Her clinical profile included the three most frequent clinical findings of CSS and at least one of each of the three least prevalent categories (Table 1). She was not submitted to molecular examination for diagnostic confirmation due to its high cost and restricted access by the public health service.
�
�
There was no history of consanguinity between the parents, and the patient was the oldest of the couple�s two daughters. In the gestational history, there were no reports of complications nor use of alcohol or drugs. She was born at term with low weight for gestational age (1,950 kg) and an Apgar score of 6/10 (5th minute). Her growth deficiency was apparent.
Regarding previous dental history, her mother reported that it was her daughter�s first visit to the dentist and that she consumed sugar food once to twice a week.
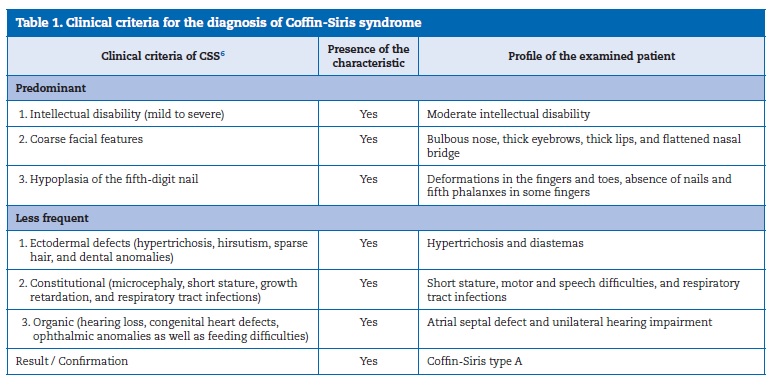
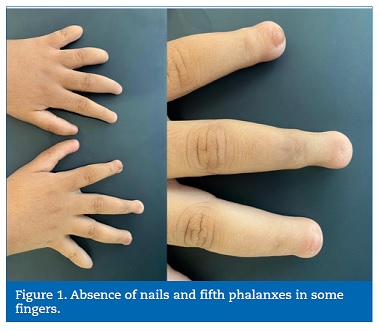
Physical examination revealed deformations in the fingers and toes, absence of nails and fifth phalanxes in some fingers (Figures 1 and 2), motor and speech difficulties, high palate, short stature, and unilateral hearing loss. Radiographic examination of the hands and wrists revealed that the patient presented a delay in bone age. On extraoral examination, facial features typical of the syndrome were observed, such as a bulbous nose, thick eyebrows, hypertrichosis, thick lips, and flattened nasal bridge (Figure 3).
�
�
�

�
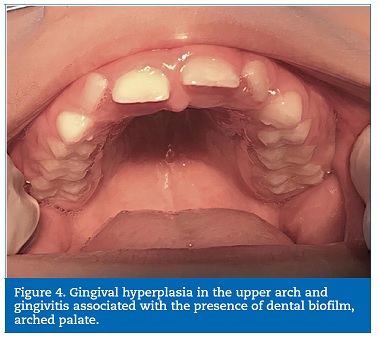
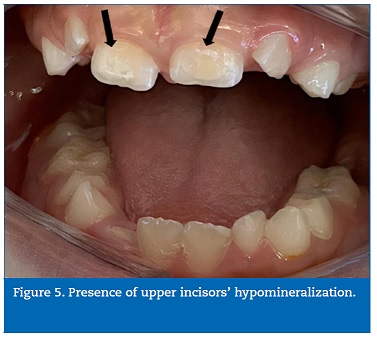
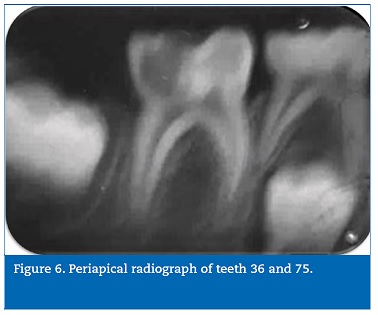
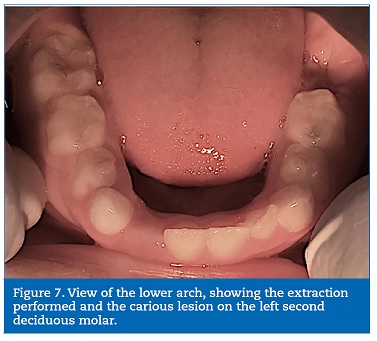
Intraoral examination revealed the presence of gingival hyperplasia in the upper arch and gingivitis associated with the presence of dental biofilm, arched palate, Angle class I occlusion without crossbite or open bite, dolichofacial pattern, labial hypotonia, and mild enamel hypomineralization (presence of whitish-cream demarcated opacities)14 in the permanent maxillary central incisors (Figures 4 and 5). Moreover, she had caries lesions in the deciduous mandibular left second molar and mandibular first permanent molar, which presented great coronary destruction and pulp involvement (Figures 6 and 7).
�
�
�
�
�
No demarcated opacities, enamel breakdown, or atypical restorations were observed in the patient�s other first permanent molars. Still, the tooth extraction might have been due to molar incisor hypomineralization (MIH), based on the judgment criteria for MIH diagnosis proposed for prevalence studies, where one of the criteria to diagnose �Suspected for extraction due to MIH� is the absence of the first permanent molars in a sound dentition in combination with demarcated opacities on the incisors.15
Periapical radiography of the affected teeth was performed.
Bitewing radiographs were impossible to make due to the patient�s uncooperative behavior and reduced mouth opening.
The patient used a Kinesio tape (elastic bandage) around the lips to increase the lip muscles� motor function, improving lip sealing, mouth opening, and speech.
Treatment planning included a multidisciplinary approach and involved the extraction of the permanent first molar and restoration of the deciduous tooth�s occlusal surface using light-curing glass-ionomer cement (GIC). An orthodontic evaluation was conducted in the preservation consultation, but due to the patient�s cognitive delay (difficulty to mechanically control biofilm), orthodontic therapy was not indicated.
The patient cried a lot and manifested non-collaborative behavior. Because this was an emergency appointment due to the child�s pain, who had been having difficulty eating and sleeping for days, the permanent tooth extraction was performed at the first visit. Protective stabilization with active immobilization, involving restraint by her parents and dental auxiliary, was performed to minimize the psychological stress and/or decrease the risk of physical injury to the patient, the parents, and the staff. Alternative behavioral approaches to reduce movement and resistance and increase cooperation when providing dental care for special-needs patients, such as distraction, shaping, modeling, and reinforcement, were used prior to implementing protective stabilization.
Intraoral antisepsis was performed using 0.12% chlorhexidine digluconate (Periogard�, Sao Paulo, SP, Brazil) for one minute, followed by extraoral antisepsis with 2% chlorhexidine digluconate (Riohex Gard�, Rioquimica, Sao Jose do Rio Preto, SP, Brazil). After topical anesthesia, the lower alveolar and buccal nerve was blocked using 2% lidocaine + epinephrine 1:100.00 (Alphacaine�, Nova DFL, Taquara, RJ, Brazil), followed by syndesmotomy.
Subsequently, odontosection was performed in the tooth�s buccal-lingual direction using a tapered drill (KG Sorensen, Cotia, SP, Brazil). The roots were removed using #151 dental forceps (Quinelato, Rio Claro, SP, Brazil). The alveolar cavity was irrigated with 0.9% saline (Tayuyna Laboratory, Nova Odessa, SP, Brazil) and suture was performed using 4.0 silk thread (Sertix�, Shalon Fios Cirurgicos, Sao Luis de Montes Belos, GO, Brazil). After the surgery, analgesics and antibiotics were prescribed, and the mother was instructed on feeding, hygiene, and supervision to prevent the child from biting her lips involuntarily.
At the second appointment, the suture was removed, and further instructions on oral hygiene and dietary advice were provided. The patient was still withdrawn and non-cooperative.
Behavior guidance techniques, such as modeling and positive reinforcement, were used to alleviate anxiety and nurture a positive dental attitude. Dental prophylaxis was performed using Clinpro� toothpaste (3M, Sao Paulo, SP, Brazil) to condition behavior for the next dental appointment for primary tooth restoration. Four applications of fluoride varnish (DuraphatTM, Colgate-Palmolive Ind. and Com. Ltda, Sao Paulo, SP, Brazil), one per week, were planned for enhancing remineralization of the permanent incisors.
The patient returned seven days later to restore her deciduous mandibular second molar�s occlusal surface with encapsulated resin-modified GIC using relative isolation (Riva Light Cure�, SDI Brasil Industria e Comercio Ltda., Sao Paulo, SP, Brazil). An improvement in the child�s behavior was observed, with no need for the father to be present in the clinic or physical restraint to carry out the treatment proposed. In this appointment, the cooperative behavior was reinforced again.
Two weeks after hygiene and dietary guidance, improvement in biofilm formation and gingival tissue was observed. The patient is under follow-up, with quarterly returns scheduled to improve her and her family�s quality of life. A follow-up individualized preventive program was established involving parents� education to ensure appropriate daily oral hygiene and diet and accompany the left mandibular second permanent molar eruption. The timeline of interventions and outcomes is presented in Figure 8.
�
�
Discussion and Conclusions
CSS is a rare multiple congenital anomaly associated with mutations in BAF complex genes.2, 7, 8 These mutations are linked to a broad range of diseases that, according to the gene affected, range from non-syndromic or syndromic neurodevelopmental disorders to low-grade tumors and malignancies.16 Therefore, this case report�s patient is undergoing genetic monitoring to investigate the genotype and diagnose possible molecular mutation.
The diagnosis of this condition is based on the presence of the most frequent clinical characteristics, and the role of genetic evaluation is to complement diagnosis.4 Due to the absence of molecular tests, it was hypothesized that the patient had CSS type A based on Schrier et al.�s clinical criteria.6 These criteria require the presence of three predominant clinical findings and at least one of each of the three categories of the syndrome�s less frequent clinical characteristics. These characteristics were found in our clinical case, similar to another study conducted in India.4 Due to the reported prevalence of various findings, �classic� clinical characteristics will not always be present to support such a diagnostic strategy; thus, next-generation molecular sequencing techniques are required to confirm the diagnosis of CSS.
Fifth-digit hypoplasia/aplasia, a characteristic that gives the syndrome its name, may not be evident in some cases of CSS. Although the presence of �classic� characteristics can alert the clinician to suspect the presence of CSS, the wide phenotype variability suggestive of the absence of these characteristics does not exclude the possibility of CSS.2
The management and dental treatment of syndromic patients vary according to the needs of each individual affected, and it is important to promptly detect the disease to enable early treatment and promote good development of the child�s general and oral health.17 Our oral findings were not consistent with some previously described findings, such as delayed eruption, macroglossia, micrognathia, and the occurrence of cleft lip and palate and conoid teeth.1, 6 However, high palate and diastema were observed,2 which may denote the genetic heterogeneity of the disorder since the phenotype is genotype-dependent.5
Abnormal growth of gingival tissue has been observed in patients with several syndromes and, when associated with hypertrichosis, may denote the presence of CSS.18 Although gingival growth�s pathogenesis is still unknown,19 it has been recognized to be multifactorial and caused by gingival fibroblast dysfunction.
Gingival hyperplasia or hypertrophy makes it difficult to maintain oral hygiene and, often, masticatory function, leading to bacterial biofilm accumulation.20 Conservative prophylactic periodontal therapy associated with oral hygiene instructions can be used to treat gingival hyperplasia. In the present case, after professional prophylaxis and guidance on oral hygiene habits, the clinical condition improved in 2 weeks. Patients with gingival hyperplasia should be carefully monitored and advised about the need for thorough oral hygiene.21
The presence of caries and gingivitis are common findings, and their severity can be attributed to the patient�s cognitive impairment.22 Motor and behavioral difficulties make dental treatment difficult. In this case, non-pharmacological behavioral techniques were used, such as tell-show-do, positive reinforcement, and protective stabilization. Parents and caregivers of children with mental disabilities can help manage these patients in the dental office. Protective stabilization to ensure safety during procedures can be useful for patients when behavioral management techniques fail.17
The fluoride varnish use in a patient with hypomineralization is essential to increase calcium and fluoride ion release and control dental caries development.16 Moreover, the use of fluoride varnish is important to prevent enamel breakdown and control the hypersensitivity associated with the hypomineralization.23
We opted for the extraction of the mandibular first permanent molar because the child�s behavior would not have allowed endodontic treatment followed by placement of a stainless-steel or similar crown, which could be replaced by a porcelain crown at an older age.24 Root canal therapy requires rubber dam isolation, extended working time, radiographic acquisition, and substantial cooperation, all of which might prove challenging to non-collaborative individuals with special needs.25 Operative dental treatments, especially complex restorations and root canal therapy, are time-consuming and require patient compliance; therefore, dentists must tend to provide tooth extraction if patients with specific disabilities do not have cooperative behavior due to their developmental delay.26
GICs combine fluoro-alumina silicate glass and polyalkenoic acids. Resin-modified glass ionomers share this same chemistry but with additional resin, which reinforces the material and adds an aesthetic dimension. Used widely worldwide as definitive restorative materials for deciduous teeth, the resin-modified GICs present mechanical properties compatible with composite resins, being as efficient as the conventional technique.27 Besides offering favorable work time, easy application, and release fluoride, another advantage of GICs is that their longevity is not influenced by the use of a dental dam, making its use even easier, both in children and special-needs patients. Providing increased aesthetics and strength, the indications for resin-modified glass ionomers are non-stress bearing class I (as in this clinical report) or II restorations for deciduous teeth. The encapsulated GICs present superior resistance to compression compared to the powder/liquid system because the proportions are pre-balanced in the factory.28
The use of restorations with fluoride-releasing materials, such as GICs, can be a useful therapeutic and preventive approach for patients with special needs,17 in which we have difficulty maintaining a dry field or must work very quickly.
These patients require home care and periodic dental consultations for preventive and systematic dental treatment. Patients with several dental diseases may need to be seen every two to three months, or more often if indicated.13 In this case report, the patients� father, responsible for her, very clearly reported the improvement in the patient�s quality of life after dental treatment.
There is no report of dental care in a patient with this syndrome in the literature, making it difficult to compare the obstacles encountered and the protocols adopted in the present case report. CSS has a variable expression in different individuals.
For the patient described in our report, dental treatment was possible using non-pharmacological behavior management techniques. In individuals who are less cooperative or need more extensive treatment, pharmacologic techniques, such as conscious sedation or general anesthesia, might be necessary.
The dental surgeon�s knowledge of CSS�s clinical characteristics will lead to the early diagnosis of oral problems and improve the quality of life of the syndromic patient. The patient is being monitored, and her oral conditions have improved.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest. The authors have no conflicts of interest to declare.
�
References
1. Ordonez MPT, Oyervide JAJ. Sindrome de Coffin-Siris. Rev Fac Cienc Med Univ Cuenca. 2016;34:69-75.
2. Mannino EA, Miyawaki H, Santen G, Vergano SAS. First data from a parent-reported registry of 81 individuals with Coffin-Siris syndrome: Natural history and management recommendations. Am J Med Genet A. 2018;176:2250-8.
3. Curcio MR, Ferranti S, Lotti F, Grosso S. Coffin-Siris syndrome and epilepsy. Neurol Sci. 2020.
4. Nemani L, Barik R, Patnaik AN, Mishra RC, Rao AM, Kapur P. Coffin-Siris syndrome with the rarest constellation of congenital cardiac defects: A case report with review of literature. Ann Pediatr Cardiol. 2014;7:221-6.
5. Vergano SS, Deardorff MA. Clinical features, diagnostic criteria, and management of Coffin-Siris syndrome. Am J Med Genet C Semin Med Genet. 2014;166C:252-6.
6. Schrier SA, Bodurtha JN, Burton B, Chudley AE, Chiong MA, D�Avanzo M G, et al. The Coffin-Siris syndrome: a proposed diagnostic approach and assessment of 15 overlapping cases. Am J Med Genet A. 2012;158A:1865-76.
7. Sonmez FM, Uctepe E, Gunduz M, Gormez Z, Erpolat S, Oznur M, et al. Coffin-Siris syndrome with cafe-au-lait spots, obesity and hyperinsulinism caused by a mutation in the ARID1B gene. Intractable Rare Dis Res. 2016;5:222-6.
8. Vasileiou G, Vergarajauregui S, Endele S, Popp B, Buttner C, Ekici AB, et al. Mutations in the BAF-Complex Subunit DPF2 Are Associated with Coffin-Siris Syndrome. Am J Hum Genet. 2018;102:468-79.
9. Boerstler T, Wend H, Krumbiegel M, Kavyanifar A, Reis A, Lie DC, et al. CRISPR/Cas9 mediated generation of human ARID1B heterozygous knockout hESC lines to model Coffin-Siris syndrome. Stem Cell Res. 2020;47:101889.
10. Okamoto N, Ehara E, Tsurusaki Y, Miyake N, Matsumoto N. Coffin-Siris syndrome and cardiac anomaly with a novel SOX11 mutation. Congenit Anom (Kyoto). 2018;58:105-7.
11. Kosho T, Miyake N, Carey JC. Coffin-Siris syndrome and related disorders involving components of the BAF (mSWI/SNF) complex: historical review and recent advances using next generation sequencing. Am J Med Genet C Semin Med Genet. 2014;166C:241-51.
12. Khan U, Study D, Baker E, Clayton-Smith J. Observation of Cleft Palate in an Individual with SOX11 Mutation: Indication of a Role for SOX11 in Human Palatogenesis. Cleft Palate Craniofac J. 2018;55:456-61.
13. Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. 2017;89:218-35.
14. Ghanim A, Silva MJ, Elfrink MEC, Lygidakis NA, Marino RJ, Weerheijm KL, et al. Molar incisor hypomineralisation (MIH) training manual for clinical field surveys and practice. Eur Arch Paediatr Dent. 2017;18:225-42.
15. Weerheijm KL, Duggal M, Mejare I, Papagiannoulis L, Koch G, Martens LC, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110-3.
16. Holsten T, Bens S, Oyen F, Nemes K, Hasselblatt M, Kordes U, et al. Germline variants in SMARCB1 and other members of the BAF chromatin-remodeling complex across human disease entities: a meta-analysis. Eur J Hum Genet. 2018;26:1083-93.
17. Dentistry AAoP. Guideline on Management of Dental Patients with Special Health Care Needs. Pediatr Dent. 2016;38:171-6.
18. Bubna AK, Veeraraghavan M, Anandan S, Rangarajan S. Congenital Generalized Hypertrichosis, Gingival Hyperplasia, a Coarse Facies with Constriction Bands: A Rare Association. Int J Trichology. 2015;7:67-71.
19. Bharti V, Bansal C. Drug-induced gingival overgrowth: The nemesis of gingiva unravelled. J Indian Soc Periodontol. 2013;17:182-7.
20. Trackman PC, Kantarci A. Molecular and clinical aspects of drug-induced gingival overgrowth. J Dent Res. 2015;94:540-6.
21. Hatahira H, Abe J, Hane Y, Matsui T, Sasaoka S, Motooka Y, et al. Drug-induced gingival hyperplasia: a retrospective study using spontaneous reporting system databases. J Pharm Health Care Sci. 2017;3:19.
22. Pini DM, Frohlich PC, Rigo L. Oral health evaluation in special needs individuals. Einstein (Sao Paulo). 2016;14:501-7.
23. Restrepo M, Jeremias F, Santos-Pinto L, Cordeiro RC, Zuanon AC. Effect of Fluoride Varnish on Enamel Remineralization in Anterior Teeth with Molar Incisor Hypomineralization. J Clin Pediatr Dent. 2016;40:207-10.
24. Wasersprung D, Sarnat H. Coffin-Lowry syndrome: findings and dental treatment. Spec Care Dentist. 2006;26:220-4.
25. Alsaleh I, Cousson PY, Nicolas E, Hennequin M. Is endodontic treatment performed under general anaesthesia technically acceptable? Clin Oral Investig. 2012;16:1599-606.
26. Lin PY, Wang KW, Tu YK, Chen HM, Chi LY, Lin CP. Dental service use among patients with specific disabilities: A nationwide population-based study. J Formos Med Assoc. 2016;115:867-75.
27. Taha NA GA, Tavangar MS. Comparison of Mechanical Properties of Resin Composites with Resin Modified Glass Ionomers. J Dent Biomater. 2015;2:47-53.
28. Avelino ELLdC, Nogueira CdOP, Dorini AL, Caldas SGFR, Galvao MR. Comparacao da resistencia a compressao entre o cimento de ionomero de vidro encapsulado e o sistema po/liquido. RFO UPF. 2016;21:191-5.
�
Em�lio Carlos Sponchiado J�nior
E-mail address: spemilio@ufam.edu.br
