
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2020 | 61 (2) | 72-78
Case report
Treatment of vascular malformation with the surgical diode laser: Clinical case
Tratamento de malformação vascular labial com o laser de díodo cirúrgico: Caso clínico
a Dentist, Private Dental Practice, Lochau/Lake Constance, Austria
b Faculty of Dental Medicine, University of Porto, Oporto, Portugal
c Dental Division, University of Guarulhos, Guarulhos – SP, Brazil
Cristina Fonte - acristinafonte@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 61
Issue - 2
Case report
Pages - 72-78
Go to Volume
Article History
Received on 26/09/2019
Accepted on 03/07/2020
Available Online on 01/09/2020
Keywords
Case report
�
Treatment of vascular malformation with the surgical diode laser: Clinical case
Tratamento de malforma��o vascular labial com o laser de d�odo cir�rgico: Caso cl�nico
�
Ingrid Baaken-Buchriesera, Jo�o Bragab, Cristina Fonteb,*, L�cio Frigoc, Elisabete Barbosab, Filipe Coimbrab
a Dentist, Private Dental Practice, Lochau/Lake Constance, Austria
b Faculty of Dental Medicine, University of Porto, Oporto, Portugal
c Dental Division, University of Guarulhos, Guarulhos � SP, Brazil
�
�
http://doi.org/10.24873/j.rpemd.2020.09.701
�
Abstract
The objective of this study is to present a clinical case of a hemangioma of the lower lip successfully treated by diode laser. A vascular malformation occupying the entire red zone of the lower right lip, including the inner face, up to the midline, of a 12-year-old patient, was excised in two sessions with a diode laser (GaAl) of 980 nm with fiber tips of O 400 μm.
Total re-epithelization of the wound was achieved in approximately 21 to 30 days. No postoperative pain occurred, and the functional and aesthetic results were good. The use of diode laser in oral vascular anomalies can be considered a good treatment option.
Keywords: Diode laser, Laser excision, Laser incision, Laser surgery, Oral hemangioma, Wound healing
�
Resumo
O objetivo deste estudo � apresentar um caso cl�nico de hemangioma do l�bio inferior tratado com sucesso, por laser de d�odo. Paciente com 12 anos de idade com malforma��o vascular ocupando toda a zona vermelha do l�bio inferior direito incluindo a face interna at� � linha m�dia. O tratamento cir�rgico foi efetuado em 2 sess�es com o laser de d�odo (GaAl) de 980 nm com fibra descart�vel (fiber tips) de � 400 μm. Houve reepiteliza��o total das feridas em aproximadamente 21 a 30 dias. N�o ocorreu dor p�s-operat�ria e o resultado funcional e est�tico foi bom. O uso do laser de d�odo nas anomalias vasculares orais pode ser considerado uma boa op��o de tratamento.
Palavras-chave: Laser de d�odo, Excis�o com laser, Incis�o com laser, Cirurgia a laser, Hemangioma oral, Cicatriza��o de feridas
�
Introduction
A vascular anomaly is any lesion of congenital or acquired etiology whose major components are vascular structures.1, 2
The classification of vascular anomalies proposed in 1996 by the International Society for the Study of Vascular Anomalies (ISSVA) divides vascular anomalies into two categories: vascular tumors (including hemangioma) and vascular malformations.2, 3 Hemangioma is the most common benign vascular tumor in the child,4 usually appearing soon after birth or in early childhood. It is 3 to 5 times more predominant in females than in males and is also more common in Caucasians.
The existing treatments for vascular anomalies are chemical sclerosis, physical sclerosis, and laser excision.2, 5 Diode laser, also called injection or semiconductor laser, was first introduced in Europe in 1990 at the International Congress of Oral Medicine in Cologne, Germany, and approved by the USA Food and Drug Administration (FDA) in 1993. The wavelength of the diode laser emits energy that is absorbed mainly by hemoglobin, allowing precise cutting, with vaporization, hemostasis, and coagulation of vascular tissue with or without contact. There is no need for suturing, and postoperative edemas are scarce or nonexistent.6, 7
In this study, we present the results of the treatment of a labial hemangioma with surgical diode laser.
Case report A 12‑year‑old Caucasian female patient attended a consultation at the Department of Oral Medicine of the Faculty of Dental Medicine of the University of Porto. The main complaint was the aesthetic alteration in her right lower lip, with increased volume and altered function. Her parents reported that the onset of the alteration was after falling from her crib at 7 months of age. Clinical examination revealed a bluish swelling of soft consistency, painless to palpation, on the lower lip mucosa, measuring 25x20x10 mm and occupying half of the right lower lip (Figures 1, 2, 3, 4).
�

�

�

�

�
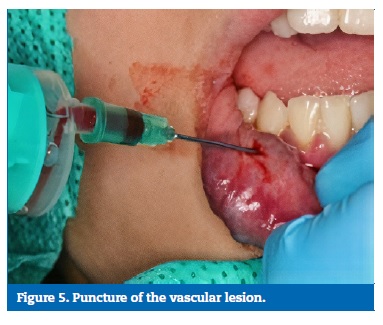
A vascular lesion with positive diascopy was clinically suspected, and the malformation was punctured for confirmation (Figure 5). Upon insertion of the needle, there was a slight inflow of blood into the syringe, suggesting low blood flow in the lesion. The preoperative lesion area was photographed and measured with a digital ruler (150 mm, Fischer Darex). The patient�s parents signed an informed consent form in accordance with the Helsinki Declaration.
�
The operative field was prepared by performing extraoral antisepsis with 0.2% chlorhexidine and intraoral with 0.12% chlorhexidine (Bexident, ISDIN) for 45 seconds. A 980‑nm diode laser device (Schmidt & BenderR, Budapest, Hungary) was used for lesion excision, following the protocol recommended by the manufacturer.
The treatment was performed in two sessions. After local anesthesia with 2% lidocaine (Xilonibsa 1:80,000, Inibsa), we approached the tumor on the inner side of the lip. This first session began by following the contour of the lesion with 2.0 W (Figure 6), and then increasing to 2.5�3.0 W in continuous mode for excision, with a 400‑μm disposable fiber applied to the mucosa at an angle of 45 degrees (Figure 7). During the passage of the fiber, visible bleaching and tissue retraction were observed (Figure 8). The fiber remained in close contact with the tissue and was slowly moved around the lesion. The deeper area of the epithelium showed bleeding, which was coagulated with a second passage of the fiber on the capillary from where the bleeding came, with the following parameters: 2.0 W, in contact, continuous mode.
�

�

�

The specimen was removed with a safety margin of approximately 1 mm and sent for histological analysis (Figure 9).
�

�
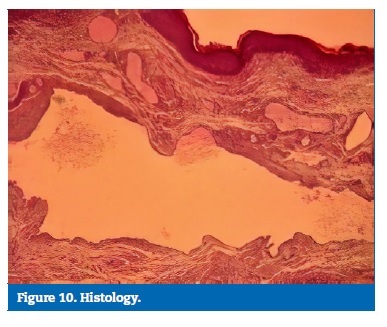
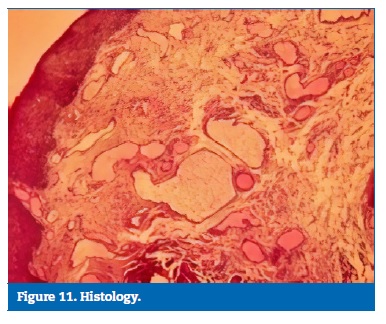
The result confirmed the clinical diagnosis of vascular hemangioma (Figures 10, 11). The wound was left open for healing by second intention, without the use of any surgical cement. Postoperative care included the application of a 0.2% chlorhexidine gel (Bexident Post Gel, ISDIN) on the wound.
�
�
�
In the second session of the treatment, we approached the red zone of the lip, using the same parameters as in the first session (Figure 12). An SPF 50 cream (Avene) was applied to the labial mucosa sensitive areas for 21 days to 3 months after surgery. The patient was followed up 30 days post‑surgery.
�

�
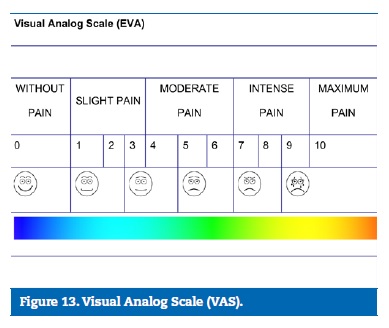
In the first three days after surgery, a pain evaluation scale was applied, standardized with a visual analog scale (VAS) (Figure 13). Following the instructions for use provided to the patient, she had to draw a cross at the point of maximum pain intensity.
�
�
Shortly after the surgery, a scorched area of carbonized and edematous tissue was observed. By the third day, no visible areas of carbonized tissue were detected. The lesions were well delimited with some necrotic material covering the wound. It was still possible to observe discrete edema. One week later, there was an immature scar with regions of coloration similar to the normal mucosa (Figure 14). The wound cavity was irregular, covered by granulation tissue. In the second week (11‑14 days), the reabsorption of damaged tissue particles was complete (Figure 15). For 21 to 30 days, a clear and whitish scar remained along the surgical site (Figure 16), and after 3 months the scar was almost imperceptible (Figure 17).
�

�

�

�

Discussion and Conclusions
We chose the diode laser for this treatment due to its easy handling for cutting and coagulation procedures.8 The novelty of this case is the use of fiber tips that are easily attached to the handpiece with no cladding plastic. Also, we used a wavelength of 980 nm, as it offers a 10‑times higher water absorption than the 810‑nm one,9 presenting better cutting properties.
As it passes through the tissue, the laser beam generates heat and coagulates the tissue to a depth of about 7 to 10 mm, occurring selective photothermolysis.10
In this clinical case, the patient had a marked aesthetic, anatomical, and functional impairment of the perioral anatomy. There was also the risk of possible local trauma and subsequent bleeding. The patient had visited several health professionals looking to solve the lip problem that affected her aesthetics and compromised socialization. She had not obtained positive answers, and the justification was always that classic surgery could leave irreversible scars and cause extensive hemorrhage.
Hemangiomas and vascular malformations have the appearance of blood‑filled blisters or reddish, bluish, or purplish spots.11, 12 In cases where there is increased blood flow velocity, they are pulsatile, have a higher temperature than adjacent tissues, and tend to increase � up to several centimeters � with decubitus position, crying, coughing, vomiting, or hypertension.1, 5 In this case, there was no history of spontaneous bleeding.
The diagnosis can be made based on the clinical aspect and using a diascopy and puncture maneuver, which, if the lesion is arterial, causes retraction of the plunger of the syringe.1, 5 The present case agrees with reports by Neville et al.1 that capillary hemangiomas originate from trauma. Histologically, the hemangioma presents as a proliferation of large numbers of small blood vessels coated by a single layer of endothelial cells and separated by septa of connective tissue.13
In our case, the histology was compatible with capillary hemangioma.
According to several authors,14 ‑ 17 laser excision is the first option among several alternative techniques in the treatment of these lesions. In a study to evaluate the efficacy of treatment of oral hemangiomas with diode laser‑induced photocoagulation, the authors suggested that lesions larger than 2.5 cm should be treated in two sessions.14
Our results were similar to those of other authors8, 18, 19 who evaluated and compared the degree of postoperative pain, discomfort, and functional complications of patients submitted to oral soft‑tissue laser treatments. On the first three postoperative days after the first phase, the patient reported no pain or mild pain (0, 1) without the need for analgesic. After the second phase of surgery, she reported mild pain (2, 3), and paracetamol 500 mg was taken every 8 hours in the first two days. On the third day, there was no pain, only complaint of aesthetic and functional discomfort.
We observed that, within three days of surgery, no areas of carbonized tissue were visible. The lesions were well delimited, with possible necrotic material covering the wound. On the first seven days post‑surgery, inflammation was evident and, at 14 days, the inflammatory process had already diminished, and all surgical wounds showed tissue repair with the formation of an immature scar. As observed previously, all surgical wounds were re‑epithelialized between three and four weeks post‑surgery.
At 3 months post‑surgery, the lip had a normal mucosa‑like appearance with no apparent scar. Some studies suggest the scarce number of myofibroblasts during healing as a possible explanation for the minimal degree of contraction of the wound after laser irradiation.20 ‑ 22 In contrast, after a conventional surgical excision, myofibroblasts occur in large quantities.
The excision of vascular lesions with diode laser provides better control of hemorrhage and reduced surgical time. The absence of sutures provides a more comfortable postoperative period, with less impairment of function. The wounds were fully reepithelialized in approximately 21 to 30 postoperative days. Postoperative pain was minimal or nonexistent.
�
References
1. Neville BW, Damm DD, Allen CM, Bouquot JE. Patologia Oral & Maxilofacial. 2nd ed. Rio de Janeiro: Guanabara Koogan; 2004. p.540‑5.
2. Shafer W, Hine M, Levy B. Tratado de Patologia Bucal. 4 ed. Rio de Janeiro: Guanabara Koogan; 1987. p.141‑2.
3. Fernandes DT, Elias RA, Santos‑Silva AR, Vargas PA, Lopes MA. Benign oral vascular lesions treated by sclerotherapy with ethanolamine oleate: A retrospective study of 43 patients. Med Oral Patol Oral Cir Bucal. 2018;23:e180‑7.
4. Zhang L, Wu HW, Yuan W, Zheng JW. Propranolol therapy for infantile hemangioma: our experience. Drug Des Devel Ther. 2017;11:1401-8.
5. Enjoras O, Wassef M, Chapot R. Color Atlas of Vascular Tumors Malformations. Cambridge: Cambridge University Press; 2009. p.2‑11.
6. Eliades A, Stavrianos C, Kokkas A, Kafas P, Nazaroglou I. 808 nm Diode Laser in Oral Surgery: A case report of laser removal of fibroma. Research Journal of Medical Sciences. 2010;4:175‑8.
7. Aras MH, Goregen M, Gungormus M, Akgul HM. Comparison of Diode Laser and Er: YAG Lasers in the Treatment of Ankyloglossia. Photomed Laser Surg. 2010;28:173‑7.
8. Taylor DL, Schafer SA, Nordquist R, Payton ME, Dickey DT, Bartels KE. Comparison of a high power diode laser with the Nd: YAG laser using in situ wound strength analysis of healing cutaneous incisions. Lasers Surg. 1997;21: 248‑54.
9. Jackson SD, Lauto A. Diode‑pumped fiber lasers: a new clinical tool?. Lasers Surg. 2002;30:184‑90.
10. Azevedo LH, Galletta VC, Eduardo CP, Migliari DA. Venous Lake of the Lips Treated Using Photocoagulation with High‑Intensity Diode Laser. Photomed Laser Surg. 2010;28:263‑5.
11. Queiroz S, Assis G, Silvestre V, Germano A, Silva J. Treatment of oral hemangioma with sclerotherapy: case report. J Vasc Bras. 2014;13:249‑53.
12. Portaro S, Naro A, Guarneri C, Toro G, Manuli A, Calabro R. Hemangiomas of the tongue and the oral cavity in a myotonic dystrophy type 1 patient. Medicine (Baltimore). 2018;97:e13448.
13. Katchburian E, Arana V. Histologia e embriologia oral. 2nd ed. Rio de Janeiro: Guanabara Koogan; 1999.
14. Angiero F, Benedicenti S, Romans G, Crippa R. Treatment of hemangioma of the head and neck with diode laser and forced dehydration with induced photocoagulation. Photomed Laser Surg. 2008;26:113‑8.
15. Genovese WJ, Santos MT, Faloppa F, Merli LA. The Use of Surgical Diode Laser in Oral Hemangioma: A Case Report. Photomed Laser Surg. 2010;28:147‑51.
16. Aciole GT, Aciole JM, Soares LG, Santos NR, Santos JN, Pinheiro AL. Surgical Treatment of Oral Lymphangiomas with CO2 laser: Report of two uncommon Cases. Braz Dent J. 2010;21:1‑7.
17. Akbulut N, Kursun ES, Tumer MK, Kamburoglu K, Gulsen U. Is the 810 nm diode laser the best choice in oral soft tissue therapy? Eur J Dent. 2013;7:207‑11.
18. Kara C. Evaluation of patient perceptions of frenectomy: a comparasion of Nd: Yag Laser and conventional techniques. Photomed Laser Surg. 2008;26:147‑52.
19. Haytac M, Ozcelik O. Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J Periodontol. 2006;77:1815‑9.
20. Fisher SE, Frame JW, Browne RM, Tranter RM. A comparative histological study of wound healing following CO2 laser and conventional surgical excision of buccal mucosal canine. Arch Oral Biol. 1983;28:287‑91.
21. Zeinoun T, Nammour S, Dourov N, Aftimos G, Luomanen M. Myofibroblasts in healing laser excision wounds. Lasers Surg Med. 2001;28:74‑9.
22. Ishii J, Kuriyama T, Komori T. Experimental study on the morphological and functional recovery following partial glossectomy in rabbits: a comparison between CO2 laser and electrocautery. Photomed Laser Surg. 2005;23:47‑51.
�
Cristina Fonte
E-mail address: acristinafonte@hotmail.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 26 September 2019
Accepted 3 July 2020
Available online 1 September 2020
