
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2019 | 60 (1) | 18-26
Case report
Endodontic management of developmental anomalies: conservation of invaginated tissues in Type II dens invaginatus – case series
Abordagem endodôntica de anomalias de desenvolvimento: conservação dos tecidos invaginados de dens invaginatus Tipo II – série de casos
a Department of Endodontics, Faculdade de Medicina Dentária, Universidade de Lisboa (University of Lisbon), Lisbon, Portugal
b Centro de Estudo de Medicina Dentária Baseada na Evidência, Faculdade de Medicina Dentária, Universidade de Lisboa (University of Lisbon), Lisbon, Portugal
c Department of Endodontics, Universitat Internacional de Catalunya (University of Catalunya), Barcelona, Spain
Mariana Domingos Pires - mariana.dpires@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 1
Case report
Pages - 18-26
Go to Volume
Article History
Received on 01/10/2018
Accepted on 12/02/2019
Available Online on 02/05/2019
Keywords
Case report
�
Endodontic management of developmental anomalies: conservation of invaginated tissues in Type II dens invaginatus � case series
Abordagem endod�ntica de anomalias de desenvolvimento: conserva��o dos tecidos invaginados de dens invaginatus Tipo II � s�rie de casos
�
Mariana Domingos Piresa,*, Abayomi Omokeji Baruwaa, Jorge N.R. Martinsa,b, S�rgio Andr� Quaresmaa,c, Rui Pereira da Costaa,c, Ant�nio Ginjeiraa
a Department of Endodontics, Faculdade de Medicina Dent�ria, Universidade de Lisboa (University of Lisbon), Lisbon, Portugal
b Centro de Estudo de Medicina Dent�ria Baseada na Evid�ncia, Faculdade de Medicina Dent�ria, Universidade de Lisboa (University of Lisbon), Lisbon, Portugal
c Department of Endodontics, Universitat Internacional de Catalunya (University of Catalunya), Barcelona, Spain
�
�
http://doi.org/10.24873/j.rpemd.2019.03.442�
Abstract
Dens invaginatus is an uncommon occurrence in the permanent dentition. However, practitioners must be aware of this anatomical variation, as an early diagnosis may prevent the need for endodontic treatment. Clinically, root canal treatment of Oehler�s Type II dens invaginatus may present a complex challenge. This paper reports two cases of non-surgical endodontic treatment and one case of non-surgical endodontic retreatment of upper lateral incisors diagnosed with Oehler�s Type II dens invaginatus. All procedures were done maintaining the original anatomy of both the invagination and the root canal space to minimize dentin elimination. At follow-up appointments, resolution of apical pathosis was noted in all three cases, with no sign of structural strain. With the help of dedicated instruments, such as ultrasonic tips, and under magnification, the conservation of the invagination in Oehler�s Type II dens invaginatus is a valid and successful treatment option.
Keywords: Case reports, Dens in dente, Dens invaginatus, Endodontics, Endodontic treatment
�
Resumo
Apesar do dens invaginatus ser uma ocorr�ncia pouco comum na denti��o permanente, o cl�nico deve considerar esta varia��o anat�mica, uma vez que o diagn�stico atempado pode evitar a necessidade de tratamento endod�ntico. Clinicamente, o tratamento endod�ntico do dens invaginatus tipo II de Oehlers pode constituir um desafio complexo. Neste artigo apresentamos dois casos de tratamento endod�ntico e um de retratamento endod�ntico de incisivos laterais superiores diagnosticados com dens invaginatus tipo II de Oehlers. Todos os tratamentos foram realizados com a manuten��o da anatomia, tanto dos tecidos invaginados como do sistema canalar, para minimizar a perda de estrutura dentin�ria s�. Nas consultas de controlo, foi observada resolu��o da patologia periapical nos tr�s casos, sem comprometimento da estrutura dent�ria remanescente. Com a ajuda de material espec�fico, como pontas ultrass�nicas, e sob amplia��o, a conserva��o do tecido invaginado no tratamento de dens invaginatus tipo II de Oehlers constitui uma op��o de tratamento v�lida e com resultados previs�veis.
Palavras-chave: Caso cl�nico, Dens in dente, Dens invaginatus, Endodontia, Tratamento endod�ntico
�
Introduction
Dens invaginatus consists of an infolding of a tooth�s outer portion (enamel) into the inner portion (dentine) during the soft tissue stage of development, with the formation of a pocket-like space.1, 2 Several classification systems have been proposed for this condition, and the most commonly accepted was published by Oehlers3 in 1957. This system differentiates three types according to how far the invagination extends radiographically into the root: in Type I, the invagination is limited to the crown; in Type II, it invades part of the root and ends as a blind sac; and in Type III, it invades the entire root ending with a communication with the lateral periodontal tissues (Type IIIa) or periapical tissues (Type IIIb).1, 2, 4, 5
The prevalence of dens invaginatus varies depending on the invagination type. Type I is the most common, and it may reach a prevalence of 11.3%, while Types II and III are uncommon and may reach 0.7% and 0.8% of cases, respectively.6 Nevertheless, some studies report much lower ratios.7, 8 The most affected teeth are the maxillary lateral incisors, and bilateral occurrence is not uncommon.4, 6, 9
The affected tooth may show no clinical symptoms, and, in most cases, the dens invaginatus is detected by chance on a radiograph.8, 10 The invagination allows the entry of irritant agents, such as microorganisms, into the invaginated lumen.
This inner space presents an atypical morphological tissue arrangement and might be extremely close to the pulp space, or even communicate with it. This situation creates a predisposition for the development of dental caries, or even pulp necrosis, which often occurs rather early, within a few years of eruption, and sometimes even before root end closure, and may eventually lead to the development of periapical pathosis in an intact and healthy-looking tooth.4, 5, 8, 11
Periapical pathosis is more prone to occur in dens invaginatus Types II and III.6 7, According to Gunduz et al.,7 at the time of treatment referral, 8.1% and 87.5% of the patients with dens invaginatus Types II and III, respectively, had periapical pathosis. Kirzioglu & Ceyhan6 reported similar findings. An invaginated tooth may pose technical difficulties to its clinical management.8 Clinically, dens invaginatus Types II and III with pulp necrosis often represent the most challenging cases, since the pulp pathosis usually requires treatment of both the invagination and the main root canal system, and, in extreme cases, the total elimination of the invaginated tissues, which might lead to structural fragility.12
The objective of this article is to show three cases of endodontic treatment of Type II dens invaginatus. In all three cases, the invagination was preserved separately from the pulp canal space in an effort to spare healthy dentine and, thus, keep the original structural strength.
CASE REPORTS
General clinical proceduresThree patients were referred for endodontic evaluation of a maxillary lateral incisor. In all cases, the medical and dental history was reviewed and considered non-contributory, and intra-oral and radiographic examinations were performed.
Diagnosis of pulpal and periapical pathosis was made based on pulpal tests and periapical radiographs. In all teeth, a deep radiopaque enamel infolding could be noted surrounding a radiolucent lumen ending inside the root canal space. These features allowed a radiographic diagnosis of Oehler�s Type II dens invaginatus in all teeth, which were also associated with apical periodontitis. Root canal therapy was recommended, accepted by all the patients, who filled and signed a general informed consent, and performed under a dental operating microscope. In all cases, an effort was made to preserve tooth structure by managing the invagination independently, without its incorporation into the adjacent pulp space. After proper local anesthesia and rubber dam placement, access was obtained, using round burs (Komet Medical, Lemgo, Germany; R&S, France), Start X ultrasonic tips (Dentsply Maillefer, Switzerland) or both, and a full debridement was performed under copious irrigation with 5.25% of sodium hypochlorite. Working length was performed by using electronic apex locators (Root ZX II, Morita, USA). In all cases, the final irrigation procedure also included irrigation for one minute with 10% citric acid or 17% EDTA prior to a final sodium hypochlorite rinse under sonic or manual dynamic agitation.
All teeth were filled with a resin-based sealer and warm gutta-percha, although, in one case, an apical barrier of MTA was also required. A posterior follow-up appointment showed an improvement of the clinical condition in all cases, without any sign of structural failure.
Case report #1
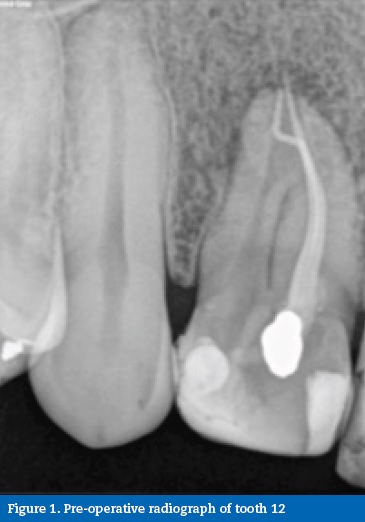
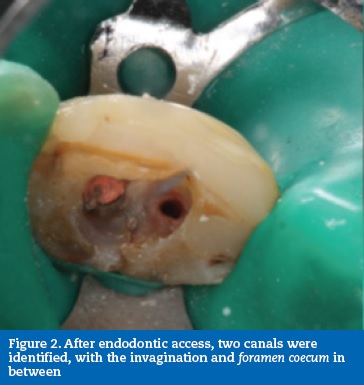
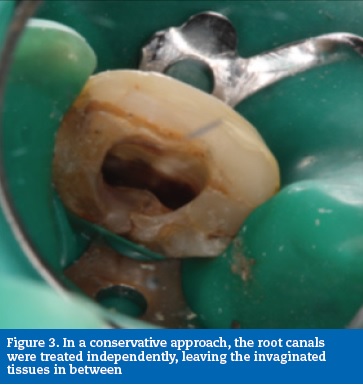
After clinical observation, a 34-year-old Caucasian male was diagnosed with asymptomatic apical periodontitis on tooth 12 after previous endodontic treatment (Figure 1). After accessing the pulp chamber, two canal orifices were evident with the invagination and foramen coecum in between (Figure 2). In an attempt to avoid excessive root structure damage, both root canals were treated independently, leaving the invaginated tissues in between to be included in the final root canal filling (Figure 3). Root canal instrumentation was performed with ProTaper nickel-titanium rotary instruments (ProTaper Universal, Dentsply Maillefer, Switzerland).
Due to an excessively large apical size, an apical barrier of 6 mm in thickness was created with MTA (ProRoot MTA, Dentsply Tulsa Dental, USA) in the first appointment (Figure 4).
�
�
�
�

�
In a second visit, the rest of the canal was back-filled with gutta-percha and sealer (Top Seal, Dentsply Maillefer, Switzerland) using the continuous wave of condensation technique (Figure 5). A 2-year follow-up revealed satisfactory healing of the inflammatory process associated with the tooth (Figure 6).
�

�

�
Case report #2
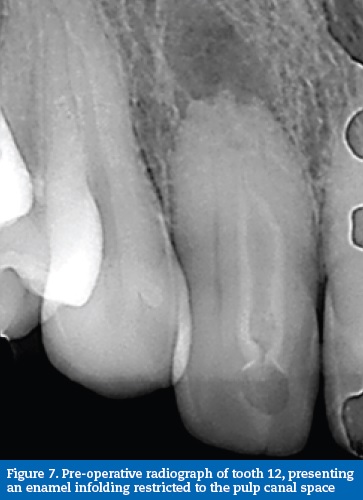
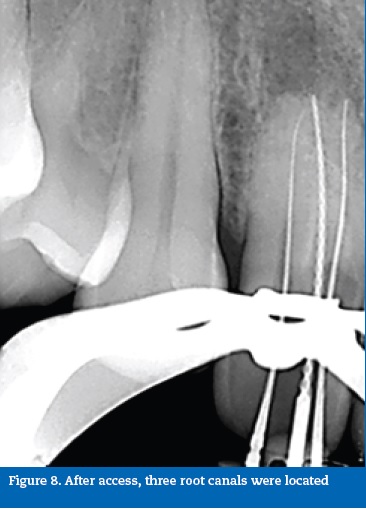
A 31-year-old Caucasian female patient was referred by a general practitioner after diagnosis of necrotic pulp and asymptomatic apical periodontitis on tooth 12. Radiographic exams revealed the presence of periapical pathology. An atypical pulpal anatomy could be observed with an enamel-lined invagination running parallel to the pulp system in the entire root but ending inside the root canal space. (Figure 7).
�
�
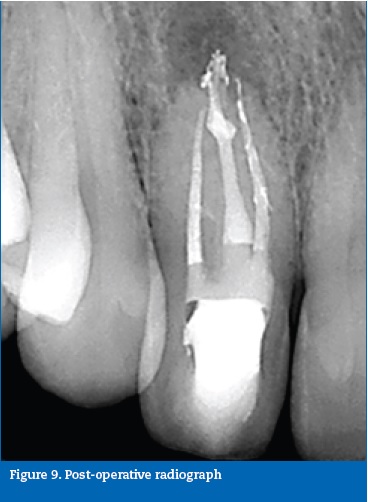
Endodontic therapy was performed under magnification, over three visits. After endodontic access, three canals were located and identified with START-X 3 ultrasonic tips and Endo Sonore files (Dentsply Maillefer, Switzerland). The central canal was the lumen of the invaginated tissues, while both peripheral root canals belonged to the pulp space, which was divided and compressed outwards by the invagination (Figure 8). The three canals were instrumented with ProTaper nickel-titanium rotary instruments (ProTaper Universal, Dentsply Maillefer, Switzerland). The invagination was managed as an independent root canal. Root canal obturation was performed with gutta-percha and sealer (Top Seal, Dentsply Maillefer, Switzerland) using the continuous wave of condensation technique (Figure 9). A 12-month follow-up radiograph showed healing of the periapical tissues (Figure 10).
�
�
�

�
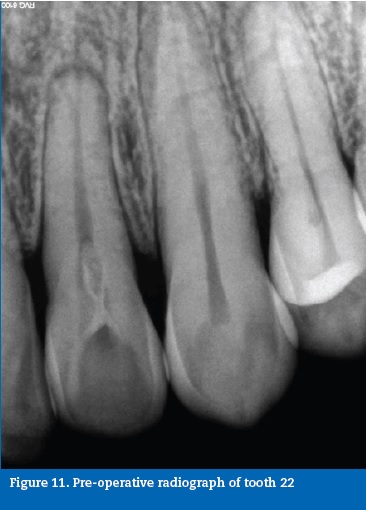
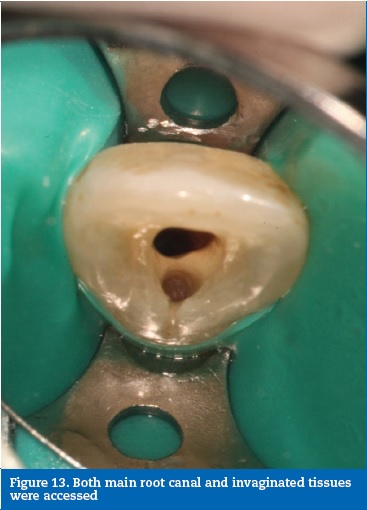
Case report #3A 41-year-old Caucasian male was diagnosed with necrotic pulp and symptomatic apical periodontitis on tooth 22. A clinical, radiographic analysis revealed an Oehler�s Type II dens invaginatus (Figure 11). The tooth was intact, and it was assumed that the necrosis was due to the communication between the foramen coecum, in the palatal surface, and the dental pulp, through the invagination (Figure 12). A routine access to the main root canal system was prepared and the access to the interior of the invaginated tissues was prepared with ultrasonic tips (ProUltra, Dentsply Maillefer, Switzerland) (Figure 13). The root canal system and invagination were instrumented and disinfected independently, not removing the entire dens invaginatus to preserve structure. ProTaper nickel-titanium rotary instruments (ProTaper Universal, Dentsply Maillefer, Switzerland) were used. At the second visit, the root canal and invagination were filled with gutta-percha and sealer (AH Plus, Dentsply, USA) using the continuous wave of condensation technique (Figures 14, 15 and 16).
�
�

�
�

�

�

�
A communication was noted between the canal and the invagination in the final radiograph (Figure 17). A 7-month follow-up radiograph showed healing of the periapical tissues (Figure 18).
�

�

�
Discussion
Early diagnosis of dens invaginatus is important to help prevent the need for endodontic treatment and to plan for it correctly when necessary. This anomaly is more commonly detected by chance in periapical radiographs, but clinicians should be aware of its prevalence and take it into consideration especially when assessing upper lateral incisors.8, 10 Advanced radiographic techniques with cone-beam computed tomography (CBCT) imaging may also be useful.12 However, the decision to use CBCT scanning should depend on whether the benefits outweigh the risk of the relatively higher radiation dose.9 Treatment options for dens invaginatus range from preventive measures such as sealing minimal invaginations in cases of vital pulp and absence of clinical symptoms and radiographic signs, to extraction when the invagination is severe and the tooth has a poor prognosis.13, 14 Clinically, Oehler�s Type II invaginations are more challenging and difficult to deal with due to the larger extension of the invagination and the complexity of the internal anatomy, which may hamper the thorough disinfection of the canal space.15 Moreover, early pulp necrosis may lead to arrest of root development, and, consequently, an open apex, further complicating the management of such teeth.5, 15
However, the technological advances in Endodontics, such as the operating microscope, ultrasonic tips and bioceramic cements, make conventional endodontic treatment of Type II dens invaginatus predictable.
When both the root canal and the invagination are infected, the root canal treatment of a dens invaginatus Type II anatomy may involve the inclusion of the invagination into the root canal space or maintaining the invagination separately. Two studies have recommended the elimination of the invagination and its infected dentin, and the consequent creation of a unique and larger root canal space, to simplify the root canal disinfection and obturation.14, 16 However, this may lead to unnecessary elimination of healthy dentine besides resulting in thinner root walls, which may increase the tendency for root fracture. Other techniques, such as regenerative endodontics, endodontic microsurgery or both have also been reported as successful options to treat Type II dens invaginatus.17 - 19 In these morphologies, the apex is also unusually large, due to incomplete or atypical embryological development, thus rendering impossible to guarantee adequate apical seal with conventional thermoplastic obturation techniques, and apexification with an MTA apical barrier might be recommended. The results of both in vitro and in vivo studies show that MTA is not only biocompatible but also bioactive, and exerts antibacterial properties while assuring a good seal.20 - 24 In an attempt to overcome the known drawbacks of MTA (long setting time, high cost, and potential for discoloration) other bioceramic cements, such as Biodentine (Septodont, Saint-Maur-des-Foss�s, France), have been employed for apical plugs with promising results.25, 26
It is important that the clinician acknowledges the complexity of this kind of teeth and its morphology and prepares himself with certain armamentarium. With the use of modern endodontic techniques such as specific ultrasonic tips and microscope magnification, the clinician is able to perform a conventional endodontic treatment with predictable outcomes, while trying to preserve the maximum structure possible.27
The three case reports described in this study are demonstrative of different dens invaginatus morphologies. All cases were associated with both root canal and invagination infection.
The pulpal and periapical diagnoses were based on pulpal tests and intraoral digital periapical radiographs. All cases were endodontically treated while preserving the invaginated tissues separated from the main canal space. This procedure allowed the reduction of healthy dentin removal and avoiding the creation of an extremely large empty root canal space, which would reduce the root�s global strength. Although a proper endodontic treatment follow-up is recommended after one year, or even earlier, these clinical cases presented resolution of symptoms and clinical improvements in the periapical lesions in all three cases, with no signs of structural fatigue.28 Even though a longer follow-up would be recommended, the clinical option to perform endodontic treatment without incorporating the invaginated tissues into the canal space showed a favorable outcome.
�
References
1. Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J. 2008;41:1123-36.
2. Sathorn C, Parashos P. Contemporary treatment of class II dens invaginatus. Int Endod J. 2007;40:308-16.
3. Oehlers FA. Dens invaginatus (dilated composite odontoma). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med and Oral Pathol. 1957;10:1204-18.
4. H�lsmann M. Dens invaginatus: Aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30:79‐90.
5. Er K, Kustarcı A, �zan U, Ta� sdemir T. Nonsurgical Endodontic Treatment of Dens Invaginatus in a Mandibular Premolar with Large Periradicular Lesion: A Case Report. J Endod. 2007;33:322-4.
6. Kirzioglu Z, Ceyhan D. The prevalence of anterior teeth with dens invaginatus in the western Mediterranean region of Turkey. Int Endod J. 2009;42:727‐34.
7. G�nd�z K, Peruze C, Canger EM Zengin Z, S�mer P. A retrospective study of the prevalence and characteristics of dens invaginatus in a sample of the Turkish population. Med Oral Patol Oral Cir Bucal. 2013;18:e27-32.
8. Hamasha AA, Al-Omari QD. Prevalence of dens invaginatus in Jordanian adults. Int Endod J. 2004;37:307-10.
9. Capar ID, Ertas H, Arslan H, Ertas ET. A Retrospective Comparative Study of Cone-beam Computed Tomography versus Rendered Panoramic Images in Identifying the Presence, Types, and Characteristics of Dens Invaginatus in a Turkish Population. J Endod. 2015;41:473-8.
10. Jaramillo A, Fern�ndez R, Villa P. Endodontic treatment of dens invaginatus: A 5-year follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e15-21.
11. Ozbas H, Subay R, Orduli M. Surgical retreatment of an invaginated maxillary central incisor following overfilled endodontic treatment: a case report. Eur J Dent. 2010;4:324-8.
12. Kristoffersen �, Nag OH, Fristad I. Dens invaginatus and treatment options based on a classification system: report of a type II invagination. Int Endod J. 2008;41,702-9.
13. Zengin A, Sumer A, Celenk P. Double Dens Invaginatus: report of three cases. Eur J Dent. 2009;3:67-70.
14. Baumgart M, Hanni S, Suter B, Schaffner M, Lussi A. Dent invagin�e (dens invaginatus) revue de litt�raturerecommandations diagnostiques et th�rapeutiques. Rev Mens Suisse Odontostomatol. 2009;119:706-14.
15. Pai SF, Yang SF, Lin LM. Nonsurgical endodontic treatment of dens invaginatus with large periradicular lesion: a case report. J Endod. 2004;30:597-600.
16. Silberman A, Cohenca N, Simon JH. Anatomical redesign for the treatment of dens invaginatus type III with open apexes: a literature review and case presentation. J Am Dent Asoc. 2006;137:180-5.
17. Timmerman A, Parashos P. Delayed root development by displaced mineral trioxide aggregate after regenerative endodontics: a case report. J Endod. 2017;43:252-6.
18. Srivastava R, Verma P, Tripathi V, Tripathi P, Singh A. Management of Oehlers Type II dens in dente with open apex and alveolar bone defect. J Clin Diagn Res. 2016;11:zj05-6.
19. Pinto N, Hamish A, Cabrera C, Andrade C, Druttman T, Brizuela C. An innovative regenerative endodontic procedure using leukocyte and platelet-rich fibrin associated with apical surgery: case report. J Endod. 2017;43:1828-34.
20. Camilleri J, Montesin FE, Papaioannou S, McDonald F, Pitt Ford TR (2004) Biocompatibility of two commercial forms of mineral trioxide aggregate. Int J Endod. 2004;37:699-704.
21. Kim DH, Jang JH, Lee BN, Chang HS, Hwang IN, Oh WM, Hwang YC. Anti-inflammatory and Mineralization Effects of ProRoot MTA and Endocem MTA in Studies of Human and Rat Dental Pulps In Vitro and In Vivo. J Endod. 2018;44:1534-41.
22. Parirokh M, Torabinejad M. Mineral Trioxide Aggregate: A Comprehensive Literature Review � Part I: Chemical, Physical, and Antibacterial Properties. J Endod. 2010;36;16-27.
23. Ng FK, Messer LB. Mineral trioxide aggregate as a pulpotomy medicament: An evidence-based assessment. Eur Arch Paediatr Dent. 2008;9:58-73.
24. Rajasekharan S, Martens LC, Vandenbulcke J, Jacquet W, Bottenberg P, Cauwels RGEC. Efficacy of three different pulpotomy agents in primary molars: a randomized control trial. Int Endodo J. 2016;50;215-28.
25. Parirokh M, Torabinejad M. Mineral Trioxide Aggregate: A Comprehensive Literature Review�Part III: Clinical Applications, Drawbacks, and Mechanism of Action. J Endod. 2010;36:400-13.
26. Haapasalo M, Parhar M, Huang X, Wei X, Lin J, Shen Y. Clinical use of bioceramic materials. Endod Topics. 2015;32:97-117.
27. Bishop K, Alani A. Dens invaginatus. Part 2: clinical, radiographic features and management options. Int Endod J. 2008;41:1137-54.
28. �rstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29:150-5
�
Mariana Domingos Pires
E-mail address: mariana.dpires@gmail.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 1 October 2018
Accepted 12 February 2019
Available online 2 April 2019
