
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2017 | 58 (3) | 188-191
Case report
Unusual presentation of a psoriasiform mucositis in the oral cavity: case report
Apresentação incomum de uma mucosite psoriasiforme na cavidade oral: caso clínico
a Faculdade de Medicina de Juiz de Fora, Universidade Presidente Antônio Carlos, Juiz de Fora, Minas Gerais, Brasil
b Oral and Maxillofacial Surgery, Associação Brasileira de Odontologia, Juiz de Fora, Minas Gerais, Brasil
Pietro Mainenti - pietromainenti@terra.com.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 3
Case report
Pages - 188-191
Go to Volume
Article History
Received on 17/04/2017
Accepted on 11/10/2017
Available Online on 10/11/2017
Keywords
Case report
�
Unusual presentation of a psoriasiform mucositis in the oral cavity: case report
Apresenta��o incomum de uma mucosite psoriasiforme na cavidade oral: caso cl�nico
�
Daniela Pereira Bortolina, Gustavo Neumann Barrosa, Isaac Nilton Fernandes Oliveiraa, Rodrigo Falci Santosb, Pietro Mainentia,*
a Faculdade de Medicina de Juiz de Fora, Universidade Presidente Ant�nio Carlos, Juiz de Fora, Minas Gerais, Brasil.
b Oral and Maxillofacial Surgery, Associa��o Brasileira de Odontologia, Juiz de Fora, Minas Gerais, Brasil.
�
�
http://doi.org/10.24873/j.rpemd.2017.11.027
�
Abstract
Psoriasis is a chronic inflammatory disease that may affect the skin and sometimes the joints. Owing to some similarities, the psoriasiform mucositis can be misinterpreted as a psoriatic lesion or vice-versa. However, some authors do not accept the occurrence of an oral psoriatic manifestation without associated skin lesions. The present case report describes a strictly oral manifestation of psoriasiform mucositis. The patient was a 24-year-old woman that complained of a reddish lesion in her palate. As the clinical presentation did not favor a provisional diagnosis, the final determination of the lesion occurred only after the clinical exam and the hematological and histopathological findings. In the authors' opinion, the psoriasiform mucositis depicted in the present report revealed an unusual manifestation of an erythematous bilateral lesion. The differential diagnosis of psoriatic lesion and psoriasiform mucositis may be challenging and require a careful study of each case. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(3):188-191)
Keywords: Oral mucositis, Psoriasiform mucositis, Psoriasis
�
Resumo
A psor�ase � uma doen�a inflamat�ria cr�nica que afeta a pele e pode ter reflexo nas articula��es. Devido a algumas semelhan�as, a mucosite psoriasiforme pode ser mal interpretada como uma les�o psori�tica ou vice-versa. No entanto, alguns autores podem n�o aceitar a ocorr�ncia de uma manifesta��o psori�tica oral sem les�es cut�neas. O presente relato de caso cl�nico descreve uma manifesta��o estritamente oral de uma mucosite psoriasiforme. A paciente era uma mulher de 24 anos que se queixava de uma les�o avermelhada em seu palato. Como a apresenta��o cl�nica n�o favoreceu um diagn�stico imediato, a determina��o final da les�o ocorreu somente ap�s a soma do exame cl�nico e dos achados hematol�gicos e histopatol�gicos. Na opini�o dos autores, a mucosite psoriasiforme, descrita no presente relato, revelou uma manifesta��o incomum de uma les�o eritematosa bilateral. O diagn�stico da les�o psori�tica e da mucosite psoriasiforme pode ser desafiador, exigindo um estudo cuidadoso de cada caso. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(3):189-191)
Palavras-chave: Mucosite oral, Mucosite psoriasiforme, Psor�ase
�
Introduction
Psoriasis is a chronic immune-mediated inflammatory disease associated with a genetic background, that affects the skin and sometimes joints. A clinical polymorphism is expected, tending to be symmetrically distributed on extensor surfaces of the extremities. Its etiology is still incompletely understood. It affects both genders equally and about 1% to 3% of the global population.1-3
Oral psoriasis is unusual, and its manifestation without other anatomic involvement has been questioned.3-6 Although some authors accept the existence of oral lesions as a manifestation of psoriasis based on their similarity with the skin lesions, others claim that the oral and skin lesions need to be found simultaneously in order to diagnose a psoriatic occurrence. 4 ,5 ,7 ,8 Intraoral lesions are rarely reported, and the first-ever clinical findings reported had no microscopic confirmation. As a result, the number of case descriptions and the incidence of intraoral psoriasis cannot be accurately determined based on the literature. 2 ,4 ,6 ,7
Psoriasiform mucositis presents a variable pattern and may be asymptomatic, revealing an erythematous aspect.,5-,7
The diagnosis of psoriasiform mucositis is strongly supported by microscopic findings, and biopsy is an essential tool.,4-,6 Its microscopy shows hyperkeratosis, club-shaped elongation of the rete ridges, thinning of the suprapapillary epithelium, and a chronic inflammatory infiltrate consisting, predominantly, of lymphocytes or neutrophils, depending on the stage of the lesion.,6 However, there is no specific microscopic presentation for oral psoriasis, and such features could be shared by other histologically similar diseases. 2 ,4 ,6 ,8
This report describes a case of a strictly oral manifestation of a psoriasiform lesion and addresses the diagnosis and treatment regarding its unusual presentation.
Case Report
A 24-year-old woman attended an appointment with an oral and maxillofacial surgeon, in March 2015. At the consultation, the chief complaint was: �I noticed a red spot on my palate�. The patient stated that the lesion had been there for three months.
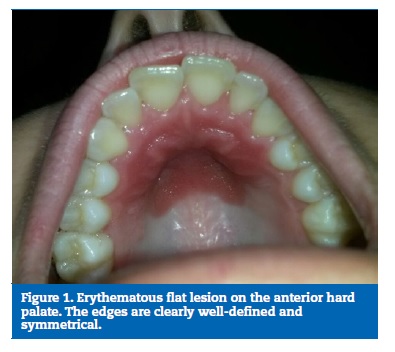
During anamnesis, the patient denied using prescription drugs and having hypersensitivity to drugs or systemic alterations. Clinical examination revealed a flat erythematous lesion, with well-defined edges and bilateral symmetry, affecting the anterior mucosa of the hard palate (Figure 1). There were no other lesions on the skin or other mucosal surfaces.
�
�
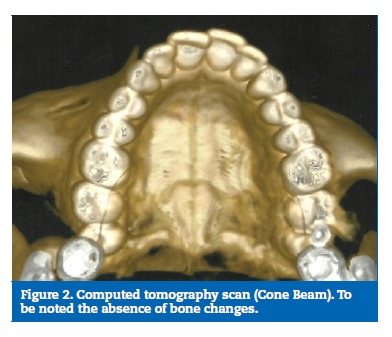
A computed tomography scan (CT scan) was requested to evaluate a potential bone invasion. The exam was performed to rule out the possibility of neoplasia (lethal midline granuloma) or vasculitis (Wegener�s granulomatosis). The CT scan showed no bone lesion (Figure 2).
�
�
An incisional biopsy was performed to clarify the diagnosis.
An ellipsoid specimen (measuring 1.1 x 0.4 cm) of the suspicious area and a margin was removed. The tissue was fixed in 10% formalin and sent for histopathological analysis.
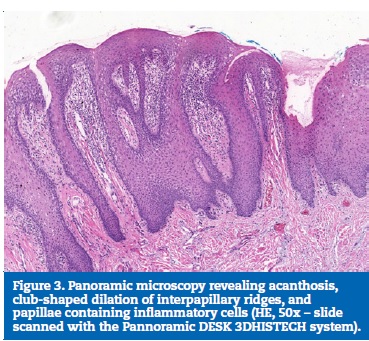
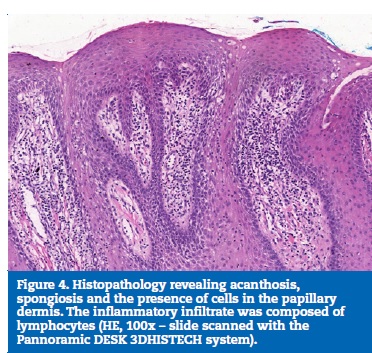
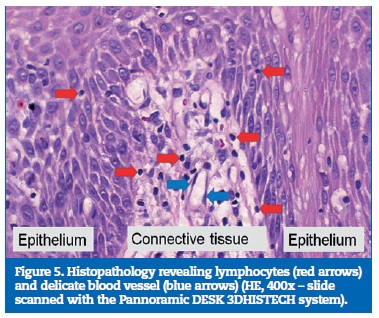
The histopathological analysis of the specimen revealed a stratified squamous epithelium lining the sample. Acanthosis, spongiosis and club-shaped dilatation of the interpapillary ridges were observed. The papillae showed an inflammatory infiltrate composed of lymphocytes. The microscopic features favored a psoriasis-like lesion (Figures 3, 4 and 5).
�
�
�
�
Complementary exams were requested in May 2015, and an analysis of biomarkers of inflammation and antinuclear factor (ANF) was performed in order to track an active rheumatic disease. The results were as follows: erythrocyte sedimentation rate = 43 mm/h (reference range: 0-15 mm/h), quantitative C-reactive protein = 1.3 mg/dl (reference range: 0-6 mg/dl) and antinuclear factor = 1:80 (default: fine speckled pattern without staining in the cytoplasm, the mitotic apparatus and the chromosomal metaphase plate).
Treatment with a topical ointment consisting of betamethasone valerate (0.05%), gentamicin sulfate (0.1%), tolnaftate (1%) and clioquinol (1%), t.i.d. for 30 days, was prescribed. The follow-up, after the treatment, showed the remission of the lesion (Figure 6).
�

�
Discussion and Conclusions
The etiology of psoriasis remains unknown, even though it is clear that it has a genetic component.2 The disease affects both genders equally.2 Its lesions appear before the second decade of life in 50% of the cases and are more frequent in Caucasians.2
As a provisional diagnosis, this case could be diagnosed as a psoriatic lesion. However, the clinical and test findings pointed in another direction.
Some criteria have been proposed for the diagnosis of oral psoriasis, including a) a concurrent manifestation of oral and skin lesions, b) a family history of skin psoriasis and c) a clinicopathological manifestation consistent with the disease. 2 ,4 ,7 ,8
Suspected lesions may be considered psoriasiform mucositis in the absence of the aforementioned diagnostic criteria.,4 In the present case report, the differential diagnosis between oral psoriasis and psoriasiform mucositis took into account the characteristics proposed by the pertinent literature. Therefore, in the absence of psoriatic oral presentations and skin lesions, the diagnose was psoriasiform mucositis.
Psoriasiform mucositis� lesions show variable manifestations and may be white or erythematous, with serpiginous or annular edges. 4 ,6 ,8
,9 The oral lesions may affect any part of the oral mucosa, but the palate and gingiva are unusual sites. 4 ,6 -8This report presents a flat erythematous lesion on the mucosa of the hard palate. According to the literature, psoriasiform lesions are uncommon in the palate. This case presents itself as very unusual due to the symmetrical and erythematous lesion, thus not favoring a prompt clinical diagnosis. In order to rule out some diseases, such as vasculitis (Wegener�s granulomatosis) and neoplasia (lethal midline granuloma), a conebeam tomographic exam was performed.
The differential diagnosis between psoriasiform mucositis and other diseases, such as psoriasis, Reiter�s syndrome, benign migratory glossitis and migratory erythema, may be very challenging since they can share similar clinical or histological findings. 3 ,4 ,6 ,8
However, the examiner can rule out the non-psoriasiform lesions by assessing the clinical presentation in association with the microscopic findings. 3 ,4 ,6 ,8
On microscopic examination, psoriasiform mucositis presents some features such as acanthosis and parakeratosis. 4 ,6 ,8 Moreover, the epithelium may show exocytosis, and the connective tissue may exhibit leukocyte infiltration and vascular congestion in the papillary region.2 The intraepithelial microabscess, known as Munro abscess, is also typically seen in psoriasis.2 In this case, a biopsy specimen was obtained for the microscopic analysis of the lesion. Munro abscesses were not present.However, the histopathology disclosed a psoriasis-like lesion by revealing typical features of acanthosis, club-shaped dilation of the interpapillary ridges, swollen connective tissue papillae and an inflammatory infiltrate composed of lymphocytes.
To establish a careful evaluation of the case, some blood tests were ordered in an attempt to rule out psoriatic arthropathy. The antinuclear factor found indicated a very little chance of an autoimmune rheumatic disease. According to Dellavance et al.,10 the nuclear fine speckled pattern, as found in the present case, is predominantly associated with a lack of autoimmune disease. In the absence of clinical arthropathy, and since the histopathology did not support psoriasis, psoriatic arthritis was excluded. Also, the positive laboratory findings of erythrocyte sedimentation rate and C-reactive protein were not sufficient to support a diagnosis of psoriasis.
There is no standard treatment for psoriasis-like lesions. Both steroids and retinoids help to control the disease.4 Richardson et al.6and Tarakji et al.11 described the use of corticosteroids successfully, while Reis et al.9 used retinoids with success. Richardson et al.6 reported that asymptomatic cases do not require medication. In this report, the patient was asymptomatic in every consultation. However, the patient�s complaint resulted in an investigation and treatment. The patient was treated with topical ointment consisting of betamethasone valerate (0.05%), gentamicin sulfate (0.1%), tolnaftate (1%) and clioquinol (1%), for 30 days. The result was a remission. After the pharmacological treatment, the patient no longer showed signs of the disease.
The clinical case described did not favor a diagnosis after the initial clinical examination. A biopsy was performed, and the microscopy revealed psoriasiform mucositis. Since there is some controversy between psoriasiform mucositis and psoriasis, a diligent evaluation of the case was conducted. Clinical, hematological and histopathological findings were then correlated with the final diagnosis of psoriasiform mucositis. In the authors� opinion, the present case revealed an unusual manifestation of an erythematous bilateral lesion on the palate.
�
References
1. Brasileiro Filho G. Bogliolo: Patologia. 8th ed. Rio de Janeiro: Guanabara Koogan; 2011.
2. Migliari DA, Penha SS, Marques MM, Matthews RW. Considerations on the diagnosis of oral psoriasis: a case report. Med Oral. 2004;9:300-3.
3. Sociedade Brasileira de Dermatologia. Consenso Brasileiro de Psor�ase 2012: guias de avalia��o e tratamento. 2nd ed. Rio de Janeiro; 2012.
4. Fatahzadeh M, Schwartz RA. Oral Psoriasis: An Overlooked Enigma. Dermatology 2016;232:319-25.
5. Ganzetti G, Campanati A, Santarelli A, Pozzi V, Molinelli E, Minnetti I, et al. Involvement of the oral cavity in psoriasis: results of a clinical study. Br J Dermatol. 2015;172:282-5.
6. Richardson LJ, Kratochvil FJ, Zieper MB. Unusual palatal presentation of oral psoriasis. J Can Dent Assoc. 2000;66:80-2.
7. Yesudian PD, Chalmers RJ, Warren RB, Griffiths CE. In search of oral psoriasis. Arch Dermatol Res. 2012;304:1-5.
8. Khan S, Zaheer S, Gupta ND. Oral psoriasis: A diagnostic dilemma. Eur J Gen Dent 2013;2:67-71.
9. Reis V, Artico G, Seo J, Bruno I, Hirota SK, Lemos J�nior C, et al. Psoriasiform mucositis on the gingival and palatal mucosae treated with retinoic-acid mouthwash. Int J Dermatol. 2013;52:113-5.
10. Dellavance A, Leser PG, Andrade LEC. Import�ncia do padr�o de fluoresc�ncia na interpreta��o do teste do FAN: o caso do padr�o pontilhado fino denso. Rev Assoc Med Bras 2007;53:439-45.
11. Tarakji B, Umair A, Babaker Z, Eghaiby SNA, Gazal G, Sarraj F. Relation Between Psoriasis and Geographic Tongue. J Clin Diagn Res 2014;8:6-7.
�
Pietro Mainenti
E-mail address: pietromainenti@terra.com.br
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflicts of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 17 April 2017
Accepted 11 October 2017
Available online 16 November 2017
