
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2017 | 58 (3) | 133-138
Review
Therapy for bisphosphonate-related osteonecrosis of the jaw: a systematic review
Tratamento da Osteonecrose dos maxilares induzidas por bifosfonatos: Revisão Sistemática
a School of Medical and Health Sciences of Juiz de Fora, SUPREMA/JF- MG, Brasil
b Dentistry program of SUPREMA/JF and Hospital e Maternidade Therezinha de Jesus (HMTJ), Brasil
c Implantology program of SUPREMA/JF and Hospital e Maternidade Therezinha de Jesus HMTJ), Brasil
d Department of Prosthodontics, School of Dental Medicine, University of Zagreb, Croatia
e Faculty of Dentistry, Dalhousie University Halifax Nova Scotia, Canada
f Faculdade de Medicina Dentária da Universidade do Porto (FMDUP), Portugal
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 3
Review
Pages - 133-138
Go to Volume
Article History
Received on 08/12/2016
Accepted on 07/08/2017
Available Online on 04/10/2017
Keywords
Review
�
Therapy for bisphosphonate-related osteonecrosis of the jaw: a systematic review.
Tratamento da Osteonecrose dos maxilares induzidas por bifosfonatos: Revis�o Sistem�tica.
�
Felipe Lara Francischettia,*, Ant�nio M�rcio Lima Ferraz J�niorb, Rodrigo Guerra de Oliveirab,c, Tomislav Badeld, Archie Morrisone, Raquel Zita Gomesf
a School of Medical and Health Sciences of Juiz de Fora, SUPREMA/JF� MG, Brasil
b Dentistry program of SUPREMA/JF and Hospital e Maternidade Therezinha de Jesus (HMTJ), Brasil
c Implantology program of SUPREMA/JF and Hospital e Maternidade Therezinha de Jesus HMTJ), Brasil
d Department of Prosthodontics, School of Dental Medicine, University of Zagreb, Croatia
e Faculty of Dentistry, Dalhousie University Halifax Nova Scotia, Canada
f Faculdade de Medicina Dent�ria da Universidade do Porto (FMDUP), Portugal
�
�
http://doi.org/10.24873/j.rpemd.2017.10.022
�
ABSTRACT
Bisphosphonates are usually prescribed for treating metabolic and neoplastic bone disorders. Intravenous bisphosphonate formulations containing nitrogen are the ones most often associated with osteonecrosis of the jaw. The available therapies range from conservative procedures to invasive procedures.
The literature was systematically reviewed to determine the therapies available and their efficacy.
Related studies published originally in any language from January 2003 to April 2017 and indexed in the MEDLINE (National Library of Medicine) and Cochrane databases were analyzed. The following phrases were searched: �Bisphosphonate-Associated Osteonecrosis of the Jaw� OR �Bisphosphonate Osteonecroses� OR �Bisphosphonate Osteonecrosis� OR �Bisphosphonate-Induced Osteonecrosis of the Jaw� OR �Bisphosphonate-Related Osteonecrosis of the Jaw� AND �treatment� OR �therapy� OR �therapeutics� OR �treatment outcome.� The inclusion criteria were randomized controlled clinical trials, pertinent retrospective studies, systematic reviews, and meta-analyses. The levels of evidence of the studies were assessed independently by two referees, experts in the area.
This review confirms that the therapeutic approaches are based only on expert recommendations and opinions. Hence, preventive guidelines are mandatory because there is no gold standard in the therapy of bisphosphonate-related osteonecrosis of the jaw. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(3):133-138)
Keywords: Bisphosphonates, Bisphosphonates Related, Osteonecrosis of the Jaw (BRONJ), Bisphosphonates therapy, Cancer and osteoporosis treatment
�
RESUMO
Os bisfosfonatos sao normalmente prescritos no tratamento de dist�rbios �sseos metab�licos e neopl�sicos. A associa��o de nitrog�nio com bisfosfonatos intravenosos e a forma mais frequentemente associada a osteonecrose dos maxilares. As terapias dispon�veis variam desde tratamentos conservadores a procedimentos invasivos.
O objetivo desta revis�o foi determinar os tratamentos dispon�veis e a sua efic�cia. Foram analisados estudos publicados de Janeiro de 2003 a Abril de 2017 indexados na MEDLINE e Cochrane com as palavras-chave: Bisphosphonate-Associated Osteonecrosis of the Jaw� OU �Bisphosphonate Osteonecroses� OU �Bisphosphonate-Induced Osteonecrosis of the Jaw� OU �Bisphosphonate-Related Osteonecrosis of the Jaw� E �treatment� OU �therapy� OU �therapeutics� OU �treatment outcome�. Os crit�rios de inclus�o foram ensaios cl�nicos randomizados controlados, estudos retrospectivos pertinentes, an�lises sistem�ticas e meta-analises. Os niveis de evid�ncia dos estudos foram avaliados por dois �rbitros especializados. Esta revisao confirma que as abordagens terap�uticas sao baseadas em recomenda��es/opini�es de especialistas. Por isso a preven��o e obrigat�ria porque n�o ha uma terapia gold-standard na Osteonecrose dos maxilares induzida por bifosfanatos. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(3):133-138)
Palavras-chave: Bisfosfonatos, Osteonecrose dos maxilares induzida por bisfosfonatos, Terapia com bisfosfonatos, Tratamento do cancro e osteoporose
�
Introduction
Oral and intravenous bisphosphonates are first choice drugs for the treatment of osteoporosis, multiple myeloma, and metastatic bone disease. The affinity of bisphosphonates with bone tissue and their inhibitory effect on osteoclastic cells cause a strong antiresorptive action, reducing the risk of osteoporotic fractures and effectively controlling the deleterious effect of bone metastases. However, their use has been associated with osteonecrosis of the jaw (ONJ), which is a potentially severe side effect that affects the mandible in 70% of bisphosphonate cases1-7 In the literature regarding ONJ prevalence in patients treated with bisphosphonates, some studies found no bisphosphonate‑related osteonecrosis of the jaw (BRONJ), while others found BRONJ, with a prevalence of up to 7.8%, mainly in intravenous administrations.1-7Risk also increases significantly when the patient is subjected to dental procedures, especially tooth extraction and mainly when intravenous bisphosphonates are used.3 Other dental procedures may trigger BRONJ, such as periodontal surgeries and clinical or surgical endodontic interventions.1-3 Once BRONJ is developing, its management is a dilemma.8
To this day, no effective treatment was found and discontinuing bisphosphonates has not proven to be beneficial.3,8The temporary discontinuation of bisphosphonates does not seem to provide any short‑term advantage, while the long‑term discontinuation, if systemic conditions allow, may benefit the stabilization of ONJ sites and reduce clinical symptoms.1-7 Local and systemic antimicrobial drugs have been used independently or along with surgery, and sometimes associated with therapies that accelerate healing, such as laser therapy, hyperbaric oxygen, and platelet‑rich plasma.8-14
This systematic review aimed to assess the treatments available for BRONJ.
Participants: Patients with BRONJ
Intervention: Conservative or invasive procedures
Comparison: Between procedures available
Outcomes: Improvement or complete healing of BRONJ
Timeframe: Articles from 2003 to 2017
Methods
The review included the most pertinent studies published originally in any language from 2003 to 2017 and indexed in the MEDLINE (National Library of Medicine) and Cochrane databases.
In order to select the studies with the highest scientific evidence, we included randomized controlled clinical trials, the most relevant retrospectives studies and systematic reviews with or without meta‑analysis.
The search criteria included the following keywords of the medical subject heading (MeSH): �Bisphosphonate Associated Osteonecrosis of the Jaw� OR �Bisphosphonate Osteonecrosis� OR �Bisphosphonate Osteonecrosis� OR �Bisphosphonate‑Induced Osteonecrosis of the Jaw� OR �Bisphosphonate Related Osteonecrosis of the Jaw� AND �treatment� OR �therapy� OR �therapeutics� OR �treatment outcome�. The study designs were limited by the following keywords: �randomized controlled trial�, �retro-spective studies�, �systematic review�, �meta‑analysis�, �humans�, and �all languages�.
The inclusion and exclusion criteria were used freely and independently by two experienced referees from the area who selected studies based on the points raised for each issue (Table 1).
�
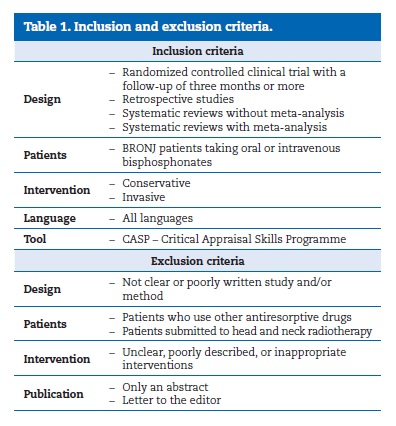
�
Results
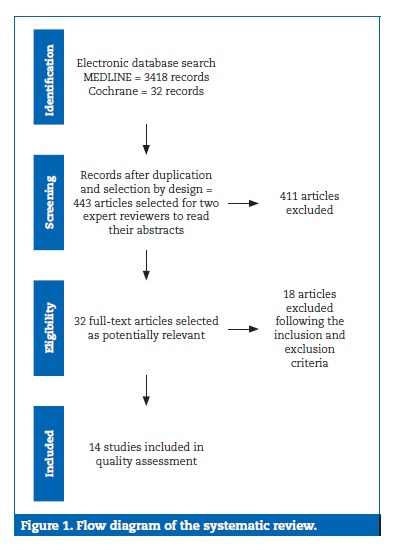
The search strategy was based on MeSH descriptors (Figure 1).
�
�
All searches were limited to human studies. The results of the database search for studies on BRONJ treatment, 3418 records in MEDLINE and 23 records in Cochrane, were combined, and the repeated articles excluded. After the selection based on study design (randomized controlled trial, retrospective study, systematic review, and meta‑analysis), 443 articles remained. Two experienced and independent referees chose 32 of the 443 studies after reading their abstracts. Then, after fully reading those 32 articles, 18 were excluded for being either unclear or poorly described.
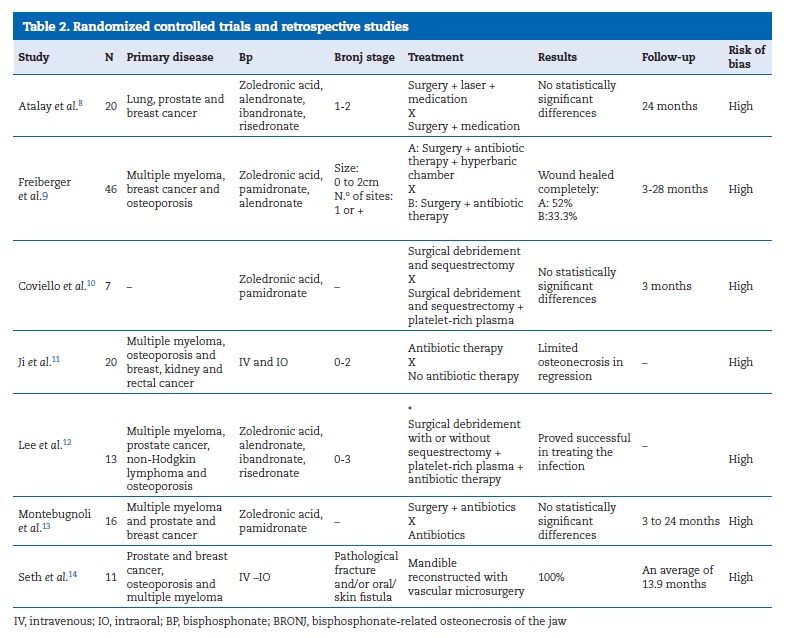
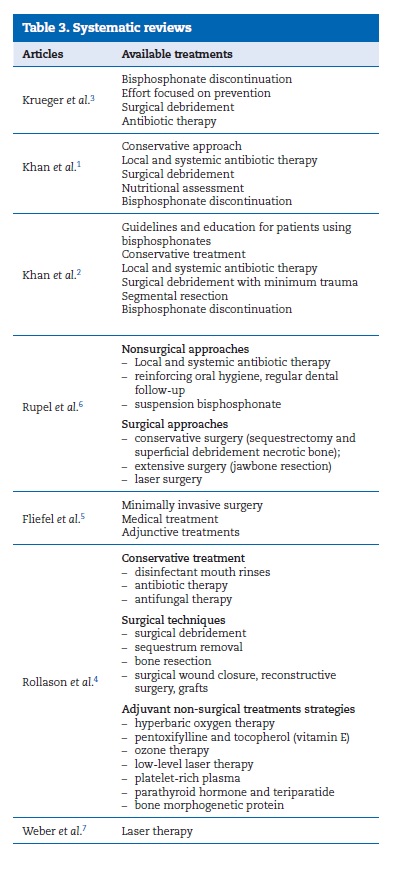
According to the Critical Appraisal Skills Programme (CASP) selection, 14 articles remained for the present systematic review: seven randomized controlled trials and retrospective studies (Table 2), and seven systematic reviews (Table 3).
�
�
�
Discussion
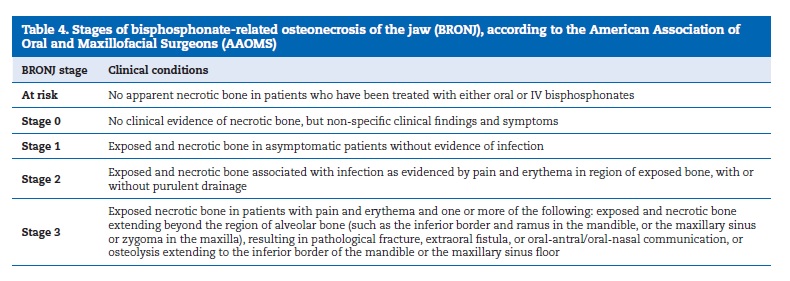
The first cases of BRONJ were described in 2003, and a series of cases have been described since then.1-7 Since BRONJ affects mainly the region treated by dentists and is an emerging complication, there has been a growing concern in dentists� daily practice before the decision to make dental interventions in patients taking bisphosphonates or even to treat established BRONJ. The American Association of Oral and Maxillofacial Surgeons (AAOMS) has developed a staging system for BRONJ to help classify its stage and determine the appropriate treatment5 (Table 4).
�
�
The number of studies with high‑level evidence for BRONJ therapy is small. Evidence quality is generally poor, mainly because of the numerous doubts associated with the condition, from its pathophysiology and diagnosis to its effective treatment and prevention of recurrence. Patients with BRONJ should be submitted to oral rehabilitation to maintain or recover their normal nutritional status, which is often compromised prior to the diagnosis, and to improve their quality of life.1,4 Currently, the diagnosis is clinical, and the radiographic and tomography images present radiolucent images characterized by regions of necrotic, devitalized bone. However, radiographic and tomography images are important to determine the actual area affected by osteonecrosis and, consequently, to discard other bone lesions thus helping to classify the BRONJ stage and plan the appropriate therapy.2
Since ONJ is directly related to bisphosphonates, experts suggest discontinuing the medication for at least three months.1-7
This recommendation is controversial because bisphosphonates can effectively increase bone density in cases of osteoporosis, maintain bone metastasis in remission and keep the patient free of pain and capable of carrying out many of the daily activities.
The studies included in this work do not state clearly whetherthe medication was discontinued and whether the discontinuation of BRONJ treatment was partial or total. The recommendation to discontinue the medication should be carefully considered by the medical team, the dentist, and other professionals who are treating these patients. Even a temporary discontinuation should be carefully considered because the bisphosphonate�s high affinity and incorporation in bone tissue and its long half‑life it may not allow that it�s discontinuation provides the desired effect. More studies in this area are needed since currently there is no scientific evidence to answer this question.1-7
Nowadays, the treatment of choice for BRONJ is conservative, and in vitro studies have shown that bisphosphonates are toxic to soft tissues, suggesting that they can affect healing and, consequently, expose bone tissue.2 Hence, local and systemic antibiotic therapies are the procedures of choice. This does not mean that the pathophysiology is related to microorganisms, because there is a wound in the oral cavity even when no bone is exposed. The area already contains numerous microorganisms that tend to infect the wound and complicate the initial situation. A study suggested a relationship between actinomyces and BRONJ<12 but was unable to prove it. On the other hand, another study concluded that no specific pathogen is associated with BRONJ, although antibiotics used as single therapy effectively reduce the wound size and sometimes promote total remission; the outcome may be influenced by the BRONJ stage.11
Surgical debridement is considered a conservative approach since it only removes visible necrotic tissue without traumatizing healthy areas. Its objective is to reduce the extension of microorganism colonization in the wound bed. Although there are many types of debridement (mechanical, autolytic, and chemical), the selected studies do not discuss the subject; they only mention debridement as an option. Antibiotics must be prescribed as soon as the decision to debride is taken. Also, sequestrectomy may be needed along with debridement. Sequestrectomy is a more invasive procedure but may be necessary depending on the BRONJ stage.1-7,12-14 It is a mutilating procedure and is only indicated when BRONJ severity is maximal. After sequestrectomy, the affected area needs to be reconstructed.14
This procedure is recommended only in stage 3 BRONJ, and the vascular microsurgery usually uses the fibula as a donor. Sequestrectomy is the procedure of choice for reconstructing the jaw. Nevertheless, a thorough assessment is necessary because there is a high risk of complications at the recipient site and for the patient, such as transplant of malignant tumor cells, BRONJ recurrence and graft failure.14 Despite the known risks, a partial or total mandibulectomy affects quality of life significantly. However, a mandibulectomy is sometimes necessary, and survival to the mandibulectomy is usually good. In the analyzed studies, the follow‑up period in these cases was, on average, 13.9 months.
BRONJ did not recur during the longest follow‑up of 2.5 years, but one patient died after the surgery because of cancer‑related complications and other patients had complications such as fistula, hematoma and infection, which were resolved.14
The approaches discussed so far are the classic approaches, that is, antibiotic therapy associated with a surgical procedure, from the least to the most invasive one, depending on BRONJ severity. Given the absence of total BRONJ resolution, the results of these studies are not statistically significant.
Other treatments have been described, often associated with these conventional therapies.
The use of laser therapy7-8and hyperbaric oxygen9 were suggested as adjuvant therapies. Laser therapy can remove the necrotic and infected tissue, decontaminate the area and provide biostimulation, thus accelerating the healing process and stimulating alkaline phosphatase and osteoblasts. Laser therapy is a promising treatment but, in the early stages of BRONJ, should be associated with combined therapies to be considered the gold‑standard management; however, the definition of a standard protocol is still required.7-8 Conventional therapy associated with hyperbaric oxygen9 provided statistically significant results because of the ability of the chamber to reduce edema and inflammation, act as a bactericide, and stimulate cellular mobilization, angiogenesis and tissue repair. However, more studies with larger samples and more homogeneous BRONJ stages are needed for a proper assessment of this therapy.
The use of platelet‑ rich plasma10,12 associated to laser therapy7-8 is promising, but the results are not statistically significant.
Platelet‑rich plasma is an autogenous and highly concentrated source of growth factors, which have an important role in osteoblast stimulation and angiogenesis. It mainly accelerates healing.10-12
What one can observe in the available therapies is that all of them aim to control infection, include the removal of necrotic tissue and attempt to accelerate healing, which is consistent with in vitro studies that show that bisphosphonates are toxic to soft tissues and, consequently, compromise complete healing.2 Soft tissue damage may expose bone and enable secondary infection, which is often associated with the observed complications. More studies on therapies that accelerate healing are necessary. The main cause of impaired healing remains to be discovered. It may be directly related to bisphosphonates because these drugs must be taken continuously and, even if the use is discontinued, their ability to bind to bone tissue for a long time may continue to cause damage and stimulate and/or maintain BRONJ.
The fact that bisphosphonates are directly related to ONJ characterizes the users of this medication as a risk group. This population is large and expanding, since it includes several diseases in which bisphosphonates are the treatment of choice. Additionally, osteonecrosis is irreversible. Therefore, more detailed information is necessary regarding this risk population to help determine bisphosphonate mechanism of action. In vitro and in vivo prevention and interventional studies are also needed.
Due to BRONJ being complex, there are still many doubts and longer follow‑up results analyses are required. It is difficult to control every possible bias; in fact, all studies included, after careful analysis, were considered as having a high risk of bias regarding random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, and incomplete outcome data. The identified bias were the following: 1) inconclusive study; 2) low quality of the methodological design; 3) very different follow‑up periods ranging from three to twenty‑eight months; 4) small sample size of some studies, affecting their clinical and statistical relevance; 5) short intervention period in addition to diverse methodology involving different BRONJ forms; 6) unclear description of the randomization and patient distribution processes; 7) follow‑up drop‑outs; 8) use of drugs, like corticosteroids, that may or may not affect BRONJ; 9) no double blinded or blinded therapy study. According to the Cochrane Risk of Bias tool, these factors affect both the internal and external validity of these studies. Due to high bias, the authors decided to provide only a descriptive analysis. Therefore, this systematic review does not contain a meta‑analysis.
Conclusion
� This review confirms the need for more randomized clinical studies on BRONJ treatments;
� Currently, the therapeutic approaches are based only on the recommendation of experts. Therefore, prevention is mandatory;
� Prevention and guidance programs for the patients and professionals who treat them should be developed immediately.
References
1. Khan AA, Sandor GK, Dore E, et al. Canadian consensus practice guidelines for bisphosphonate associated osteonecrosis of the jaw. J Rheumatol. 2008;35:1391‑7.
2. Khan Aa, Sandor Gk, Dore E, et al. Bisphosphonate associated osteonecrosis of the jaw. J Rheumatol. 2009;36:478‑90.
3. Krueger CD, West PM, Sargent M, Lodolce AE, Pickard AS. Bisphosphonate‑induced osteonecrosis of the jaw. Ann Pharmacother. 2007;41:276‑84.
4. Rollason V, Laverriere A, McDonald LC, Walsh T, Tramer MR, Vogt-Ferrier NB. Interventions for treating bisphosphonate‑related osteonecrosis of the jaw (BRONJ). Cochrane Databases Syst Rev. 2016;2:CD008455. doi: 10.1002/14651858. CD008455.pub2
5
6. Rupel K, Ottaviani G, Gobbo M et al. A systematic review of therapeutical
approaches in bisphosphonate‑related osteonecrosis of the jaw (BRONJ). Oral Oncol.
2014;50:1049‑57. 7. Weber JB, Camilotti RS, Ponte ME. Efficacy
of laser therapy in management of bisphosphonate‑related osteonecrosis of the
jaw (BRONJ): a systematic review. Laser Med Sci. 2016;31:1261-72. 8. Atalay B, Yalcin S, Emes Y et al. Bisphosphonate‑related
osteonecrosis: laser‑assited surgical
treatment or conventional surgery? Laser Med Sci. 2011:26:815‑23. 9. Freiberger JJ, Padilla‑Burgos R,
Mcgraw T, et al. What is the role of
hyperbaric oxygen in the management of bisphosphonate‑related osteonecrosis of the
jaw: a randomized controlled trial of hyperbaric oxygen as an adjunct to
surgery and antibiotics. J Oral Maxillofac
Surg. 2012;70:1573‑83. 10. Coviello V, Peluso F, Dehkhargani SZ, et
al. Platelet‑rich plasma improves wound healing in multiple myeloma
bisphosphonate‑associated osteonecrosis of the jaw patients. J Biol Regul Homeost Agents. 2012;26:151‑5. 11. Ji X, Pushalkar S, Li Y, Glickman R, Fleisher K, Saxena D. Antibiotic effects on bacterial profile in
osteonecrosis of the jaw. Oral Dis. 2012;18:85‑95. 12. Lee CY, Pien FD, Suzuki
JB. Identification and treatment of bisphosphonate‑associated
actinomycotic osteonecrosis of the jaws.
Implant Dent. 2011;20:331‑6. 13. Montebugnoli L, Felicetti L, Gissi DB, Pizzigallo A, Pelliccioni GA, Marchetti C. Biphosphonate‑associated
osteonecrosis can be controlled by nonsurgical management. Oral
Surg Oral Med Oral Pathol
Oral Radiol Endod.
2007;104:473‑7. 14. Seth R, Futran ND, Alam DS, Knott PD. Outcomes of vascularized bone graft reconstruction
of the mandible in bisphosphonate‑related osteonecrosis of the jaws. Laryngoscope. 2010;120:2165‑71. � Felipe
Lara Francischetti Correio
eletronico: feliplf@gmail.com � Ethical disclosures Protection of human and animal subjects. The authors declare that no experiments were
performed on humans or animals for this study. Confidentiality
of data. The authors declare that
no patient data appear in this article. Right
to privacy and informed consent. The authors declare that no patient data appear in
this article. � Conflict of interest The authors have no conflicts of interest to declare. � Article history: Received 8 December 2016 Accepted 7 August 2017 Available online 4 October 2017
