Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Rev Port Estomatol Med Dent Cir Maxilofac | 2017 | 58 (1) | 2-7
Original research
Assessment of tobacco use and tobacco cessation counseling by Portuguese dentists
Avaliação do hábito tabágico e do aconselhamento em cessação tabágica dos médicos dentistas portugueses
a Portuguese Dental Association (OMD), Portugal
b Faculty of Dental Medicine of the University of Porto (FMDUP), Porto, Portugal
c Institute of Public Health of the University of Porto (ISPUP), Porto, Portugal
Paulo Melo - dpaulomelopt@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 1
Original research
Pages - 2-7
Go to Volume
Article History
Received on 29/09/2016
Accepted on 31/12/2016
Available Online on 15/05/2017
Keywords
Original research
�
Assessment of tobacco use and tobacco cessation counseling
by Portuguese dentists
Avalia��o do
h�bito tab�gico e do aconselhamento em cessa��o tab�gica dos m�dicos
dentistas portugueses
�
Marta Resendea,b, Ot�lia Pereira-Lopesa,b, Orlando Monteiro da Silvaa, Paulo Meloa,b,c,*
aPortuguese Dental Association (OMD), Portugal
b Faculty of Dental Medicine of the University of Porto (FMDUP), Porto, Portugal
cInstitute of Public Health of the University of Porto (ISPUP), Porto, Portugal
�
�
http://doi.org/10.24873/j.rpemd.2017.05.013�
Abstract
Objectives:This study aimed to assess the tobacco use by Portuguese dentists and their intervention in their patients� tobacco prevention and cessation.
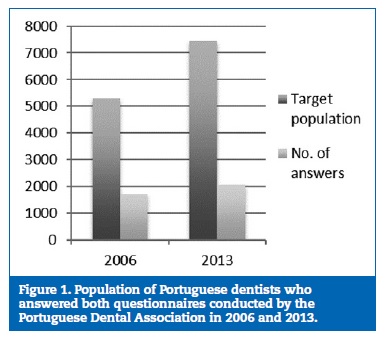
Methods:In 2006, a questionnaire was mailed to 5298 Portuguese dentists. This questionnaire focused on their tobacco use habits and their attitude toward tobacco prevention and cessation in their patients. In 2013, a second questionnaire was emailed to 7434 Portuguese dentists. Besides the same questions of the first one, it also focused on the characterization of the dentists� tobacco use habits and their perceived obstacles to tobacco prevention and cessation in patients. The data were analyzed using the Pearson�s chi-square test.
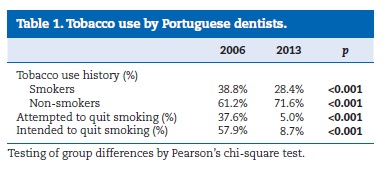
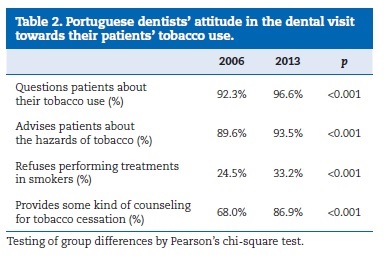
Results:A total of 1704 (32.2%) and 2048 (27.5%) inquiries answered the questionnaires completely in 2006 and 2013, respectively. Tobacco use was more frequent (p<0.001) among the dentists of the 2006 questionnaire (38.8% vs. 28.4%), who also showed more attempts and intents to quit smoking (p<0.001). The attitude toward their patients� tobacco use habits was stronger in the dentists of the 2013 questionnaire (p<0.001). The 2013 questionnaire�s results revealed that only a few of the inquiries knew the 5As approach (17.0%) and prescribed pharmacological aids to quit smoking (4.0%) or a nicotine replacement therapy (12.0%).
However, most of them showed potential interest in attending training sessions to learn how to help their patients quitting smoking.
Conclusion:Although there is a high prevalence of tobacco use among Portuguese dentists, they usually advise their patients to quit smoking. Dentists need more training in tobacco cessation.
Keywords: Education, Oral health, Tobacco cessation, Tobacco prevention, Tobacco use, Training.
�
Resumo
Objetivos:Avaliar o h�bito tab�gico e a interven��o dos m�dicos dentistas portugueses na preven��o e cessa��o tab�gica dos seus pacientes.
M�todos: Em 2006 foi enviado um question�rio por correio para 5298 m�dicos dentistas sobre o seu consumo tab�gico e a sua atitude relativamente a preven��o e cessa��o tab�gica nos seus pacientes. Em 2013 foi enviado outro inqu�rito por e-mail para 7434 m�dicos dentistas. Neste inqu�rito acrescentaram-se perguntas para a caracteriza��o do consumo tab�gico do medico dentista e dos obst�culos na preven��o e cessa��o tab�gica nos pacientes. Os dados foram analisados com o teste do qui-quadrado de Pearson.
Resultados: Foram obtidas 1704 (32,2%) e 2048 (27,5%) respostas completas em 2006 e 2013, respetivamente. O consumo de tabaco era mais frequente (p<0,001) nos m�dicos dentistas do inqu�rito de 2006 (38.8% vs 28.4%), que apresentaram tamb�m mais tentativas e inten��es para cessar o consumo (p<0,001). A conduta relativamente ao consumo tab�gico dos seus pacientes e mais vincada nos m�dicos dentistas do inqu�rito de 2013 (p<0,001). O question�rio de 2013 revelou que apenas poucos conhecem a abordagem 5A (17%) e prescrevem ajuda farmacol�gica para deixar de fumar (4%) ou uma terapia de reposi��o nicotinica (12%). Contudo, a maioria mostra interesse em participar em a��es de forma��o para se preparar para ajudar os seus pacientes na cessa��o tab�gica.
Conclus�o: Existe uma elevada preval�ncia de consumo tab�gico entre os m�dicos dentistas portugueses mas habitualmente estes aconselham os seus pacientes a deixarem de fumar. Torna-se necess�rio uma maior forma��o dos m�dicos dentistas em cessa��o tab�gica.
Palavras-chave: Formacao, Saude oral, Cessacao tabagica, Prevencao tabagica, Consumo tabagico, Ensino.
�
Introduction
The control and prevention of tobacco use are two priority objectives of the European Union�s public health due to the several problems that tobacco use causes in the whole body.1,2
Tobacco has more than 4000 components that accumulate toxic, irritant, and carcinogenic effects on the body�s cells and tissues, as well as physical and psychic dependence. Accordingly, tobacco is considered one of the main causes of death and preventable diseases.1,3 Tobacco use causes several health problems in the different parts of the body, including oral diseases.
The oral manifestations of using tobacco range from mild conditions, such as halitosis and pigmentation, to more severe ones, such as oral cancer (of which it is the main risk factor).4,5
It is well known that tobacco is associated with other oral lesions affecting the soft and hard tissues, including potentially malignant lesions (leukoplakia, erythroplakia), tobacco keratosis, nicotinic stomatitis, and periodontitis, as well as tooth loss and failure in the rehabilitation with dental implants.
Dental caries (which is more frequent in the cervical surface of the tooth), smoker�s melanosis in the gums and jugal mucosa, and hairy tongue are other oral manifestations caused by the continuous exposure to tobacco components.2,6
In tobacco users, the immune system�s response to oral infections is reduced, and the response to treatments seems less favorable (this latter association is still controversial).2,6,7
Furthermore, the children of women who smoke through their pregnancy have higher risk of congenital anomalies, such as cleft lip and palate.6
Due to the previously mentioned reasons, tobacco cessation should be advised to every patient who smokes.2,3,8 Dentists have a privileged position in tobacco prevention and cessation, as they are one of the health care professionals who are more often and for a longer period with their patients. Furthermore, they can easily show the manifestations of tobacco use from a clinical perspective, since the oral cavity is one of the areas with most repercussions and these are easily observed.1
In the clinical approach to a smoker, two types of intervention can be used: the opportunistic intervention, which can be routinely performed by any health care professional during their clinical practice, and the intensive support intervention, which is carried out by skilled and trained professionals.
In their brief opportunistic intervention, dentists should approach the tobacco use problem for about 2 minutes every time they meet with the patient, and, if the patient is a smoker, they should conduct a brief intervention of approximately 10 minutes. This intervention should be based on the 5As model, which consists of five components: ask, advise, agree, assist, and arrange; thus, the clinical algorithms that structure the intervention based on that model can be applied.3
The intensive support intervention requires a longer approach conducted throughout several sessions and specifically planned for patients who want to quit smoking.1
Studies on cessation programs conducted by dentists show success rates comparable to those developed in other primary health care areas.9 However, dentists encounter several obstacles in tobacco cessation interventions, namely, the lack of postgraduate and undergraduate training.10
The Portuguese Dental Association (PDA, Ordem dos Medicos Dentistas) has been paying attention to this important issue throughout the working group created in 2003 and has been trying to understand the dentists� behavior.
This study aimed to compare the Portuguese dentists� smoking habits in 2006 and 2013, characterize their attitude toward and intervention in tobacco prevention and cessation, and identify obstacles to that intervention.
Material and Methods
The target population of this analytical and descriptive longitudinal study was composed of all the dentists who were members of the PDA. In 2006, a questionnaire was mailed to all 5298 Portuguese dentists who were PDA members. This anonymous and individual questionnaire focused on their tobacco use habits and their attitude toward tobacco prevention and cessation in their patients. The questionnaire was accompanied by an addressed and posted envelope to facilitate the dentist�s collaboration.
In 2013, a second questionnaire was emailed to 7434 Portuguese dentists who were PDA members. This anonymous questionnaire was available online for a month, and each inquiry could only complete it once. This questionnaire, besides the dentist�s tobacco use history and their attitude toward tobacco prevention and cessation in their patients, also included a characterization of the dentist�s tobacco use and the obstacles encountered in conducted interventions.
All answers received by mail in 2006 and all filled online in 2013 were considered valid. Our sample can be considered a convenience sample. The questionnaires are available attached to the online publication (Appendices 1 and 2).
The statistical software SPSS 21.0 (Statistical Package for Social Science) was used to analyze the collected data. The categorical variables were described by frequency (%) and analyzed using the Pearson�s chi‑square test. Descriptive statistical techniques (tables) were used to organize the data. The decision rule consisted in detecting statistically significant evidence for probability values (test�s proof value) lower than 0.05.
Results
A total of 1704 (32.2%) and 2048 (27.5%) inquiries answered the questionnaires completely in 2006 and 2013, respectively (Figure 1). The inquiries� age varied between 23 and 70 in 2006 and 23 and 59 in 2013.
�
�
�
�
Tobacco use was statistically significantly more frequent (p<0.001) among the dentists who answered the 2006 questionnaire (38.8%), comparing with those who answered the 2013 questionnaire (28.4%), as shown in Table 1. The percentage of dentists who referred in 2006 having attempted and/or intended to quit smoking was also statistically significantly higher than that of the ones who answered the 2013 questionnaire (p<0.001) (Table 1).
�
�
�
�
The attitude toward approaching their patients� tobacco use habits was stronger in the dentists that answered the 2013 questionnaire (Table 2). Particularly, 96.6% (vs. 92.3%) asked about their patients� tobacco use, 93.5% (vs. 89.6%) advised their patients about the hazards of tobacco, and 86.9% (vs. 68%) provided some kind of tobacco cessation counseling. Also, more dentists in 2013 (33.2% vs. 24.5%) had refused to treat patients who smoked. These differences were statistically significant (p<0.001) in every variable that characterized the dentists� attitude toward their patients� tobacco use (Table 2).�
�
�
�
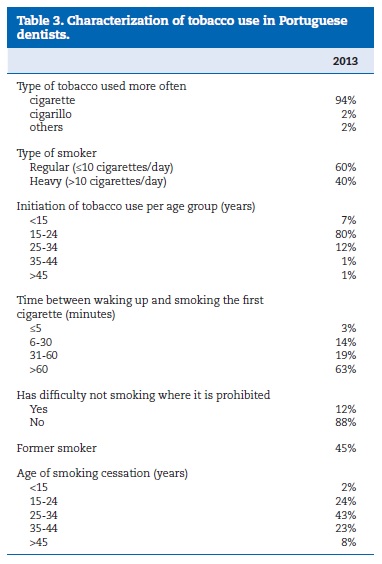
The 2013 questionnaire�s results allowed characterizing the tobacco use by Portuguese dentists. The cigarette was the inquiries� preferred type of tobacco (94.0%), almost half of them were former smokers (45.0%), most of those who still smoked were regular smokers, and the vast majority started using tobacco in the transition from adolescence to adulthood (Table 3).
�
�
�
�
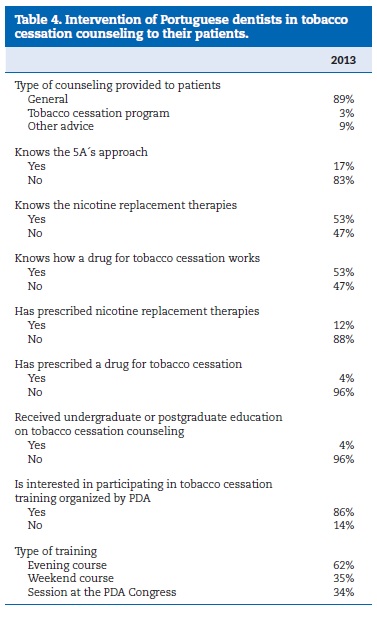
Regarding the approach to their patients, only a few of the inquiries knew the 5As approach (17.0%) and prescribed pharmacological aids to quit smoking (4.0%) or a nicotine replacement therapy (12.0%). About 96.0% of the inquiries thought they did not have enough undergraduate of postgraduate education to help their patients quitting smoking, and 86.0% showed potential interest in attending training sessions on that matter (Table 4).
�
�
�
�
Discussion
The questionnaire conducted to Portuguese dentists in 2006 was aimed to characterize their own tobacco use history and their attitude in the dental visit toward their patients� tobacco use. The questionnaire carried out to dentists in 2013 was aimed, on the one hand, to assess the differences between the dentist�s profiles of 2006 and 2013 regarding the same variables and, on the other hand, to characterize their attitude toward and intervention in tobacco prevention and cessation, while identifying the obstacles to that intervention. Moreover, this last questionnaire was also intended to assess the effects of tobacco use by these health care professionals on their tobacco cessation counseling.10
The fact that this study depended on the collaboration of the inquiries obviously influenced the sample size and can slightly influence the final results; however, this also happens in studies with similar designs.1112 Despite this limitation, a representative sample of the Portuguese dentists was obtained,since 32.5% and 27.5% of the dentists answered the 2006 and 2013 questionnaires, respectively.13
Contrary to other studies10,16 that showed less tobacco use by dentists comparing to the general population, tobacco use by Portuguese dentists is higher than in the Portuguese general population. Tobacco use among the inquired Portuguese dentists (28.4%) decreased about 10% in 7 years. Nevertheless, this percentage remains higher than that of tobacco use in the Portuguese general population aged over 15 years, which was reported to be 23% in the 2012 Eurobarometer study by the European Commission14 and 20.9% in the last Portuguese National Health Survey conducted in 2009.15
The greater proportion of dentists that had quit smoking (45%) comparing to that of the general population (15%) was a positive sign observed in this study,1 as it may represent better knowledge and awareness of the hazard effects of tobacco to health.
Regarding the Portuguese dentists� attitude toward tobacco cessation counseling to their patients, the vast majority provided brief counseling, such as asking about the patient�s tobacco use, informing them on its hazards, and advising them to quit smoking; this was also reported in other countries. 17,18
Although it is agreed that dentists have a relevant role in advising the patient who smokes,17 only a few of them support or help the patient who wants to quit smoking actually to do it. However, several studies show that the use of evidence‑based guidelines on their interventions helps clinicians to help effectively their patients reducing and quitting smoking. 8,19,20 Other studies also show that dentists can achieve tobacco cessation as effectively as professionals of other primary health care areas (physicians and nurses) 7,21 and, thus, more attention should be paid to the role of the dentist in interventions within this area.
Regarding dentists� tobacco use characterization, most of them smoked cigarettes, and only a few smoked another type of tobacco. In further studies, it could be interesting to assess the use of electronic cigarettes, as these are a current option.
According to the Portuguese Directorate‑General of Health(DGS, Direcao‑Geral de Saude), every health care professional is responsible for promoting healthy lifestyles and providing preventive care to the population, regardless of the type of care they provide and their workplace, particularly concerning tobacco prevention and treatment. 2 Due to the sensitivity and importance of this subject, as well as to the role dentists may play in it, PDA has dedicated itself to this matter in the past years, having even created a workforce for it. This workforce had as it main actions the participation and organization of tobacco prevention and control initiatives and the production and provision of different sources of information on the subject to dentists and the general public. Examples of those actions are the organization of events to celebrate the world no tobacco day and the project of early intervention on oral cancer, the participation in the technical consulting group of the DGS Tobacco Prevention and Control Program and in every event organized by this group, the participation in several television programs on that matter, the translation into Portuguese of the World Dental Federation (FDI) guide for oral health care professionals �Tobacco and Oral Health�, the elaboration of an algorithm for the clinical intervention in tobacco cessation, and the production of educational leaflets and articles on the matter published via email to every dentist or in the official website of PDA.
In the fight to tobacco use, it is important to use intervention algorithms as patients may be still unaware of tobacco�s association with oral diseases and may get tobacco cessation counseling in dental offices. Applying an algorithm leads to better knowledge of this association and somewhat promotes the patient�s acceptance to the counseling provided by the dentist. In fact, several studies have already referred that patients considered tobacco cessation counseling by dentists to be favorable. 22,23 Furthermore, if adapted to dentistry, algorithms become instructive and easy to apply by the dentist, summarizing the primary steps in this type of intervention.1
This study was also aimed to identify obstacles or barriers to the application of tobacco prevention and cessation interventions.
One of those obstacles was the lack of training and education in tobacco cessation, which had already been mentioned in several studies. 10,11,16,24 However, other studies indicate that the main obstacles encountered by dentists for providing tobacco cessation interventions are time/cost ratio, feeling of ineffectiveness or discouragement, fear of interfering with the doctor‑patient relationship, communication style, and smoker�s resistance and lack of motivation. Motivation, visits costs, costs of drug therapies that are not reimbursed by the national health system and are similar to the monthly cost of 20 cigarettes/day, the overburden of the visits, the first attempts, and psychiatric pathologies are the main obstacles encountered by the person who wants to quit smoking. 12,24
In most countries, including Portugal, dentists continue to promote tobacco cessation actively, and the training they receive is not enough. There is a general agreement on the lack of training in tobacco cessation in the education of dentists. A large part of the education on tobacco cessation is focused on a very brief intervention, and most courses do not provide counseling for tobacco cessation. In fact, this education is not comprehensive or systematic. Moreover, much of the efforts are focused on the consequences of smoking, and little attention is paid to tobacco cessation actions.25
New curricula are now being implemented in dental medicine faculties across Europe and many other parts of the world, focused on tobacco use knowledge and methods to promote the adoption and incorporation of tobacco cessation counseling in the clinical practice during education.26
Conclusion Although there is a high prevalence of tobacco use among Portuguese dentists, these usually advise their patients to quit smoking. Dentists need urgently more training, namely postgraduate training, in tobacco prevention and cessation, in order to improve their intervention with their patients.
�
References
1. Nunes E. Programa Nacional para a prevencao e controlo do tabagismo. Lisboa: Direcao‑Geral de Saude, 2012.
2. Nunes E, Candeias A, Mendes B, Pardal C, Fonseca J, Oliveira L, et al. Cessacao tabagica � Programa tipo de actuacao. Lisboa: Direcao Geral da Saude/Gradiva, 2007.
3. Cesar Neto JB, Rosa EF, Pannuti CM, Romito GA. Smoking and periodontal tissues: a review. Braz Oral Res. 2012;26(Suppl 1):25‑31.
4. Fiorini T, Musskopf ML, Oppermann RV, Susin C. Is there a positive effect of smoking cessation on periodontal health? A systematic review. J Periodontol. 2014;85:83‑91.
5. Warnakulasuriya S, Dietrich T, Bornstein MM, Casals Peidro E, Preshaw PM, Walter C, et al. Oral health risks of tobacco use and effects of cessation. Int Dent J. 2010;60:7‑30.
6. Chambrone L, Preshaw PM, Rosa EF, Heasman PA, Romito GA, Pannuti CM, et al. Effects of smoking cessation on the outcomes of non‑surgical periodontal therapy: a systematic review and individual patient data meta‑analysis. J Clin Periodontol. 2013;40:607‑15.
7. Gorin SS, Heck JE. Meta‑analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol Biomarkers Prev. 2004;13:2012‑22.
8. Carr AB, Ebbert J. Interventions for tobacco cessation in the dental setting. Cochrane Database Syst Rev. 2012;6:CD005084.
9. Johnson NW, Lowe JC, Warnakulasuriya KA. Tobacco cessation activities of UK dentists in primary care: signs of improvement. Br Dent J. 2006;200:85‑9.
10 10. Casals Peidro E, Otero Romero S, Cuenca Sala E. Prevalence of smoking among dentists in Catalonia�Spain 2006. Literature review of smoking cessation practices in the dental office. Med Oral Patol Oral Cir Bucal. 2008;13:E671‑7.
11. Binnal A, Rajesh G, Denny C, Ahmed J. Insights into the tobacco cessation scenario among dental graduates: an Indian perspective. Asian Pac J Cancer Prev. 2012;13:2611‑7.
12. Prakash P, Belek MG, Grimes B, Silverstein S, Meckstroth R, Heckman B, et al. Dentists� attitudes, behaviors, and barriers related to tobacco‑ use cessation in the dental setting. J Public Health Dent. 2013;73:94‑ 102.
13. Burgess TF. A general introduction to the design of questionnaires for survey research. Leeds: University of Leeds, 2001.
14. TNS Opinion & Social. Special Eurobarometer 385: Attitudes of Europeans towards tobacco. Brussels: European Commission, 2012.
15. Instituto Nacional de Estatistica (INE). Census 2009: Resultados definitivos. Lisboa: INE, 2010.
16. Antal M, Forster A, Zalai Z, Barabas K, Ramseier C, Nagy K. Attitudes of Hungarian dental professionals to tobacco use and cessation. Cent Eur J Public Health. 2012;20:45‑9.
17. Reis I, Fortuna P, Ascencao R, Bugalho A, Costa J, Carneiro A. Normas de Orientacao Clinica. Lisboa: Centro de Estudos de Medicina Baseada na Evidencia � Faculdade de Medicina de Lisboa, 2008.
18. Ebn Ahmady A, Khoshnevisan MH, Heidari N, Lando HA. Dentists� familiarity with tobacco cessation programs in dental settings in Iran. J Public Health Dent. 2011;71:271‑7.
19. Albert D, Ward A. Tobacco cessation in the dental office. Dent Clin North Am. 2012;56:747‑70.
20. Walsh MM, Belek M, Prakash P, Grimes B, Heckman B, Kaufman N, et al. The effect of training on the use oftobacco‑use cessation guidelines in dental settings. J Am Dent Assoc. 2012;143:602‑13.
21. Watt RG, Johnson NW, Warnakulasuriya KA. Action on smoking�opportunities for the dental team. Br Dent J. 2000;189:357‑60.
22. United States Public Health Service. Treating tobacco use and dependence: 2008 update U.S. Public Health Service Clinical Practice Guideline executive summary. Respir Care. 2008;53:1217‑22.
23. Sood P, Narang R, Swathi V, Mittal L, Jha K, Gupta A. Dental patient�s knowledge and perceptions about the effects of smoking and role of dentists in smoking cessation activities. Eur J Dent. 2014;8:216‑23.
24. Rosseel JP, Jacobs JE, Hilberink SR, Maassen IM, Segaar D, Plasschaert AJ, et al. Experienced barriers and facilitators for integrating smoking cessation advice and support into daily dental practice. A short report. Br Dent J. 2011;210:E10.
25. Ramseier CA, Christen A, McGowan J, McCartan B, Minenna L, Ohrn K, et al. Tobacco use prevention and cessation in dental and dental hygiene undergraduate education. Oral Health Prev Dent. 2006;4:49‑60.
26. Davis JM, Ramseier CA, Mattheos N., Schoonheim‑Kleim M, Compton S, Al‑Hazmi N, et al. Education of tobacco use prevention and cessation for dental professionals � a paradigm shift. Int Dent J. 2010;60:60‑72.
�
Paulo Melo
E-mail address: dpaulomelopt@gmail.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflicts of interest
The authors have no conflicts of interest to declare.
�
Acknowledgments
The authors would like to thank Prof. Sergio Matos, Prof. Ricardo Faria e Almeida, Prof. Isabel Poiares Batista, Dr. Jose Frias Bulhosa, Prof. Eunice Carrilho, and Dr. Luis Filipe Correia.
�
Appendices. Supplementary content
Supplementary data associated with this article can be found, in> the online version, at http://doi.org/10.24873/j.rpemd.2017.05.013.
�
Article History
Received 29 September 2016
Accepted 31 December 2016
Available online 30 March 2017