
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 72-77
Clinical case
Nonsurgical endodontic treatment of misdiagnosed odontogenic cutaneous sinus tracts: Two case reports
Tratamento endodôntico não cirúrgico de fístulas cutâneas odontogénicas mal diagnosticadas: Dois casos clínicos
a Istanbul Medeniyet University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
b Istanbul University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
c Istanbul Nisantasi University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
?kbal Sena Çelebi Keskin - ikbal.celebi@medeniyet.edu.tr
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Clinical case
Pages - 72-77
Go to Volume
Article History
Received on 31/07/2024
Accepted on 24/05/2025
Available Online on 29/06/2025
Keywords
Clinical Case Report
�
Nonsurgical endodontic treatment of misdiagnosed odontogenic cutaneous sinus tracts: Two case reports
Tratamento endod�ntico n�o cir�rgico de f�stulas cut�neas odontog�nicas mal diagnosticadas: Dois casos cl�nicos
�
İkbal Sena �elebi Keskin1,* 0000-0002-5243-9176
Turgut Yağmur Yal�ın2 0000-0001-9737-9499
Fehmi Raif Erişen3 0000-0002-1146-6979
1Istanbul Medeniyet University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
2Istanbul University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
3Istanbul Nisantasi University, Faculty of Dentistry, Department of Endodontics, Istanbul, Turkey
�
�
Article history:
Received 31 July 2024
Accepted 24 May 2025
Available online 16 June 2025
�
Abstract
Odontogenic cutaneous sinus tracts of endodontic origin can be clinically mistaken for various other diseases. Accurate diagnosis of this clinical presentation is crucial for delivering appropriate care because misdiagnosis can lead to healing failure or unnecessary treatment. Because sinus tracts of odontogenic origin can arise from various dental issues, a dental etiology must be considered for any sinus tract on the face or neck. The presente report describes two cases of odontogenic cutaneous sinus tracts that were initially misdiagnosed but were then successfully treated with nonsurgical endodontic therapy. These cases emphasize the importance of accurate diagnosis and the utility of cone-beam computed tomography for identifying the origins of odontogenic cutaneous sinus tracts. This approach avoids unnecessary treatment and ensures effective management of odontogenic infections. Effective communication between medical and dental practitioners is crucial for proper diagnosis and treatment, prevention of chronicity, and ensuring patient recovery.
Keywords:
Diagnostic errors, Endodontics, Periapical abscess, Root canal therapy
�
Resumo
As f�stulas cut�neas odontog�nicas de origem endod�ntica podem ser facilmente confundidas com outras condi��es cl�nicas. O seu diagn�stico preciso � essencial para a presta��o de cuidados adequados, dado que um diagn�stico incorreto pode resultar no insucesso da recupera��o ou na administra��o de tratamentos desnecess�rios. Dada a variedade de problemas dent�rios que podem originar f�stulas odontog�nicas, � fundamental ter em conta a etiologia dent�ria em qualquer caso de f�stula na face ou no pesco�o. O presente descreve dois casos de f�stulas cut�neas odontog�nicas que foram inicialmente diagnosticadas de forma incorreta, sendo posteriormente tratadas com sucesso atrav�s de tratamento endodontico n�o cir�rgico. Estes casos sublinham a import�ncia de um diagn�stico rigoroso e da tomografia computadorizada de feixe c�nico como ferramenta valiosa para identificar a origem das f�stulas. Al�m de prevenir tratamentos desnecess�rios, esta abordagem garante uma gest�o eficaz das infe��es odontog�nicas. A colabora��o estreita entre m�dicos e m�dicos dentistas � imprescind�vel para um diagn�stico e tratamento adequados, prevenindo a cronicidade e garantindo a recupera��o do paciente.
Palavras-chave: Diagn�stico incorreto,Endodontia,Abcesso periapical,Terapia de canal radicular
�
Introduction
A sinus tract is described as a pathway that originates from a localized inflammatory area and extends to the epithelial surface.1 Sinus tracts of odontogenic origin can arise from various dental issues, including pulpal infections, chronic apical periodontitis, root fractures, chemical irritation, and dental trauma.2, 3 During the formation of an odontogenic sinus tract, the infected material perforates the bone, traverses the soft tissue along the path of least resistance, and drains externally.4, 5 Depending on the proximity of the apex to the cortical plates and/or bone density, the stoma can form on the attached gingiva, alveolar mucosa, or gingival sulcus of the buccal or lingual surfaces.4 In some cases, the infection may also drain cutaneously through a sinus tract.5
Odontogenic cutaneous sinus tracts (OCSTs) are noted to occur four times more frequently in the lower jaw than in the upper jaw.3, 6 The OCST location depends on the site of cortical-plate perforation caused by the inflammatory processes and its connection to facial muscle attachments.5, 7 Clinically, these lesions typically manifest as purulent papules or nodules in the submental, submandibular, cervical, or retromandibular regions.3, 4 However, OCSTs have also been reported in the chin, cheek, nasal philtrum, canine space, nasolabial folds, nostrils, infraorbital region, and neck.5 7 - 11
A thorough differential diagnosis is important to ensure proper management of OCST lesions. The differential diagnoses of OCST include bacterial infections, malignancies, osteomyelitis, pyogenic granulomas, congenital fistulas, local skin infections (e.g., carbuncles, infected epidermoid cysts), chronic tuberculosis, mycotic infections, tertiary syphilis gummas, and furuncles.3, 12 - 14 These conditions should be carefully considered to avoid a misdiagnosis.
Although OCSTs have been previously described, their atypical appearance poses diagnostic challenges.15 Moreover, in the absence of dental symptoms, patients often consult dermatologists, otolaryngologists, and plastic surgeons, where atypical presentation may lead to an initial misdiagnosis.16, 17
A misdiagnosis commonly leads to unnecessary treatments, such as a variety of antibiotic protocols, surgical excisions, biopsies, and even radiotherapy, exacerbating the chronicity of the lesion and affecting facial aesthetics owing to scarring and dimpling.3, 18
Herein, we highlight two cases of OCSTs that were initially misdiagnosed but were then effectively treated with nonsurgical endodontic therapy after dental referral.
Case reports
Case 1
A healthy 18-year-old woman with no systemic conditions presented to the Department of Endodontics at the Faculty of Dentistry of Istanbul University, Turkey, with a complaint of extraoral swelling and a recurring wound in the right submandibular region. The patient reported undergoing three surgical procedures in the affected area performed by an otolaryngologist over the past 2 years, with the most recent one occurring 3 months before her dental visit. The patient rarely visited the dentist and had not attended a dental appointment for 3 years before this complaint.
Extraoral examination revealed active drainage from the submandibular region (Figure 1), although the patient reporte no associated pain. Intraoral examination revealed extensive restorations in the mandibular right posterior teeth. Her soft tissues, including the gingival tissues, appeared healthy with no signs of inflammation or bleeding. Panoramic and periapical radiographs revealed an extensive periapical radiolucency associated with teeth 46 and 47 (Figure 2). Electrical pulp and cold tests conducted on the relevant teeth resulted in negative responses. Considering that the extraoral infection could have originated from the teeth in that area, a cone-beam computed tomography (CBCT) was performed for thorough assessment.
�

Figure 1. Extraoral view of the odontogenic cutaneous sinus tract located in the submandibular region.
�

Figure 2. An orthopantomogram shows a radiolucent region located at the apex of the mandibular left second molar.
�
The CBCT revealed that the periapical lesion on tooth 47 had perforated the lingual cortical bone (Figures 3 and 4), suggesting the possibility of an OCST caused by a periapical infection in the corresponding tooth. Root canal treatment of tooth 47 was initiated under local anesthesia with rubber dam isolation. The previous restoration was carefully removed, and an endodontic access cavity was prepared using round standard diamond burs. The root canals were prepared using manual files (Dentsply Maillefer, Ballaigues, Switzerland) and ProTaper Next rotary nickel-titanium instruments (Dentsply Maillefer, Ballaigues, Switzerland). Between each file, the area was irrigated with 2 mL of 2.5% sodium hypochlorite. Then, an intracanal calcium hydroxide dressing (Ultracal XS, Ultradent Products, South Jordan, UT, USA) was carefully applied.
�

Figure 3. Sagittal view of cone-beam computed tomography.
�

Figure 4. Coronal view of cone-beam computed tomography
�
Two weeks later, the amount of fluid draining from the extraoral area had decreased, and initial wound healing was observed. Following irrigation and cleaning of the canals with 5.25% sodium hypochlorite, 17% ethylenediaminetetraacetic acid (EDTA), and distilled water, calcium hydroxide was reapplied for 2 weeks.
One month after the initial visit, the sinus tract showed no evidence of drainage. Final irrigation was performed using 5.25% sodium hypochlorite, 17% EDTA, and distilled water.
Then, the canals were obturated using the lateral condensation technique with gutta-percha (Dentsply Maillefer, Ballaigues, Switzerland) and AH Plus root canal sealer (Dentsply, DeTrey, Konstanz, Germany). The patient was referred to a restorative dentist for permanent restoration. However, the scar tissue resulting from the previous surgeries persisted. At the 1-year follow-up, no recurrence of infection was noted (Figure 5). Although the scar from the previous surgeries persisted, the patient expressed satisfaction with the aesthetic outcome and declined referral to a dermatologist for further evaluation or cosmetic intervention.
�

�
Figure 5. Postoperative follow-up at 1 year. Healing of the skin lesion with scarring formation.
Case 2
A systemically healthy 20-year-old woman presented to the Department of Endodontics at the Faculty of Dentistry of Istanbul Medeniyet University, Turkey, with left submandibular swelling and skin lesions. The patient reported having undergone three surgical procedures for the skin lesion performed by two different otorhinolaryngologists over the past 2 years.
Extraoral examination revealed active drainage in the left submandibular region (Figure 6). The patient had not seen a dentist for over 3 years before the symptoms started.
�

Figure 6. Extraoral photograph shows a sinus tract in the submandibular area.
�
Intraoral examination revealed initial signs of gingival inflammation in the soft tissues, such as slight redness and swelling, but no bleeding upon probing. Overall, oral hygiene was inadequate. Clinical and radiographic evaluations revealed deep caries in teeth 35 and 37, inadequate root canal treatment in tooth 36, and periapical lesions in teeth 36 and 37 (Figure 7). The teeth exhibited no sensitivity to palpation or percussion. A CBCT was performed for a more comprehensive evaluation. Based on the CBCT findings, the patient was diagnosed with OCST caused by a periapical infection in the mandibular left second molar (Figure 8).
�

Figure 7. The orthopantomogram shows a radiolucent area near the apex of the mandibular left second molar.
�
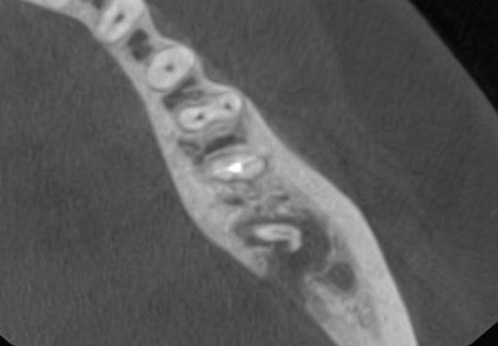
Figure 8. Axial view of cone-beam computed tomography.
�
Root canal treatment of tooth 36 was initiated under local anesthesia with rubber dam isolation. An endodontic access cavity was prepared using round standard diamond burs. The root canals were shaped using hand files (Dentsply Maillefer, Ballaigues, Switzerland) and Mtwo nickel-titanium rotary files (VDW, Munich, Germany). Irrigation was performed using 2 mL of 5.25% sodium hypochlorite between each file. Then, calcium hydroxide (Ultracal XS, Ultradent Products, South Jordan, UT, USA) was applied as an intracanal medicament (Figure 9).
�
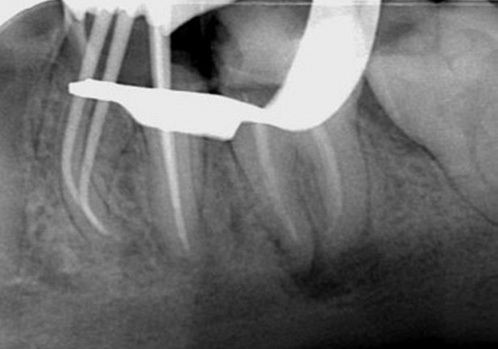
Figure 9. Periapical radiographs taken during root canal treatment.
�
The patient postponed the second appointment due to a holiday, so it took place two months after the initial visit. By then, symptoms had disappeared, and drainage ceased (Figure 10). Final irrigation and obturation were completed as performed in Case 1. Following the completion of the root canal treatment, the patient was referred to a restorative dentist for the final restoration of the respective tooth.
�

Figure 10. Extraoral photograph at the 2-month follow-up.
�
At the 1-year follow-up, no recurrence of infection was noted. Even though the scar from previous surgeries persisted, the patient declined referral to a dermatologist, expressing satisfaction with the aesthetic outcome. Periapical healing was radiographically confirmed at the 1-year follow-up (Figures 11 and 12).
�

Figure 11. Radiograph at the 6-month follow-up.
�

Figure 12. Postoperative follow-up at 1 year. Healing of the skin lesion with scarring.
�
Discussion and conclusions
Pulp infection, chronic apical periodontitis, dental trauma, root fracture, and peri-implantitis can lead to inflammatory bon� resorption, resulting in erosion of the alveolar bone.19 - 22 As the infection progresses, it navigates peripherally and eventually perforates the cortical bone. Thereafter, it passes through fascial spaces and muscle attachments, ultimately exiting cutaneously.12
The diagnosis of OCSTs presents significant challenges in daily dental practice. These lesions often manifest far from their primary dental origin, lack characteristic symptoms, and can be mistaken for dermatological or systemic conditions, delaying proper diagnosis.16 Moreover, the absence of obvious dental symptoms, such as pain or swelling, can obscure their odontogenic etiology and result in misdiagnosis. The mischaracterization of these lesions as chronic skin conditions further complicates an accurate identification.4
The insertion of gutta-percha cones or other radiopaque materials in the sinus tract is helpful for radiographically determining its origin and should be routinely performed. In a previous study, sinus tract angiography was successfully used to diagnose a sinus tract distant from the affected area.3 High-resolution ultrasound has also been reported as a non-invasive and precise imaging method for identifying OCSTs.6 Additionally, pulp sensitivity tests must be performed to determine whether the infection originates from necrotic pulp tissue.10 These strategies are useful for avoiding a misdiagnosis. CBCT is widely employed in endodontics to evaluate complex root canal morphologies, identify root resorption and fractures, and perform preoperative assessments in cases of surgical retreatment, planned replantation, or autotransplantation.23 It has also been used to trace OCSTs and aid in their diagnosis in several cases.18, 24, 25 In both cases presented here, CBCT was instrumental in assisting with the diagnosis.
The exclusion of periradicular pathologies related to pulpal necrosis is a critical step before initiating invasive treatments.26 If the tooth can be saved, the infection should be treated using root canal therapy; otherwise, the tooth must be extracted.27, 28 Nonsurgical root canal therapy is the preferred option and should always be attempted first.5, 7, 9 The OCST is expected to spontaneously heal within 5�14 days following root canal treatment or tooth extraction.13
In cases where the OCST has been previously treated surgically, healing may occur with scar formation. Such scarring may raise aesthetic concerns, and referral to a dermatologista for further evaluation and management could be considered.
Early identification of the source of the sinus tract prevents ineffective treatment, thus improving the recovery rate.28 Unless the origin of the infection is effectively treated, the OCST is at risk of recurrence.4, 19 In both cases presented here, diferente medical professionals had misdiagnosed the cause of the OCST, which resulted in unnecessary antibiotic therapy andsurgical procedures.
In conclusion, we reported two cases of odontogenic cutaneous sinus tracts that were initially misdiagnosed but were effectively treated with nonsurgical endodontic therapy
after dental referral. The cases presented highlight how some lesions in the head and neck can have a dental origin, often overlooked by medical professionals. Effective multidisciplinar communication, particularly involving experts in otolaryngology, plastic surgery, and dermatology, is importante to prevent treatment delays and ensure appropriate treatment.
�
References
1. Endodontists AA. Glossary: Contemporary Terminology for Endodontics. Chicago, IL: American Association of Endodontists. 1994.
2. Azizlou E, Sobhani MA, Ghabraei S, Khoshkhounejad M, Ghorbanzadeh A, Tahan SS. Extraoral sinus tracts of odontogenic origin: a case series. Front Dent. 2020;17:29.
3. Bai J, Ji AP, Huang MW. Submental cutaneous sinus tract of mandibular second molar origin. Int Endod J. 2014;47:1185-91.
4. Cohenca N, Karni S, Rotstein I. Extraoral sinus tract misdiagnosed as an endodontic lesion. J Endod. 2003;29:841-3.
5. Din�ol M, Yilmaz B, Ersev H, G�nd�z VM, Arslanoğlu B, Yal�ın T, et al. Treatment of extraoral cutaneous sinus tracts with non-surgical endodontic intervention: report of six cases. J Istanbul Univ Fac Dent. 2015;49:35-40.
6. Corvino A, Catalano O, Wortsman X, Rold�n FA, Cavallieri F, Gonzalez C, et al. High-Resolution Ultrasound of Odontogenic Cutaneous Sinus Tract: An International Multicentric Experience and a Review of the Literature. J Ultrasound Med. 2024;43:1489-99.
7. Sareen S, Pathak AK, Purwar P, Dixit J, Singhal D, Sajjanhar I, et al. Nasal sinus tract of odontogenic origin: report of a case. Case Rep Dent. 2015;1:813478.
8. Johnson BR, Remeikis NA, Van Cura JE. Diagnosis and treatment of cutaneous facial sinus tracts of dental origin. J Am Dent Assoc. 1999;130:832-6.
9. Pasternak-J�nior B, Teixeira CS, Silva-Sousa YT, Sousa-Neto MD. Diagnosis and treatment of odontogenic cutaneous sinus tracts of endodontic origin: three case studies. Int Endod J. 2009;42:271-6.
10. Tidwell E, Jenkins JD, Ellis CD, Hutson B, Cederberg RA. Cutaneous odontogenic sinus tract to the chin: a case report. Int Endod J. 1997;30:352-5.
11. Witherow H, Washan P, Blenkinsopp P. Midline odontogenic infections: a continuing diagnostic problem. Br J Plast Surg. 2003;56:173-5.
12. Cioffi GA, Terezhalmy GT, Parlette HL. Cutaneous draining sinus tract: an odontogenic etiology. J Am Acad Dermatol. 1986;14:94-100.
13. Spear KL, Sheridan PJ, Perry HO. Sinus tracts to the chin and jaw of dental origin. J Am Acad Dermatol. 1983;8:486-92.
14. Kaban LB. Draining skin lesions of dental origin: the path of spread of chronic odontogenic infection. Plast Reconstr Surg. 1980;66:711-7.
15. Varghese LL, Bhattacharya A, Sharma P, Apratim A. Nonsurgical management of an extraoral cutaneous sinus tract of odontogenic origin. BMJ Case Rep. 2020;13:e234699.
16. Sarraf P, Khoshkhounejad M, Babaahmadi M. An odontogenic cutaneous sinus tract in an unusual site with multiple misdiagnoses. Clin Case Rep. 2023;11:8049.
17. Sidhu S, Thomas AM, Kundra R. Perplexity and repercussions in maldiagnosis of an extraoral draining sinus by a physician and its dental management: a case report. Int J Clin Pediatr Dent. 2022;15:115-8.
18. Curvers F, De Haes P, Lambrechts P. Non-surgical endodontic therapy as treatment of choice for a misdiagnosed recurring extraoral sinus tract. Eur Endod J. 2017;2:13.
19. Mittal N, Gupta P. Management of extra oral sinus cases: a clinical dilemma. J Endod. 2004;30:541-7.
20. Chan CP, Chang SH, Huang CC, Wu SK, Huang SK. Cutaneous sinus tract caused by vertical root fracture. J Endod. 1997;23:593-5
21. Mishra R, Khan TS. Cutaneous sinus tract in association with traumatic injury to the teeth. Int J Clin Pediatr Dent. 2013;6:205-7.
22. Nkenke E, Amann K, Reich S, Neukam FW, Frankenberger R. Submental cutaneous sinus tract as a result of progressive peri-implantitis: a case report. J Periodontol. 2004;75:1417-23.
23. Chan F, Brown LF, Parashos P. CBCT in contemporary endodontics. Aust Dent J. 2023;68:39-55.
24. Abuabara A, Schramm CA, Zielak JC, Baratto-Filho F. Dental infection simulating skin lesion. An Bras Dermatol. 2012;87:619-21.
25. Tian J, Liang G, Qi W, Jiang H. Odontogenic cutaneous sinus tract associated with a mandibular second molar having a rare distolingual root: a case report. Head Face Med. 2015;11:13.
26. Lewin-Epstein J, Taicher S, Azaz B. Cutaneous sinus tracts of dental origin. Arch Dermatol. 1978;114:1158-61.
27. Gupta M, Das D, Kapur R, Sibal N. A clinical predicament � diagnosis and differential diagnosis of cutaneous facial sinus tracts of dental origin: a series of case reports. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e132-6.
28. Samir N, Al-Mahrezi A, Al-Sudairy S. Odontogenic cutaneous fistula: report of two cases. Sultan Qaboos Univ Med J. 2011;11:115-8.
29. Valderhaug J. A histologic study of experimentally produced intra-oral odontogenic fistulae in monkeys. Int J Oral Surg. 1973;2:54-61.
�
İkbal Sena �elebi Keskin
E-mail address: ikbal.celebi@medeniyet.edu.tr
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
İkbal Sena �elebi Keskin: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization,
Writing � original draft, Writing � review & editing. Turgut Yağmur Yal�ın: Methodology, Writing � original draft, Supervision, Visualization, Writing � review & editing. Fehmi Raif Erişen: Supervision, Validation, Writing � review & editing.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
