
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 91-96
Clinical case
Nonsurgical management of odontogenic maxillary sinusitis – Two case reports
Tratamento não cirúrgico de sinusite maxilar odontogénica – dois casos clínicos
a Federal University of Paraná, Curitiba, Paraná, Brazil
b Neurological Institute of Curitiba, Curitiba, Paraná, Brazil
Lisa Yurie Oda - yu_oda@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Clinical case
Pages - 91-96
Go to Volume
Article History
Received on 19/01/2024
Accepted on 11/05/2025
Available Online on 29/06/2025
Keywords
Clinical Case Report
�
Nonsurgical management of odontogenic maxillary sinusitis � Two case reports
Tratamento n�o cir�rgico de sinusite maxilar odontog�nica � dois casos cl�nicos
�
Andr� Luiz da Costa Michelotto1 0000-0001-7855-4407
Lisa Yurie Oda1,* 0000-0001-5203-5422
Wagner Hummig2 0000-0003-1651-6610
Antonio Batista1 0000-0002-6571-6662
1 Federal University of Paran�, Curitiba, Paran�, Brazil
2 Neurological Institute of Curitiba, Curitiba, Paran�, Brazil
�
�
Article history:
Received 19 January 2024
Accepted 11 May 2025
Available online 26 June 2025
�
Abstract
Odontogenic maxillary sinusitis is a sinus pathology secondary to maxillary dental pathologies or complications from dental procedures. Due to its clinical presentations of sinonasal symptoms, odontogenic sources may be underdiagnosed, leading to an incorrect treatment.
This report presents two cases in which odontogenic maxillary sinusitis was correctly diagnosed and treated by nonsurgical endodontic management. In both cases, the patients presented with pain or discomfort in the maxillary region, and the cone-beam computed tomography revealed thickening of the maxillary sinus membrane, which was helpful for the diagnosis and follow-up. In the first case, the tooth related to the pathology underwent primary nonsurgical endodontic treatment, while in the second case, the tooth underwent nonsurgical endodontic retreatment. In both cases, calcium hydroxide dressing was used between appointments, and the root canals were filled with gutta-percha cones and bioceramic sealer. The follow-up cone-beam computed tomography obtained 24 months later in the first case and 16 months in the second showed the absence of maxillary sinus abnormalities, and the patients presented without clinical symptoms. The clinician must be aware of the signs and symptoms related to odontogenic maxillary sinusitis to be successful in diagnosis, planning, and treatment. (Rev Port Estomatol Med Dent Cir Maxilofac.
Keywords: Endodontic,Maxillary sinusitis,Root canal therapy
�
Resumo
A sinusite maxilar odontog�nica � uma patologia sinusal secund�ria a patologias dent�rias maxilares ou complica��es de procedimentos dent�rios. Devido �s suas apresenta��es cl�nicas de sintomas nasossinusais, as origens odontog�nicas podem ser subdiagnosticadas, levando a um tratamento incorreto. Este artigo apresenta dois casos em que a sinusite maxilar odontog�nica foi corretamente diagnosticada e resolvida atrav�s da realiza��o de interven��o endod�ntica n�o cir�rgica. Em ambos os casos, os pacientes apresentavam dor ou desconforto na regi�o maxilar, tendo sido observado espessamento da membrana do seio maxilar na tomografia computadorizada de feixe c�nico, o que foi �til para o diagn�stico e seguimento. Enquanto no primeiro caso o dente relacionado com a patologia recebeu tratamento endod�ntico prim�rio n�o cir�rgico, no segundo, o dente recebeu retratamento endod�ntico n�o cir�rgico.
Em ambos os casos, foi utilizado hidr�xido de c�lcio entre as consultas, e os canais radiculares foram obturados com cones de guta-percha e cimento biocer�mico. A tomografia computadorizada de feixe c�nico de seguimento realizada ap�s 24 meses no primeiro caso e 16 meses no segundo mostrou aus�ncia de anomalias do seio maxilar, e os pacientes apresentaram-se sem sintomas cl�nicos. � importante que o profissional tenha conhecimento dos sinais e sintomas relacionados com a sinusite maxilar
odontog�nica, para que possa ter sucesso no diagn�stico, planeamento e tratamento.
Palavras-chave: Endodontia, Sinusite maxilar,Tratamento do canal radicular
�
Introduction
Dental pain is the most frequent cause of orofacial pain.1 It can mimic other types of facial pain because the dental pathology may refer pain to other teeth or distant locations in the maxillofacial area or the neck, making the diagnosis challenging.2
Dental pathologies can favor the spread of infection to the maxillary sinus due to the proximity of the root apexes to the maxillary sinus floor, leading to the development of sinus pathologies such as odontogenic maxillary sinusitis (OMS).3 - 6
OMS is secondary to an adjacent infectious maxillary dental pathology or complications from dental procedures.7 It has a prevalence of 25% to 40%,7 - 10 with studies reporting a higher rate of 86%.3 The clinical presentations of rhinosinusitis can overshadow odontogenic sources, and dental symptoms can overshadow sinusitis.7
OMS is a condition still underestimated and underdiagnosed,7, 11 and its diagnosis often requires evaluation by otolaryngologists and dentists.7 This report aims to present and describe two cases of OMS in which the dental source was correctly identified, and the pathology was managed by nonsurgical endodontic treatment and retreatment.
�
Case reports
Case 1
A 52-year-old female patient complained of a sharp and stabbing pain in her left cheek. It had started one year earlier, lasting a few minutes, and then worsened to persistente pain. A neurologist diagnosed her with trigeminal neuralgia and prescribed carbamazepine 400 mg BID, but she did not respond to this treatment. She underwent another medical consultation, which ruled out the trigeminal neuralgia diagnosis and suggested an evaluation with a dentist specialized in orofacial pain for a possible diagnosis of odontalgia.
During the consultation with the dentist, the patient presented with pain to palpation and percussion, and tooth #27 was negative for the cold pulp test, suggesting pulp alteration.
A computed tomography scan of the maxillary sinuses showed tooth #27 with delimited apical hypodensity and thickening of the left maxillary sinus membrane (Figure 1), compatible with an inflammatory lesion.
�

Figure 1. Initial computed tomography image of th left maxillary region showing apical periodontitis associated with tooth #27 and mucosal thickening in the maxillary sinus.
�
The patient was referred to an endodontist for nonsurgical root canal treatment (Figure 2). Tooth #27 was anesthetized with submucosal infiltration using 1.8 mL of 2.0% mepivacaine with 1:100,000 epinephrine (DFL, Rio de Janeiro, Brazil), and rubber dam isolation was established. The access cavity was made using 1014 and 3080 diamond burs (KG Sorensen, Cotia, Brazil), and the root canals were identified with the aid of an endodontic explorer. The working length was determined with an electronic apex locator (Root Zx II, Morita, USA). The mesiobuccal and distobuccal root canals were prepared with a #35.04 Mtwo file (VDW Dental, Munich, Germany), and the palatal root canal up to a #50.05 Reciproc file (VDW Dental, Munich, Germany) at 350 rpm of speed and 3 N of torque. All instrumentation was performed under copious syringe irrigation with 2 mL of 2.5% sodium hypochlorite per canal after using each instrument.
�

Figure 2. Initial periapical radiography of tooth #27.
�
The final rinse consisted of irrigation with 2 mL of 17.0% EDTA per canal, which remained for three minutes, followed by a final sodium hypochlorite rinse with 5 mL of solution per canal. The root canals were dried using matched paper points #30 (VDW Dental, Munich, Germany).
Then, an intracanal dressing with calcium hydroxide paste (UltraCal XS, Ultradent, USA) was applied, and a glass-ionomer cement (Ionofast, Biodinâmica, Brazil) was used for a provisional restoration.
In the second appointment, the intracanal dressing was removed using a #20 manual file up to the working length, and final irrigation was performed with 17.0% EDTA and 2.5% sodium hypochlorite, following the same protocol as the first appointment.
The canals were dried with paper points. Then, root canal filling was performed with gutta-percha cones (Odous de Deus, Belo Horizonte, Brazil) calibrated according to the tip of the last instrument used, using the single-cone technique and the BioRootTM RCS sealer (Septodont, Saint-Maur-des-Fossés, France) (Figure 3). The access cavity was temporarily restored with glass-ionomer cement, and the patient was referred for coronal rehabilitation.
�

Figure 3. Final periapical radiography of tooth #27.
�
After the endodontic treatment, the patient became completely asymptomatic. A 5-month cone-beam computed tomography (CBCT) scan showed the absence of maxillary sinus abnormalities (Figure 4). Another CBCT scan two years later confirmed it (Figure 5).
�

Figure 4. 5-month follow-up CBCT image of tooth #27 showing signs of repair of the apical periodontitis and maxillary sinus abnormalities.
�
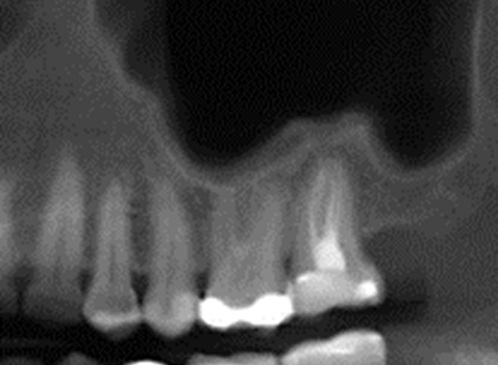
Figure 5. 2-year follow-up CBCT image of tooth #27 showing absence of apical periodontitis related to tooth #27 and maxillary sinus abnormalities.
�
Case 2
A 42-year-old female patient had a chief complaint of mild facial sensitivity in the left maxillary posterior region. On clinical examination, the patient presented with only slight discomfort in the molar teeth region during percussion, but teeth #23 and #27 were positive for the cold pulp test. Two months before, she had undergone endodontic treatment on tooth #26 due to irreversible pulpitis (Figure 6). The initial periapical radiography showed no changes in the premolars or molars (Figure 6), so a CBCT was requested. The CBCT revealed apical periodontitis in tooth #25, which had undergone previous endodontic treatment (Figure 7). It also showed thickening of the left maxillary sinus membrane and destruction of cortical bone (Figures 7 and 8). Thus, it was decided to perform nonsurgical endodontic retreatment.
�

Figure 6. Initial periapical radiography of the maxillary left premolars and molars.
�

Figure 7. Initial CBCT image (sagittal view) showing cortical bone destruction and mucosal thickening associated with tooth #25.
�

Figure 8. Initial CBCT image (axial view) showing mucosal thickening associated with tooth #25.
�
The access cavity was obtained with a round high-speed diamond bur (1014, KG Sorensen, Cotia, Brazil) under suitable anesthesia and rubber dam isolation. After locating the root canals, the filling material was removed using a #25 Reciproc Classic file (VDW Dental, Munich, Germany) without solvent. The working length was determined with an electronic apex locator (Root Zx II, Morita, USA). The root canals were instrumented with a #35.04 Mtwo file (VDW Dental, Munich, Germany), and the palatal root canal up to a #50.05 Reciproc Blue file (VDW Dental, Munich, Germany).
All instrumentation was performed under copious syringe irrigation with 2.5% sodium hypochlorite. The final rinse consisted of irrigation with 2 mL of 17.0% EDTA per canal, which remained for three minutes, followed by a final sodium hypochlorite rinse with 5 mL of solution per canal. The root canals were dried using matched paper points #30 (VDW Dental, Munich, Germany). Then, an intracanal dressing with calcium hydroxide paste (UltraCal XS, Ultradent, USA) was applied, and a glass-ionomer cement (Ionofast, Biodinâmica, Brazil) was used for a provisional restoration.
In the second appointment, the intracanal dressing was removed using a #20 manual file up to the working length, and final irrigation was performed with 17.0% EDTA and 2.5% sodium hypochlorite, following the same protocol as the first appointment.
The canals were dried with paper points. Then, root canal filling was performed with gutta-percha cones (Odous de Deus, Belo Horizonte, Brazil) calibrated according to the tip of
the last instrument used, using the single-cone technique and the BioRootTM RCS sealer (Septodont, Saint-Maur-des-Fossés, France) (Figure 9). The access cavity was temporarily restored, and the patient was referred for coronal rehabilitation.
�

Figure 9. Final periapical radiography of tooth #25.
�
The symptoms showed improvement after the first appointment, in which the filling material was removed and the root canals were disinfected and filled with the intracanal dressing. They completely disappeared after 15 days of treatment. After 16 months, a CBCT scan showed signs of normality (Figures 10 and 11).
�

Figure 10. 16-month follow-up CBCT image (sagital view) of tooth #25 showing cortical bone repair and absence of maxillary sinus abnormalities.
�
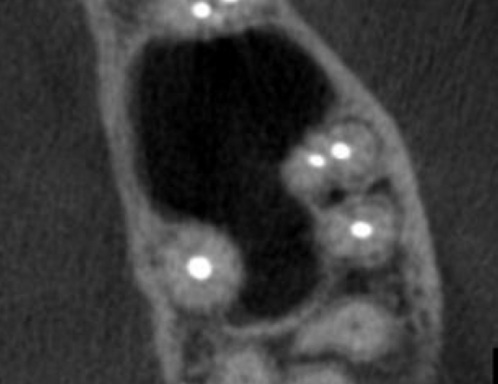
Figure 11. 16-month follow-up CBCT image (axial view) of tooth #25 showing no maxillary sinus abnormalities.
�
Discussion and conclusions
A pulpal infectious process in maxillary posterior teeth can affect the integrity of the maxillary sinus floor and lead to inflammatory changes in the sinus mucosa, such as its thickening.6, 12 The maxillary sinus mucosa can be considered normal when there is no thickening or a uniform thickening of up to 2 mm, 11 - 13 or up to 3 mm.14
Teeth-related mucosal thickening in the sinus was observed in both reported cases. This sign is the most common abnormality of the maxillary sinus, with a prevalence ranging from 36% to 58.5%.3, 4, 9, 11, 14 Special attention must be given to the involvement of one or both sinuses, as unilateral involvement is considered a sign to investigate dental etiology.15 Also, mucosal thickening is ten times more common in individuals with apical periodontitis,15 reaching a prevalence of 70% in those with mild and moderate apical periodontitis and 100% in those with severe apical periodontitis.3
In the first case reported, the sinus pathology was related to the second molar, which had its roots located below the maxillary sinus floor. This finding agrees with a previous study that reported that the mesiobuccal root is the closest to the sinus floor16 In the second case reported, the affected tooth was the second premolar, which, compared to the first premolar, is closer to the maxillary sinus floor,16, 17 and is usually located below it.15, 16
However, studies evaluating the relationship between the sinus mucosal thickening and the anatomical relationship of the root apexes reported that the proximity of the root apex
to the floor of the maxillary sinus alone did not influence the development of mucosal thickening,3, 11 only when associated with other factors, such as the presence of apical periodontitis.3, 11 Likewise, one study indicated that the presence of endodontic treatment alone did not increase the degree of mucosal thickening.11 Adequate length, homogeneity of the filling, and coronal sealing have been related to the absence of sinus abnormalities (63.98%, 74.19%, and 89.78% of cases, respectively) and higher rates of an absence of periapical lesions (68.71%, 78.7 8%, and 89.93% of cases, respectively).4
The clinical symptoms of OMS alone are not sufficient for its diagnosis since this condition may be asymptomatic.7 In both reported cases, the patients only reported pain or discomfort in the maxillary area. However, common symptoms ofOMS are foul smell, purulence, and dental pain.7
Imaging exams are important tools for diagnosing OMS. Panoramic radiographs are limited due to the overlap of anatomical structures and the impossibility of cross-sectional analysis. In turn, CBCT provides three-dimensional images, showing the size and location of periapical lesions and the proximity of root apices to other structures.3, 5, 12, 13 A study comparing these two types of imaging exams reported that panoramic radiography provided smaller distances and a greater relationship of apices within the maxillary sinus.13 In our second case, apical periodontitis or sinus abnormalities were not observed in the initial periapical radiography, but the CBCT showed changes in the maxillary sinus and its association with the affected teeth. Periapical radiographs can provide high-quality images but have the same limitation as panoramic radiographs: the superimposition of anatomical structures.15
The treatment for OMS typically includes nonsurgical root canal treatment, periradicular surgery, or even tooth extraction.6 In both reported cases, nonsurgical root canal treatment
or retreatment was the choice, and no antibiotics were required. For the successful management of OMS, the primary goal is to control the root canal infection rather than using
systemic antibiotics, as these will not treat the cause of the pathology.6
The cases reported demonstrate the importance of a correct diagnosis to provide the best management for the patient and avoid unnecessary interventions. It often requires a multidisciplinar approach involving otorhinolaryngologists and diverse specialties within dentistry.7, 10, 11 The cold pulp test and the CBCT scan are important to help in the differential diagnosis.6, 7, 15 When there is an endodontic origin, the tooth must have a necrotic pulp or a failing root canal treatment.6
Dental pathologies of endodontic origin may spread infections to the maxillary sinus. Clinicians must be knowledgeable about OMS and be able to determine whether the symptoms
reported by the patient have a truly odontogenic origin. It is important to incorporate CBCT images into the diagnostic process to determine if there is a relationship between the dental source and maxillary sinus abnormalities.
�
References
1. International Classification of Orofacial Pain, 1st Editions (ICOP). Cephalalgia. 2020;40:129-221.
2. De Leeuw R, Klasser GD, editors. Orofacial pain: guidelines for assessment, diagnosis, and management. 6th ed. Hanover Park, IL: Quintessence Publishing Co, Inc; 2018.
3. Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012;38:1069-74.
4. Souza-Nunes LA, Verner FS, Rosado LPL, Aquino SN, Carvalho ACP, Junqueira RB. Periapical and Endodontic Status Scale for Endodontically Treated Teeth and Their Association with Maxillary Sinus Abnormalities: A Cone-beam Computed Tomographic Study. J Endod. 2019;45:1479-88.
5. Rodrigues PA, Pinheiro VV, Moura JDM, Silva DCB, Tuji FM. Anatomical proximity of upper teeth and local factos associated with the thickness of the maxillary sinus membrane: a retrospective study. Giornale Italiano di Endodonzia. 2021;35:44-51.
6. Siqueira JF, Jr., Lenzi R, Hern�ndez S, Alberdi JC, Martin G, Pessotti VP, et al. Effects of Endodontic Infections on the Maxillary Sinus: A Case Series of Treatment Outcome. J Endod. 2021;47:1166-76.
7. Craig JR, Poetker DM, Aksoy U, Allevi F, Biglioli F, Cha BY, et al. Diagnosing odontogenic sinusitis: An international multidisciplinary consensus statement. Int Forum Allergy Rhinol. 2021;11:1235-48.
8. Sakir M, Ercalik Yalcinkaya S. Associations between Periapical Health of Maxillary Molars and Mucosal Thickening of Maxillary Sinuses in Cone-beam Computed Tomographic Images: A Retrospective Study. J Endod. 2020;46:397-403.
9. Garcia-Font M, Abella F, Patel S, Rodr�guez M, Sanchez JAG, Duran-Sindreu F. Cone-beam Computed Tomographic Analysis to Detect the Association between Primary and Secondary Endodontic Infections and Mucosal Thickness of Maxillary Sinus. J Endod. 2020;46:1235-40.
10. Ito K, Kondo T, Andreu-Arasa VC, Li B, Hirahara N, Muraoka H, et al. Quantitative assessment of the maxillary sinusitis using computed tomography texture analysis: odontogenic vs non-odontogenic etiology. Oral Radiol. 2022;38:315-24.
11. Aksoy U, Orhan K. Association between odontogenic conditions and maxillary sinus mucosal thickening: a retrospective CBCT study. Clin Oral Investig. 2019;23:123-31.
12. Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod. 2011;37:753-7.
13. Terlemez A, Tassoker M, Kizilcakaya M, Gulec M. Comparison of cone-beam computed tomography and panoramic radiography in the evaluation of maxillary sinus pathology related to maxillary posterior teeth: Do apical lesions increase the risk of maxillary sinus pathology? Imaging Sci Dent. 2019;49:115-22.
14. Nunes CA, Guedes OA, Alencar AH, Peters OA, Estrela CR, Estrela C. Evaluation of Periapical Lesions and Their Association with Maxillary Sinus Abnormalities on Conebeam Computed Tomographic Images. J Endod. 2016;42:42-6.
15. Whyte A, Boeddinghaus R. Imaging of odontogenic sinusitis. Clinical Radiology. 2019;74:503-16.
16. Tian XM, Qian L, Xin XZ, Wei B, Gong Y. An Analysis of the Proximity of Maxillary Posterior Teeth to the Maxillary Sinus Using Cone-beam Computed Tomography. J Endod. 2016;42:371-7.
17. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. An Assessment of the Relationship between the Maxillary Sinus Floor and the Maxillary Posterior Teeth Root Tips Using Dental Cone-beam Computerized Tomography. Eur J Dent. 2010;4:462-7.
�
Lisa Yurie Oda
E-mail address: yu_oda@hotmail.com
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Andr� Luiz da Costa Michelotto: Conceptualization, Data curation; Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation,
Visualization, Writing � review & editing. Lisa Yurie Oda: Data curation, Formal analysis, Investigation, Methodology, Writing � original draft, Writing � review & editing. Wagner Hummig: Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing � review & editing. Antonio Batista: Conceptualization, Project administration, Resources, Supervision, Validation, Visualization, Writing � review & editing.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
