
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 51-57
Original research
Factors associated with the prevalence of apical periodontitis: An observational study
Fatores associados à prevalência de pediodontite apical: um estudo observacional
a Universidade Católica Portuguesa, Faculty of Dental Medicine, Center for Interdisciplinary Research in Health, Viseu, Portugal
b Department of Endodontics, Rey Juan Carlos University, Madrid, Spain
Rita Noites - rita.noites@ucp.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Original research
Pages - 51-57
Go to Volume
Article History
Received on 29/07/2024
Accepted on 11/05/2025
Available Online on 11/06/2025
Keywords
Original Research
Factors associated with the prevalence of apical periodontitis: An observational study
Fatores associados à prevalência de pediodontite apical: um estudo observacional
Rita Noites1,* 0009-0008-2329-5071
Maria Bartolomeu1 0000-0003-2986-2088
Ana Sofia Duarte1 0000-0001-6849-6004
Alejandro Perez2 0000-0002-6925-5939
Miguel Cardoso1 0000-0003-2916-0537
1Universidade Católica Portuguesa, Faculty of Dental Medicine, Center for Interdisciplinary Research in Health, Viseu, Portugal
2Department of Endodontics, Rey Juan Carlos University, Madrid, Spain
Article history:
Received 29 July 2024
Accepted 11 May 2025
Available online 9 June 2025
Abstract
Objectives: Apical periodontitis is a lesion of endodontic origin caused by an immune response to necrotic and infected dental pulp. Since apical periodontitis can persist after endodontic treatment, radiographic diagnosis is crucial. This study evaluates factors associated with the prevalence of apical periodontitis in a Portuguese population using the full-scale periapical index.
Methods: A cross-sectional study analyzed 402 medical records and panoramic radiographs from January to May 2023. The periapical status, presence of apical periodontitis, quality of endodontic treatment, quality of coronal restoration, presence of caries lesions, and presence of retained root fragments were assessed. The correlation between these variables was examined.
Results: Among 9056 teeth, 4.7% presented apical periodontitis (periapical index ≥3), and 53.3% of participants had fewer than one apical periodontitis lesion. Of 437 teeth with endodontic treatment, 300 (69.6%) did not have apical periodontitis, while 131 (30.4%) had apical periodontitis. A significant statistical relationship (p<0.05) was observed between apical periodontitis and other dental conditions, including the presence of retained root fragments, caries lesions, the quality of endodontic treatment, and the quality of restoration. The strongest correlation was found between apical periodontitis and the quality of endodontic treatment (Cramers V = 61%), while no consistent correlations were observed with other variables.
Conclusions: The prevalence of apical periodontitis was higher in teeth with endodontic treatment, with a strong correlation with treatment quality. The presence of caries lesions, coronal restorations, and retained root fragments also influenced the occurrence of apical periodontitis, reinforcing the need for further studies.
Keywords: Dental restoration,Endodontically treated teeth,Periapical diseases,Periapical periodontitis,Treatment outcome
Resumo
Objectivos: A periodontite apical é uma lesão de origem endodôntica causada pela resposta imunológica à polpa dentária necrótica e infetada. Como pode persistir após o tratamento endodôntico, o diagnóstico radiográfico é essencial. Este estudo avalia os fatores associados à sua prevalência numa população portuguesa, utilizando o índice periapical.
Métodos: Estudo transversal com a análise de 402 registos clínicos e radiografias panorâmicas entre janeiro e maio de 2023. Avaliaram-se o estado periapical, a presença de periodontite apical, a qualidade do tratamento endodôntico e da restauração coronária, lesões de cárie e fragmentos radiculares retidos. Foram analisadas correlações entre estas variáveis.
Resultados: De entre 9056 dentes analisados, 4,7% apresentavam periodontite apical (índice periapical ≥ 3) e 53,3% dos participantes tinham menos de uma lesão de periodontite apical. Dos 437 dentes tratados endodonticamente, 300 (69,6%) não apresentavam periodontite apical, enquanto 131 (30,4%) apresentavam. Foi observada uma
correlação estatisticamente significativa (p<0,05) entre periodontite apical e fatores como fragmentos radiculares retidos, lesões de cárie, qualidade do tratamento endodôntico e qualidade da restauração. A correlação mais forte foi encontrada entre periodontite apical e qualidade do tratamento endodôntico (V de Cramer = 61%), não tendo sido observadas correlações consistentes com outras variáveis.
Conclusões: A prevalência de periodontite apical foi maior em dentes com tratamento endodôntico, correlacionando-se fortemente com a sua qualidade. Lesões de cárie, restaurações coronárias e fragmentos radiculares retidos também influenciaram a ocorrência de periodontite apical, reforçando a necessidade de estudos adicionais.
Palavras-chave: Restauração dentária,Dentes tratados endodonticamente, Doença periapical, Periodontite periapical, Resultado do tratamento
Introduction
Apical periodontitis (AP) is an endodontic condition caused by the infection and necrosis of pulp tissue.1, 2 It presents as a defensive response to microorganisms in the root canal system.3 This inflammation results from a dynamic interplay between microbial factors in the root canals and the hosts defense mechanisms at the interface between the infected pulp and the apical tissues.4
Longitudinal studies of endodontic treatment performed in postgraduate programs or by specialists have reported high success rates of approximately 7580% in teeth with AP after4 5 years of follow-up. 5 7 However, cross-sectional studies from various countries reveal a relatively high prevalence of AP in root-treated teeth, ranging from 32% to 68%.8 12 The high prevalence of chronic AP has been recognized as a significant public health concern in some regions. Consequently, numerous cross-sectional studies have been conducted to assess the prevalence of AP and identify factors influencing the outcomes of endodontic treatment.13 15
Data on the prevalence of AP across different countries show variability in outcomes. While root canal treatments for teeth with AP generally achieve relatively high success rates, the importance of failure cases cannot be overlooked. Understanding the variables that impact treatment prognosis is critical for developing strategies to enhance outcomes and improve long-term success rates.
A systematic review of cross-sectional studies on the prevalence of AP found that 36% of root canal-treated teeth exhibited signs of AP.16 Furthermore, radiographic analysis revealed that most root canal treatments in that study were of poor or unacceptable technical quality.16 Up to 78% of these treatments were classified as inadequate, with only a smaller proportion classified as acceptable.16 Similarly, a recente meta-analysis reported that AP prevalence in root-filled teeth ranged from 5% to 74%.17 These figures underscore the need for policymakers to monitor public dental health demographics, compare them with other communities, and identify the strengths and weaknesses of oral and dental health programs.
This epidemiological study aimed to characterize, describe, and evaluate the prevalence of periapical radiolucency and nonsurgical root canal treatments in the Portuguese population served by an undergraduate program at a University Clinic.
Material and methods
The target population consisted of patients from the Universidade Católica Portuguesa Dental Clinic in Viseu. The patients were selected according to initial diagnostic visits from September 2023 to December 2023.
A total of 402 clinical records with panoramic radiographs were reviewed, and relevant medical and dental history data were collected using the NewSoft DS® program (ImaginaSoft HS©), which is used by the University in clinical appointments.
The final sample was established based on the following inclusion criteria: patients of both sexes, aged 18 years or older, with a minimum of eight teeth in the mouth. The exclusion criteria were patients without panoramic radiographs in their clinical records and/or incomplete clinical records; patients aged less than 18 years old and with fewer than eight teeth in the mouth; and analysis of third molars and dental implants.
A calibration method was previously developed to enhance the reliability of the results in panoramic radiograph reviews.
Two observers, one of whom had advanced clinical experience, received 100 random periapical radiographs, instructions and rules for calibration, and a document to register the scores attributed to each radiograph. The observers determined whether endodontic treatment (ET) and coronal restorations were adequate or inadequate by evaluating each radiograph using the periapical index (PAI) scoring system developed by Ørstavik et al.,18 according to a nominal scale from 1 to 5 points, where: 1 and 2 mean success; 3, 4, and 5 indicate the presence of AP. The calibration obtained a Kappa value of 0.83 (>0.61), confirming the methods suitability. Then, the periapical status of all the teeth in the study was evaluated using respective panoramic radiographs.
The chosen variables were associated with the patients identification, individual tooth condition, and oral cavity condition. The patients identification variables included clinic number, age, and sex. The variables related to the individual tooth condition included the presence of retained root fragments, the presence of cavities, the presence and quality of the ET, and the presence and quality of the restoration. The variables associated with the oral cavity condition included the number of retained root fragments, teeth with AP, ETs, restorations, and cavities.
The statistical analysis was made with the IBM SPSS software, version 21.0 (IBM Corporation, New York, USA). Regarding sample characterization, the variables were analyzed using relative and absolute frequencies. All tests used a significance level of 5% (α = 0.05). The chi-square test of Independence was used to assess the relationship between two qualitative variables. In the correlations where the chisquare test was not applicable, the variables were grouped into classes to perform the statistical test. The Cramers V coefficient was calculated (limited to values between 0 and 1) to evaluate the strength of associations between variables.
In the analysis of quantitative variables, the normality of the data was assessed using the Kolmogorov-Smirnov test. The Mann-Whitney and Kruskal-Wallis non-parametric tests were used when suited.
Results
The study analyzed 402 patients, comprising 230 females (57.2%) and 172 males (42.8%), with a mean age of 46.8 ± 17.6 years (Table 1). A total of 9056 teeth were evaluated (Table 2).
Table 1. Descriptive statistics for the variables age, number of retained root fragments, number of caries lesions, and number of teeth missing.
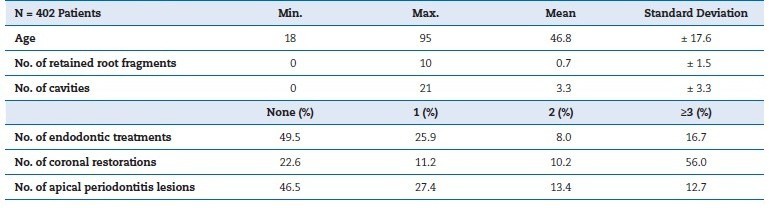
Table 2. Descriptive statistics for the variables endodontic treatment, coronal restorations, and periapical index (PAI) score.
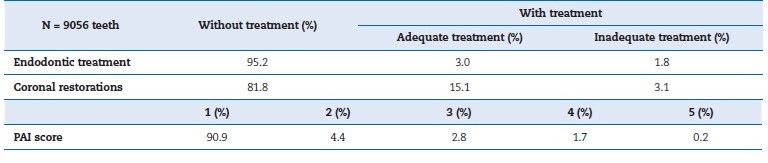
Concerning ET, 199 patients (49.5%) had no ET, representing 8625 teeth (95.2%), while 104 patients (25.9%) had one ET, 32 (8.0%) had two ETs, and 67 (16.7) had three or more ETs, collectively accounting for 431 endodontically treated teeth (4.8%) (Table 1. Among these, ET was classified as adequate in 270 teeth (62.6%) and inadequate in 161 (37.4%).
Regarding coronal restoration, 91 patients (22.6%) had no restorations, 45 (11.2%) had one, 41 (10.2%) had two, and 225 (56.0%) had three or more (Table 1). In total, 7409 teeth (81.8%) had no coronal restorations, while 1647 teeth (18.2%) were restored (Table 2). Among these restored teeth, 1367 (83%) had well-adapted restorations, while 280 (17%) had poorly adapted ones.
Analysis of AP showed that 187 patients (46.5%) had no AP lesions, while 110 (27.4%) had one, 54 (13.4%) had two, and 51 (12.7%) had three or more (Table 1). At least one AP lesion was identified in 53.5% of the patients. When evaluating PAI values for all teeth, the most prevalent score was PAI 1 (90.9%, 8232 teeth), followed by PAI 2 (4.4%, 397 teeth), PAI 3 (2.8%, 255 teeth), PAI 4 (1.7%, 153 teeth), and PAI 5 (0.2%, 18 teeth) (Table 2). The mean number of caries lesions was 3.3 ± 3.3, and the mean number of retained root fragments was 0.7 ± 1.5.
Out of the 431 teeth endodontically treated, 300 (69.6%) had no AP, while 131 (30.4%) had AP (PAI ≥ 3). Among the 300 teeth without AP, 246 (57.1%) had adequate ET, and 54 (12.5%) had inadequate ET. Conversely, of the 131 teeth with AP, 24 (5.6%) had adequate ET, and 107 (24.8%) had inadequate ET. Thus,
81.7% of teeth with AP and ET were associated with inadequate ET (Table 3). Statistical analysis revealed a significant relationship between the presence of AP and ET (p < 0.05, p = 0), with a moderately low correlation strength (Cramers V = 0.21). Furthermore, the presence of AP and the quality of ET were significantly
related (p < 0.05, p = 0), with a strong correlation (Cramers V = 0.61) (Figure 1).
Table 3. Descriptive statistics between periapical index (PAI) score and endodontic treatment.
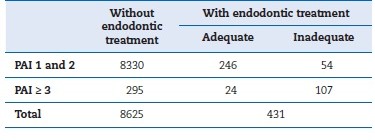
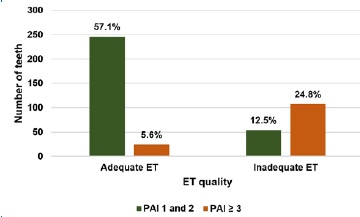
Figure 1. Correlation between periapical index (PAI) score and endodontic treatment quality.
Of the 1647 teeth with coronal restorations, 1506 (91.4%) were free of AP, while 141 (8.6%) exhibited AP. For teeth with PAI scores of 1 or 2, 1277 (77.5%) had well-adapted restorations, and 229 (13.9%) had poorly adapted restorations. Among teeth with PAI ≥ 3, 90 (5.5%) had well-adapted restorations, and 51 (3.1%) had poorly adapted restorations (Table 4). Overall, 141 teeth with AP had coronal restorations, of which 36.2% were poorly adapted. Statistical analysis demonstrated a significant relationship between the presence of AP and coronal restorations (p < 0.05, p = 0) but with low correlation strength (Cramers V = 0.09). The relationship between PAI and restoration quality was also significant (p < 0.05, p = 0), with a moderately low correlation strength (Cramers V = 0.16) (Figure 2).
Table 4. Descriptive statistics between periapical index (PAI) score and coronal restoration.
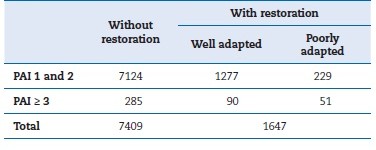
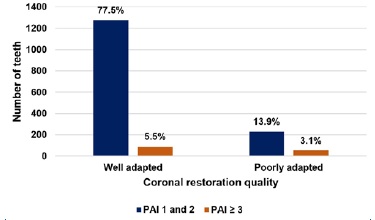
Figure 2. Correlation between periapical index (PAI) and coronal restoration quality.
Of the 9056 teeth evaluated, 278 (3.1%) presented retained root fragments, of which 172 (61.9%) were associated with AP (PAI ≥ 3). Among the 426 teeth with AP, 40.4% had retained root fragments. The relationship between PAI and retained root fragments was significant (p < 0.05, p = 0), with a moderate correlation strength (Cramers V = 0.48) (Table 5).
Table 5. Descriptive statistics between periapical index (PAI) score and retained root fragments and caries lesions.
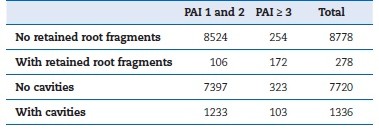
A total of 1336 teeth had caries lesions, of which 103 (7.7%) were associated with AP (PAI ≥ 3). Among the 426 teeth with AP, 24.2% exhibited cavities. The relationship between PAI and the presence of cavities was significant (p < 0.05, p = 0), although with a weak correlation (Cramers V = 0.06) (Table 5).
Discussion
The findings of this study demonstrate a significant association between the PAI and ET. Specifically, 1.5% of teeth exhibited apical lesions despite having undergone ET, with 18.3% of these cases involving adequate treatment and 81.7% inadequate treatment. These results are slightly higher than those reported in other national and international studies, which have also observed apical lesions in treated teeth despite diferences in methodology and populations studied.19 24 For example, in Greece, 60% of teeth with inadequate ET were associated with apical lesions.25 Variations in these findings may result from differences in healthcare systems, participant demographics, and the non-representative nature of some study populations.
Recent studies provide additional context to the findings of this research. A cross-sectional study using cone-beam computed tomography (CBCT) in Portuguese patients investigated the prevalence of lateral radiolucency, apical root resorption, and periapical lesions and found significant associations between these pathologies and the quality of ET, emphasizing the diagnostic precision offered by CBCT.26 Similarly, another study examining the prevalence of AP and its relationship with prior root canal treatment, the length of root canal filling, and the type of coronal restoration concluded that inadequate root canal filling and poorly adapted coronal restorations were strongly linked to higher rates of AP, supporting the findings of our study.27
In Sweden, a study evaluating 200 teeth with ET revealed the persistence of Gram-positive bacteria within root canals in cases of both chronic and acute periodontitis despite treatment and antimicrobial interventions.28 These findings underscore the challenges in completely eradicating bacterial biofilms from root canals, even with modern endodontic techniques. Contemporary endodontics emphasizes the importance of efficient biomechanical preparation and thorough disinfection of root canals to minimize bacterial biofilm and improve treatment outcomes. 29 31
Beyond ET, this study identified additional factors associated with AP, including the quality of coronal restorations, the presence of retained root fragments, and the presence of cavities.
Among the 141 teeth with AP and coronal restoration, 36.2% had poorly adapted coronal restoration. Furthermore, of the 426 teeth with AP, 40.4% contained retained root fragments, and 24.2% exhibited cavities. Poorly adapted coronal restorations were defined as those with excess or insuficiente restorative material, fractures, or visible radiolucent gaps between the restoration and the tooth. Fixed prostheses were also included in the definition of restorations. These findings align with a previous study, whic h identified similar risk factos for AP, including poorly adapted restorations and cavities.32 Other studies have also reported higher prevalence rates of AP in teeth with inadequate restorative treatment.32, 33
The sample size of 9056 teeth in this study is comparable to that of other investigations in the field. A notable predominance of female participants was observed, consistent with other epidemiological studies on endodontics. The mean participant age of 46.8 ± 17.6 years aligns with findings from studies conducted in other European countries.34, 35 Sociological factors may explain differences in sex distribution and age across studies. Patients with fewer than eight teeth were excluded to minimize confounding effects from established periodontal disease, which could complicate the assessment of other factors associated with AP.21, 35, 36
AP prevalence in this study revealed that at least one lesion was present in 53.5% of the participants. Studies using panoramic radiographs for AP evaluation report lower prevalence rates, ranging from 34% to 45%.23, 34, 36 Conversely, investigations employing periapical radiographs typically report higher prevalence rates of 70% to 86%.24, 25, 37 These discrepancies may result from differences in sample selection, radiographic methods, and diagnostic criteria for AP. In this study, 4.7% of teeth presented with AP lesions, a value within the range ofprevious studies conducted in various countries (2.9% to 8.4%).19, 23, 24, 34, 35, 38, 39
The choice of panoramic radiography as the primary diagnostic tool was dictated by its availability across all clinical records reviewed. While panoramic radiographs offer comprehensive coverage and lower radiation exposure than a fullmouth series of intraoral radiographs, they have limitations in resolution and diagnostic precision for detecting subtle lesions.
For more detailed assessments, complementary techniques such as intraoral radiographs or CBCT are recommended.40, 41 Despite its limitations, panoramic radiography remains a practical tool for large-scale epidemiological studies due to its efficiency and patient comfort.
The PAI system developed by Ørstavik et al.18 was chosen to evaluate AP lesions in this study because of its widespread use and reliability in assessing the severity of periapical pathology.
This methodology has been employed in similar studies to standardize evaluations and facilitate comparisons across research.19, 23, 24
Finally, while this study analyzed individual variables such as AP prevalence and ET adequacy, other potential risk factos were not excluded from consideration. Although inadequate ET was strongly associated with AP, the influence of additional variables cannot be ruled out. These findings highlight the multifactorial nature of AP and underscore the need for further studies to identify and control all contributing factors.
References
1. Kakehashi S, Stanley HR, Fitzgerald RJ. The effects of surgical exposures of dental pulps in germ-free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol. 1965;20:3409.
2. Siqueira JF, Rôças IN, Ricucci D. Biofilms in endodontic infection. Endodontic Topics. 2012;22:3349.
3. Ricucci D, Siqueira Jr JF. Biofilms and Apical Periodontitis: Study of Prevalence and Association with Clinical and Histopathologic Findings. J Endod. 2010;36:127788. rev port estomatol med dent cir maxilofac . 2025;66(2) :51-57 55
4. Nair PNR. Pathogenesis of Apical Periodontitis and the Causes of Endodontic Failures. Crit Rev Oral Biol Med. 2004;15:34881.
5. Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44:583609.
6. Ricucci D, Russo J, Rutberg M, Burleson JA, Spångberg LSW. A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:82542.
7. Hoskinson SE, Ng YL, Hoskinson AE, Moles DR, Gulabivala K. A retrospective comparison of outcome of root canal treatment using two different protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:70515.
8. Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995;28:1218.
9. Moreno JO, Alves FRF, Gonçalves LS, Martinez AM, Rôças IN, Siqueira JF. Periradicular Status and Quality of Root Canal Fillings and Coronal Restorations in an Urban Colombian Population. J Endod. 2013;39:6004.
10. Tavares PBL, Bonte E, Boukpessi T, Siqueira JF, Lasfargues JJ. Prevalence of Apical Periodontitis in Root CanalTreated Teeth From an Urban French Population: Influence of the Quality of Root Canal Fillings and Coronal Restorations. J Endod. 2009;35:8103.
11. Gündüz K, Avsever H, Orhan K, Demirkaya K. Cross-sectional evaluation of the periapical status as related to quality of root canal fillings and coronal restorations in a rural adult male population of Turkey. BMC Oral Health. 2011;11:20.
12. Hommez GMG, Coppens CR, De Moor RJ. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002;35:6809.
13. Tronstad L, Asbjørnsen K, Døving L, Pedersen I, Eriksen HM. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol. 2000;16:21821.
14. Segura-Egea JJ, Jiménez-Pinzón A, Poyato-Ferrera M, Velasco-Ortega E, Ríos-Santos J V. Periapical status and quality of root fillings and coronal restorations in an adult Spanish population. Int Endod J. 2004;37:52530.
15. Kalender A, Orhan K, Aksoy U, Basmaci F, Er F, Alankus A. Influence of the Quality of Endodontic Treatment and Coronal Restorations on the Prevalence of Apical Periodontitis in a Turkish Cypriot Population. Med Princ Pract. 2013;22:1737.
16. Pak JG, Fayazi S, White SN. Prevalence of Periapical Radiolucency and Root Canal Treatment: A Systematic Review of Cross-sectional Studies. J Endod. 2012;38:11706.
17. Sadat Miri S, Khademi A, Amirkhani Z, Amiri SM, Goodarzi M, Khazaei S. Prevalence of Apical Periodontitis in Different Communities: A Meta-Analysis. Iran Endod J. 2018;13:43845.
18. Orstavik D, Kerekes K, Eriksen HM. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Endod Dent Traumatol. 1986;2:2034.
19. Kirkevang L, Hörsted-Bindslev P, Ørstavik D, Wenzel A. Frequency and distribution of endodontically treated teeth and apical periodontitis in an urban Danish population. Int Endod J. 2001;34:198205.
20. Kabak Y, Abbott P V. Prevalence of apical periodontitis and the quality of endodontic treatment in an adult Belarusian population. Int Endod J. 2005;38:23845.
21. Jiménez-Pinzón A, Segura-Egea JJ, Poyato-Ferrera M, Velasco- Ortega E, Ríos-Santos J V. Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int Endod J. 2004;37:16773.
22. Peters LB, Lindeboom JA, Elst ME, Wesselink PR. Prevalence of apical periodontitis relative to endodontic treatment in na adult Dutch population: a repeated cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:5238.
23. Marques MD, Moreira B, Eriksen HM. Prevalence of apical periodontitis and results of endodontic treatment in na adult, Portuguese population. Int Endod J. 1998;31:1615.
24. Sidaravicius B, Aleksejuniene J, Eriksen HM. Endodontic treatment and prevalence of apical periodontitis in an adult population of Vilnius, Lithuania. Endod Dent Traumatol. 1999;15:2105.
25. Georgopoulou MK, Spanaki-Voreadi AP, Pantazis N, Kontakiotis EG. Frequency and distribution of root filled teeth and apical periodontitis in a Greek population. Int Endod J. 2005;38:10511.
26. Meirinhos J, Martins J, Pereira B, Baruwa A, Ginjeira A. Prevalence of lateral radiolucency, apical root resorption and periapical lesions in Portuguese patients: a CBCT crosssectional study with a worldwide overview. Eur Endod J. 2021;6:5671.
27. Meirinhos J, Martins JNR, Pereira B, Baruwa A, Gouveia J, Quaresma SA, et al. Prevalence of apical periodontitis and its association with previous root canal treatment, root canal filling length and type of coronal restoration a crosssectional study. Int Endod J. 2020;53:57384.
28. de Paz LEC, Dahlén G, Molander A, Möller Å, Bergenholtz G. Bacteria recovered from teeth with apical periodontitis after antimicrobial endodontic treatment. Int Endod J. 2003;36:5008.
29. Estrela C, Alencar AHG, Dedurcio DA, Borges AH, Estrela CRA. Influência de estratégias de sanificação no sucesso do tratamento da periodontite apical. ROBRAC: Revista Odontologica do Brasil Central. 2012;21:367-75.
30. Estrela C, Leles CR, Hollanda ACB, Moura MS, Pécora JD. Prevalence and risk factors of apical periodontitis in endodontically treated teeth in a selected population of Brazilian adults. Braz Dent J. 2008;19:349.
31. Nair PNR. On the causes of persistent apical periodontitis: a review. Int Endod J. 2006;39:24981.
32. Kirkevang L, Wenzel A. Risk indicators for apical periodontitis. Community Dent Oral Epidemiol. 2003;31:5967.
33. Asgary S, Shadman B, Ghalamkarpour Z, Shahravan A, Ghoddusi J, Bagherpour A, et al. Periapical Status and Quality of Root canal Fillings and Coronal Restorations in Iranian Population. Iran Endod J. 2010;5:7482.
34. López-López J, Jané-Salas E, Estrugo-Devesa A, Castellanos-Cosano L, Martín-González J, Velasco-Ortega E, et al. Frequency and distribution of root-filled teeth and apical periodontitis in an adult population of Barcelona, Spain. Int Dent J. 2012;62:406.
35. Lupi-Pegurier L, Bertrand M-F, Muller-Bolla M, Rocca JP, Bolla M. Periapical status, prevalence and quality of endodontic treatment in an adult French population. Int Endod J. 2002;35:6907.
36. De Cleen MJH, Schuurs AHB, Wesselink PR, Wu MK. Periapical status and prevalence of endodontic treatment in an adult Dutch population. Int Endod J. 1993;26:1129.
37. Tsuneishi M, Yamamoto T, Yamanaka R, Tamaki N, Sakamoto T, Tsuji K, et al. Radiographic evaluation of periapical status and prevalence of endodontic treatment in an adult Japanese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:6315.
38. De Moor RJG, Hommez GMG, De Boever JG, Delmé KIM, Martens GEI. Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J. 2000;33:11320.
39. Dugas NN, Lawrence HP, Teplitsky PE, Pharoah MJ, Friedman S. Periapical health and treatment quality assessment of root-filled teeth in two Canadian populations. Int Endod J. 2003;36:18192.
40. Sanderink G, Gijbels F, Pauwels H, Jacobs R. Subjective image quality of digital panoramic radiographs displayed on monitor and printed on various hardcopy media. Clin Oral Investig. 2004;8:259.
41. Ridao-Sacie C, Segura-Egea JJ, Fernández-Palacín A, Bullón- Fernández P, Ríos-Santos J V. Radiological assessment of periapical status using the periapical index: comparison of periapical radiography and digital panoramic radiography. Int Endod J. 2007;40:43340.
Rita Noites
E-mail address: rita.noites@ucp.pt
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
CRediT authorship contribution statement
Rita Noites: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing original draft, Writing review & editing. Maria Bartolomeu: Data curation, Formal analysis, Investigation, Validation, Writing original draft, Writing review & editing. Ana Sofia Duarte: Formal analysis, Validation, Writing original draft, Writing review & editing. Alejandro Perez: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing original draft, Writing review & editing. Miguel Cardoso: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing original draft, Writing review & editing.
Acknowledgments
The authors thank the Foundation for Science and Technology (FCT, Portugal) for the financial support of the Center for Interdisciplinary Research in Health (CIIS) under the project UIDB/04279/2020 and UIDP/04279/2020.
1646-2890/© 2025 Sociedade Portuguesa de Estomatologia e Medicina Dentária. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
