
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (2) | 58-64
Original research
Intraoral stereoradiography visualization with virtual reality: peri-implant bone level estimation accuracy – An in vitro study
Estereoradiografia intraoral em realidade virtual: avaliação da precisão na medição do nível ósseo peri-implantar – Estudo in vitro
a Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b MEDISIS – Sistemas Médicos, Lda., Lisbon, Portugal
Jorge Ferreira da Costa - jfc@fmd.ulisboa.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 2
Original research
Pages - 58-64
Go to Volume
Article History
Received on 18/07/2024
Accepted on 24/04/2025
Available Online on 11/06/2025
Keywords
Original Research
�
Intraoral stereoradiography visualization with virtual reality: peri-implant bone level estimation accuracy � An in vitro study
Estereoradiografia intraoral em realidade virtual: avalia��o da precis�o na medi��o do n�vel �sseo peri-implantar � Estudo in vitro
�
�
Jorge Ferreira da Costa1,* 0000-0003-2830-6784
Jo�o Caram�s1 0000-0002-5544-3744
Daniel Hachmeister2 0000-0002-1420-4376
1Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal
2MEDISIS � Sistemas M�dicos, Lda., Lisbon, Portugal
�
Article history:
Received 18 July 2024
Accepted 24 April 2025
Available online 6 June 2025
�
Abstract
Objectives: The main objectives of this in vitro study were to evaluate the accuracy and precision of stereoradiography with virtual reality in measuring peri-implant bone level compared to conventional 2D radiography, and to find which stereoscopic angles between images lead to higher accuracy and precision. Another objective was to develop a virtual reality method for viewing pairs of stereoscopic radiographs, to archive, to present, and analyze the acquired stereoscopic images.
Methods: A blinded laboratory study compared 40 samples of randomly positioned implants in 10 artificial bone blocks simulating random bone defects and crestal angulations. 320 pairs of different stereoscopic angulation images were analyzed using a head-mounted display system. A total of 1280 measurements of the mesial, distal, buccal, and lingual margins were made, in a randomized order, using 0.4 mm cylindrical threads as reference, giving a 0.2 mm maximum precision in measurements.
Results: The median absolute error and relative error interquartile range were lower in stereoscopic images. The observers� error of bone height estimation reduced substantially when stereoscopic images were used, even at low angular disparities such as 2� of stereopsis. Observers reported viewing discomfort at angles above 6�.
Conclusions: Stereoradiography significantly reduced the error in bone height estimation, with any stereoscopic angle, compared to 2D. Augmented/virtual reality technology empowers stereoradiography, offering a more affordable and user-friendly imaging system.
Keywords: Dental implants,Depth perception,Head-mounted displays,Radiostereometric analysis
�
Resumo
Objetivos: Os objetivos principais deste estudo in vitro foram avaliar a exatid�o e precis�o da estereoradiografia com realidade virtual na medi��o do n�vel �sseo peri-implantar em compara��o com a radiografia convencional 2D, e definir que �ngulos estereosc�picos entre imagens fornecem informa��es mais exatas e precisas. Outro objetivo foi desenvolver um m�todo de visualiza��o de pares de radiografias estereosc�picas com realidade virtual, para arquivar, representar e analisar as imagens estereosc�picas adquiridas, em 3D.
M�todos: Um estudo laboratorial, cego, comparou 40 amostras de implantes posicionados aleatoriamente em 10 blocos de osso sint�tico, simulando defeitos �sseos aleat�rios. 320 pares de imagens com diferentes angula��es estereosc�picas foram observados atrav�s de um sistema de realidade virtual. Foram feitas um total de 1280 medi��es das margens mesial, distal, vestibular e lingual, randomizadas, usando espiras cil�ndricas de 0,4 mm como refer�ncia, conferindo uma precis�o m�xima de 0,2 mm na medi��o.
Resultados: As medianas dos erros absolutos e os intervalos interquartil dos erros relativos foram menores nas imagens estereosc�picas. Os observadores obtiveram uma redu��o substancial do erro na estimativa do n�vel �sseo sempre que eram utilizadas imagens estereosc�picas, mesmo com baixa disparidade angular tal como 2� de estereopsia. Os observadores relataram desconforto visual em �ngulos maiores que 8�.
Conclus�es: A estereoradiografia reduziu significativamente o erro na estimativa da altura �ssea, com qualquer �ngulo de estereopsia, em compara��o com 2D. A tecnologia de realidade aumentada/virtual favorece a estereoradiografia, oferecendo um sistema de imagem mais acess�vel e f�cil de usar.
Palavras-chave: Implantes dent�rios,Perce��o de profundidade,�culos inteligentes,An�lise radioestereom�trica
�
Introduction
Two-dimensional (2D) imaging modalities like panoramic and intraoral radiographs and three-dimensional (3D) modalities like multi-slice computed tomography (CT) and cone-beam computed tomography (CBCT) can be used to evaluate peri-implant bone level. CBCT has been shown to have higher accuracy and precision than intraoral radiography for evaluating intrabony defects, but it has limitations in terms of low sensitivity in detecting early bone changes, metal artifacts obscuring the bone margin, and high radiation dose.1 - 3 Ultrasound and dental magnetic resonance imaging have also been explored as alternatives to radiographs, since they effectively depict inflammation in mucositis and peri-implantitis,4 but further studies are needed to validate their use in implant bone margin assessment.5 - 7
Despite the availability of various advanced imaging techniques, intraoral radiography is still recommended as the modality of choice for measuring bone level around implants and monitoring stability over time.8 However, it is importante to notice the limitations of intraoral radiography, such as difficulty in evaluating the whole volume of bone around the implant�s neck, especially in the buccal and lingual sides, and the potential for measurement errors mainly due to vertical angulation errors when not executed with a precise paralleling technique.1, 9
Even though a reporting precision of 0.1 mm is desired in studies, it is considered utopic.9 - 11 In everyday clinical situations, 0.5 mm should be the maximum level of precision in peri-implant bone level evaluation.
Precision is where stereoradiography can be beneficial. Stereoscopic imaging seems to allow for a more accurate assessment of peri-implant bone level and provides a more comprehensive evaluation of the structures� depth and relative position.9, 11, 12 However, no controlled study has objectively quantified this advantage, nor has the technique been studied and described in terms of ideal angles of stereoscopy.
Stereoscopic radiographs are obtained from two slightly different perspectives of the same subject, captured with a small horizontal displacement or rotation of the X-ray tube between exposures. Depending on the intended intensity of the stereo effect, the clinician could move the tube 1 cm to the left and right of the orthogonal position, which is equivalent to a 4� rotation when using a long-cone paralleling technique.9 The images are then presented separately to each eye using a stereoscopic viewing device.12
Alternatively, with some practice, they can be viewed sideby- side on the computer screen by adjusting eye convergence.
Using pairs of stereoscopic radiographs, it is even possible to calculate the 3D coordinates and relative distances, providing valuable information for treatment planning and rehabilitation.13
Stereoradiography was once a highly relevant and researched technique.9, 11 - 13 However, with the advent of volumetric imaging techniques such as CT and CBCT, stereoradiography fell out of favor due to limitations in reproducibility and difficult viewing methods. Arguably, stereoradiography should be revisited in the light of recent augmented reality/ virtual reality (AR/VR) technological developments. AR/VR technology has the potential to enhance the visualization of stereoscopic intraoral radiographic images and provide a more immersive and accurate viewing experience, with relatively low-dose acquisition and low-cost visualization equipment.
Thus, it could be particularly valuable in the field of dentomaxillofacial stereoradiography, where precise measurements and localization of noble structures or foreign bodies are crucial for surgical success.14
The main objective of this in vitro study was to evaluate the accuracy of stereoradiography in measuring peri-implant bone level, in comparison to 2D methods, and to define which stereoscopic angles between images provide more accurate information. This research also aimed to address the limitations and challenges associated with traditional 2D imaging viewing techniques and develop a virtual reality-based method for viewing pairs of stereoscopic radiographs and storing, analyzing, and making measurements in the acquired stereoscopic images in a reproducible 3D environment.
In summary, this research tests the working hypothesis that stereoradiography provides significant accuracy and precision improvement over 2D radiography in measuring peri-implant bone level.
Material and methods
A laboratory study was conducted to compare stereoradiography and conventional 2D radiography. Ten artificial bon� blocks were evaluated from all four sides, giving a total of 40 samples where titanium implant replicas (Osteotech Lda, Portugal) were inserted at random heights and angles (between �1� and �20.7�), simulating random bone defects and crestal angulations.15 The blocks had a 2x2 cm base, were 2 cm tall, and the top surface where the implants were inserted was 1.5x1.5 cm. The implant replicas had a diameter of 3 mm and a 7.5 mm long surface with circular threads spaced at 0.4 mm, with a smooth surface neck and an asymmetric tip to connect to the step motor axis.
A microstep motor with a digital control unit (Resopark SA, Portugal) and a 0.01� rotation step precision was specially developed for this study. It rotated the samples around the implant axis (fixed to the step motor axis), holding the implant parallel to the sensor surface and at 30 cm from the X-ray source, leaving the artificial bone block to rotate with several implant-to-bone angulations. The X-ray source was stationary and aimed perpendicularly at the implant and the sensor, which were positioned, with the motor, in an aluminum box frame constructed for this research.
Each sample was radiographed at 0�, +/-1�, +/-2�, +/-3�, +/- 4�, +/-5�, +/-6�, and +/-7� from the implant axis. Seven stereoscopic image pairs per sample were created by joining the positively angled radiographs with the negatively angled ones, while the 0� radiograph served as the 2D conventional radiograph.
A total of 320 image pairs were created using this method: 7 pairs in 3D and 1 pair in 2D, totaling 8 pairs per sample.
The samples were radiographed with an intraoral direct digital sensor (RVG 5100, Kodak, USA) and a 70-KV, 8-mA X-ray tube (Irix 70, Trophy, France), with a 0.30-s exposure time, and the central beam directed perpendicularly to the implant axis with a focus-to-object distance of 30 cm (long-cone parallelling technique).
All the images were mirror-inverted to simulate a lingual-side viewing method, cropped to 1200x1400 pixels with 256 gray levels (IrfanView v.4.67-64-bit, Irfan Skiljan, Bosnia), and assembled into stereo pairs in MPO format (Stereo Photo Maker Pro - 64bit v.6.31, Masuji Suto, Japan). The mirror inversion is necessary to reduce the depth cue conflict, inducing an inverted stereoscopic effect. The stereoscopic perception of a structure closer to the observer, having its limits less sharp than the distant structures (closer to the sensor surface), would cause confusion and eye strain. This issue would happen with the conventional buccal side viewing method and is thus prevented by inverting the images and providing a lingual view.
Three observers, blinded to the true implant-to-bone heights and angles, interpreted the images using a head-mounted display (Oculus Quest 3, Meta, USA) with a 3D projection software (ImmerGalery v.1.2.6, ImmerVR GmbH, Germany). The software projected an amplified 3 m high image in a standardized brightness and contrast mode,
against a dark background. The observers assessed the bon� level in a randomized order, using a precision pointer to count the amount of exposed circular threads (first boneto-implant contact) on the left, right, front (lingual), and behind (buccal) of each implant�s neck (Figures 1 and 2).
�
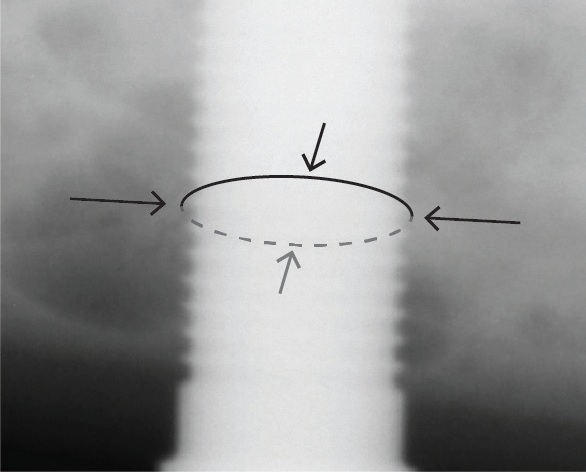
Figure 1. Measurement points at mesial, distal, buccal, and lingual sides with auxiliary circular threads at 0.4-mm intervals.
�
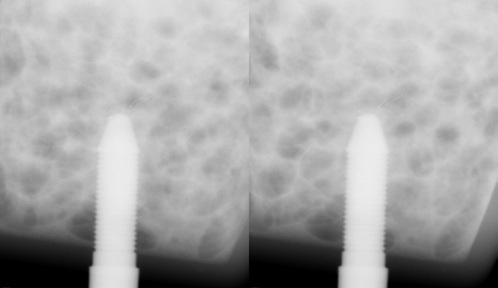
Figure 2. Stereoradiography (crossed-eye) pair at a 6� stereopsis angle (readers can look at the image by crossing the eyesight until three images are visible, then concentrate on the middle one, which will be in 3d). the lower part of the bone block is in front of the implant, superimposing the threads, conveying the illusion that there are no threads exposed, while in reality, there are between 6 (right side) and 10 (left side) exposed threads.
�
Each thread was spaced at 0.4 mm, and observers were asked to register a precision of half a thread (0.2 mm). The implant neck was considered to be the smooth surface adjacente to the threads, and the exposed threads simulated the bone dehiscence. Thus, the circular (non-helicoidal) threads served as a measuring instrument (ruler) with a precision of 0.2 mm.
Observers did not know the stereoscopic angle used on each image pair, nor if it was 2D or 3D, and performed all the measurements without feedback about the measurement error.
There was no intra or inter-observer calibration since the goal was to evaluate their accuracy and precision. They only received instructions on the viewing software interface and were asked to perform the measurements without previous training. Observers were also asked to report on the subjective visual strain from looking at the images on a scale from 1 to 5, where 1 meant a very uncomfortable image with an exaggerated stereoscopic effect, 3 the comfort limit, and 5 a very comfortable image.
A total of 1600 measurements per observer were registered on an online table (Google Sheets, Google LLC, USA). The collected data was compared to the �true� measurements acquired with a CBCT (Hyperion X9 Pro, Cefla, Italy) with a 4x4 mm field of view at 68-μm Voxel. Implant-to-surface angles in degrees and implant-to-bone heights in millimeters were measured using CBCT workstation software (Irys v.16.0, Cefla, Italy). Implant neck-to-bone heights were confirmed visually by counting the exposed threads directly on the samples. Data was analyzed using Matplotlib v.3.9.0 and Python v.3.11 (Python Software Foundation, USA).
Medians of absolute errors and interquartile ranges were calculated to compare the accuracy and dispersion of the observations.
Since the underlying distribution is unknown and likely dependent on the stereopsis angles, the bootstrap statistical test was used to infer the median absolute error for the different stereopsis angles.16
�
Results
No observer reported discomfort in 2D images, and they all classified those with a score of 5 (maximum viewing comfort). Visualization comfort decreased with the stereoscopic angle of stereopsis (Figure 3). Angles above 6� were classified as uncomfortable.
�
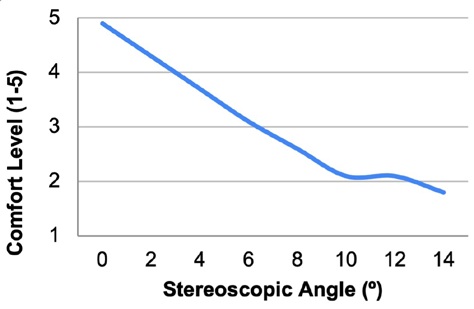
Figure 3. Average comfort perception variation in relation to the stereoscopic angle (5 = very comfortable; 3 = acceptable; 1 = very uncomfortable)
�
The implant�s neck-to-bone distance measured by each participant based on threads was converted to millimeters and compared to the actual distance to obtain the relative and absolute errors. The measurements were analyzed independently for each implant side and together for the overall perception of peri-implant bone height. Figure 4 shows the median absolute error, which is smaller for all stereoscopic angles when compared to 2D.
�
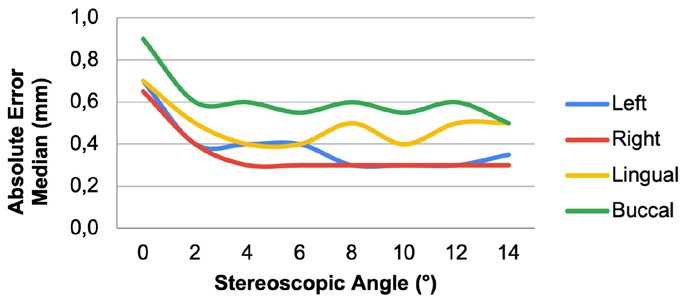
Figure 4. Median absolute error variation in relation to the stereoscopic angle
�
The introduction of the stereoscopic technique also decreased the dispersion in measurements, as reflected by the smaller interquartile range in stereoscopy (Figure 5). Moreover, the stereoscopic measurements showed an overall increase in accuracy, with more measurements within 0.2 mm of the actual values compared to the 2D measurements (Figure 6).
�
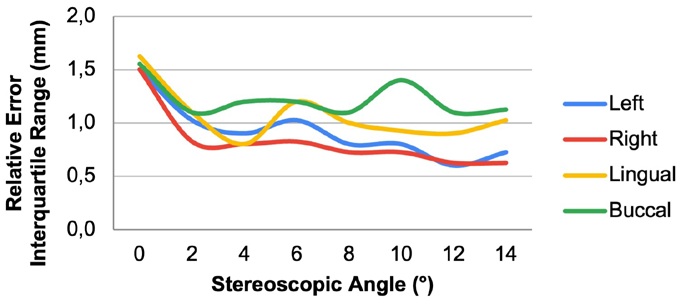
Figure 5. Relative error interquartile range variation in relation to the stereoscopic angle
�
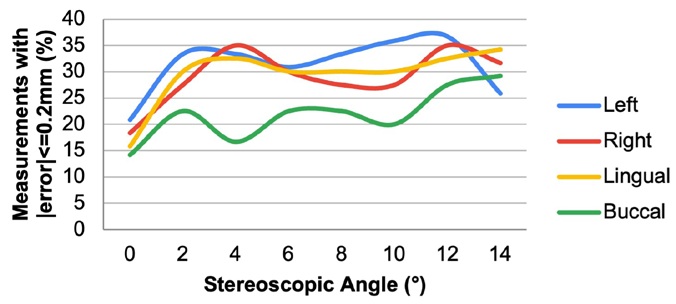
Figure 6. Number of measurements (in percentage) that agreed with the actual value with an error of less than 0.2 mm
�
Discussion
The obtained results showed a substantial reduction in the error of bone height estimation when any stereoscopic images were used, even at low angular disparities such as 2� of stereopsis.
Figure 7a) shows the box-and-whiskers plot for the bone-level identification error as a function of the stereopsis angle. There is a larger statistical dispersion of the bone-level identification error for a stereopsis angle of 0� compared to all other angles. This larger dispersion is also seen when comparing Figures 7b) and 7c), which show the histogram of the bone-level identification error for a stereopsis angle of 0� and 8�, respectively. The median value of the absolute error across all measurements was 0.7 mm for a stereopsis angle of 0� and decreased to 0.3 mm for a stereopsis angle of 8� (Figure 7a).
�
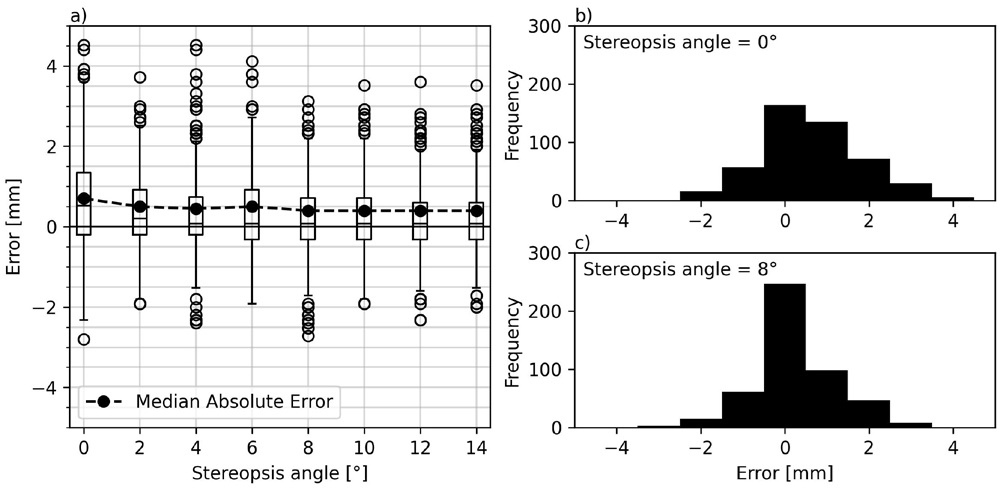
Figure 7. a) Box-and-whisker plot of the relative error in identifying the bone level as a function of the stereopsis angle used to produce the stereoscopic image. The black dashed line represents the median absolute error. b) Histogram of the bone-level identification error for a stereopsis of 0 degrees. c) Histogram of the bone-level identification error for a stereopsis of 8 degrees.
�
The error was systematically higher in the buccal measurements. Figure 6 shows that less than one-third of the measurements at the buccal margin achieved an absolute error of less than 0.2 mm.
The bootstrap statistical test16 was used to infer the median absolute error for stereopsis angles 0� and 8�. For 0�, the median absolute error was between 0.6 and 0.8 mm (95% confidence interval). For 8�, the median absolute error was between 0.3 and 0.5 mm (95% confidence interval). The 8� stereopsis angle led to a better accuracy with a p-value smaller than 0.001 for the null hypothesis, which stated that there is no difference in median absolute errors between the two stereopsis angles.
These results agree with the literature,9, 17 although this study covers a broader range of implant-to-bone angles. Hollender and Rockler9 compared 0� and 15� of beam angulation related to the implants and also found 3D to be more accurate than 2D with the same 0.3 mm error. However, they inserted the implants perpendicular to a flat bone surface, while our study used oblique implant positions of up to 21� to the bon� surface, simulating clinical situations from normal to severe bone loss; yet, we found the same error reduction.
Accuracy tests related to digital intraoral imaging are usually only evaluated on the mesial and distal margins of implants, and the literature reports a precise paralleling technique perpendicular to the implant and parallel to the bon� surface.18 In this study, the median error values were obtained from mesial, distal, buccal, and lingual sites, reaching an average of 0.3 mm accuracy.
By providing more comprehensive and accurate data, stereoradiography can support the training and validation of machine learning models for tasks such as image segmentation, object recognition, and anatomical measurements, which rely on volumetric data.This study�s main limitation is that the results differed only in higher bone angulations. If we consider only the smaller implant-to-bone angulations, then the obtained error values of 0.1 mm are similar to the literature, and no apparent difference was found between 2D and 3D images.
Another limitation relates to the reduced number of observers and the idealized in vitro conditions, which do not necessarily translate to normal clinical conditions with all dental professionals. Further studies in cadavers, simulating normal clinical situations, should be performed to validate this technique.
The main advantage shown in this study is that it addresses different angulations, from 1� to 21�. Compared to the 2D images, all stereoscopic angles greater than zero led to an improved identification of the bone level, even in buccal and lingual implant sides. Moreover, this study provides a quantitative analysis of the benefits of stereoscopy.
Concerning the ideal 3D angulation or stereo base, there seems to be no substantial improvement in accuracy nor dispersion reduction with angles greater than 4�. Furthermore, angles greater than 6� lead to an expected increased visual fatigue,(19) as reported by the observers. Thus, a stereopsis angle between 4� and 6� would be the most effective method to reduce the measurement error without sacrificing viewing comfort.
Conclusions
Stereoscopic intraoral radiography is more accurate than 2D intraoral radiography in evaluating peri-implant bone levels in all faces, including buccal and lingual, when implant-to-bone angulations are present or unknown. Any stereopsis� base angulation is more effective than 2D, but angulations over 6� should be avoided because of visual discomfort. Angular values between 4� and 6� were the most effective overall. Implant-tobone angulations up to 20� can be accurately evaluated with stereoscopic intraoral radiography, with the use of a high-resolution AR/VR head-mounted display system, which can provide a more immersive and accurate viewing experience, allowing for a more precise evaluation of peri-implant bone level.
�
References
1. Gupta I, Chaudhry A, Savita S, Shetti A. Radiographic Assessment of Peri-implant Bone Level � A Comparative Study of Digital Intraoral and Digital Panoramic Radiography. Stomatol Glas Srb. 2019;62:117-21.
2. Kim MJ, Lee SS, Choi M, Yong HS, Lee C, Kim JE, et al. Developing evidence-based clinical imaging guidelines of justification for radiographic examination after dental implant installation. Bmc Med IMAGING. 2020;20:102.
3. Dave M, Davies J, Wilson R, Palmer R. A comparison of cone beam computed tomography and conventional periapical radiography at detecting peri-implant bone defects. Clin Oral Implants Res. 2013;24:671-8.
4. Barootchi S, Tavelli L, Majzoub J, Chan HL, Wang HL, Kripfgans OD. Ultrasonographic Tissue Perfusion in Periimplant Health and Disease. J Dent Res. 2022;101:278-85.
5. Orhan K, Serindere G, Belgin CA, Kurt MH. Evaluation of the visibility of peri-implant bone defects using ultrasonography with two types of probes. J Ultrason. 2021;21:e206-12.
6. Siqueira R, Sinjab K, Pan Y-C, Soki F, Chan H-L, Kripfgans O. Comprehensive Peri-implant Tissue Evaluation with Ultrasonography and Cone-Beam Computed Tomography: A Pilot Study HHS Public Access. CLIN ORAL IMPLANT RES. 2021;32:777-85.
7. Miotk N, Schwindling FS, Zidan M, Juerchott A, Rammelsberg P, Hosseini Z, et al. Reliability and accuracy of intraoral radiography, cone beam CT, and dental MRI for evaluation of peri-implant bone lesions at zirconia implants − an ex vivo feasibility study. J DENT. 2023;130:104422.
8. K�hl S, Z�rcher S, Zitzmann NU, Filippi A, Payer M, Dagassan- Berndt D. Detection of peri-implant bone defects with different radiographic techniques � a human cadaver study. CLIN ORAL IMPLANTS RES. 2016;27:529-34.
9. Hollender L, Rockler B. Radiographic evaluation of osseointegrated implants of the jaws. Experimental study of the influence of radiographic techniques on the measurement of the relation between the implant and bone. DENTOMAXILLOFAC RADIOL. 1980;9:91-5.
10. Schulze RKW, d�Hoedt B. Mathematical analysis of projection errors in �paralleling technique� with respect to implant geometry. Clin Oral Implants Res. 2001;12:364-71.
11. Sewerin IP. Errors in radiographic assessment of marginal bone height around osseointegrated implants. Eur J Oral Sci. 1990;98:428-33.
12. Raper HR. ELEMENTARY AND DENTAL RADIOGRAPHY. 1st ed. Claudius Ash, Sons & Co. Ltd., 1913.
13. Sherlock RA, Aitken WM. A method of precision position determination using x-ray stereography. Phys Med Biol. 1980;25:349-55.
14. van Beurden MHPH, IJsselsteijn WA, Juola JF. Effectiveness of stereoscopic displays in medicine: A review. 3D RES. 2012;3:1-13.
15. Freitas GDR, Poleti ML, Xavier CRG, Ara�jo AC, Capelozza ALA. Fabrication of plaster models with radiographic features of human bone: a pilot study by fractal analysis. Rgo (Porto Alegre). 2012;60:163-7.
16. Efron B, Tibshirani Rj. An Introduction To The Bootstrap. 1st Ed. Chapman and Hall/CRC, 1994.
17. Lang NP, Wilson TG, Corbet EF. Biological complications with dental implants: their prevention, diagnosis and treatment. Clin Oral Implants Res. 2000;11(Suppl.1):146-55.
18. De Smet E, Jacobs R, Gijbels F, Naert I. The accuracy and reliability of radiographic methods for the assessment of marginal bone level around oral implants. Dentomaxillofacial Radiol. 2002;31:176-81.
19. Leroy L. Eyestrain Reduction In Stereoscopy. Wiley, 2016.
�
Jorge Ferreira da Costa
E-mail address: jfc@fmd.ulisboa.pt
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
CRediT authorship contribution statement
Jorge Ferreira da Costa: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Writing � original draft; Writing � review & editing. Jo�o Caram�s: Supervision, Writing � review & editing. Daniel Hachmeister: Data curation, Formal analysis, Methodology, Validation, Writing � review & Editing
�
Acknowledgments
The authors acknowledge the help of Osteotech, Lda., which manufactured the test implants, and Resopark, SA, which provided the step motor and digital control unit used to measure precisely the rotation of the samples to be radiographed.
Conflict of interest
The authors have no conflicts of interest to declare.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
