
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (1) | 25-30
Clinical case
Oral and craniofacial manifestations in an individual with Seckel syndrome features: A case report
Manifestações orais e craniofaciais num indivíduo com características da síndrome de Seckel: Um relato de caso
a Department of Dental Clinic, Federal University of Ceará, Fortaleza, Brazil
b Department of Dentistry, Faculty of Health Sciences, Zambeze University, Tete, Mozambique
Eduardo Frederico Eduardo Maferano - maferanoeduardo@gmail.commaferanoeduardo@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 1
Clinical case
Pages - 25-30
Go to Volume
Article History
Received on 20/03/2024
Accepted on 15/02/2025
Available Online on 30/03/2025
Keywords
Clinical Case Report
�
Oral and craniofacial manifestations in an individual with Seckel syndrome features: A case report
Manifesta��es orais e craniofaciais num indiv�duo com caracter�sticas da s�ndrome de Seckel: Um relato de caso
�
Lorena Sousa do Bonfim Costa1 0000-0001-8926-6785
Eduardo Frederico Eduardo Maferano1,2,* 0009-0004-4182-1881
Sara Maria Silva1 0000-0003-4025-4315
Thyciana Rodrigues Ribeiro1 0000-0002-6614-6809
F�bio Wildson Gurgel Costa1 0000-0002-3262-3347
1Department of Dental Clinic, Federal University of Cear�, Fortaleza, Brazil.
2Department of Dentistry, Faculty of Health Sciences, Zambeze University, Tete, Mozambique.
�
�
Article history:
Received 20 March 2024
Accepted 15 February 2025
Available online 18 March 2025
�
Abstract
This study aims to describe the oral and craniofacial findings of a patient undergoing genetic investigation related to Seckel syndrome. A 36-year-old patient, during clinical examination, exhibited general manifestations potentially associated with Seckel syndrome, such as microcephaly, harmonious short stature, and compensated cardiopathy with the use of a pacemaker, besides intellectual deficit. Among the orofacial findings, significant mandibular atrophy with discontinuity of the inferior alveolar neurovascular canal, taurodontism in posterior teeth, and micrognathia were observed. The need for procedures such as extractions and/or endodontic treatment, evidenced after clinical history analysis and physical examination, especially in the lower teeth, posed a clinical challenge due to the thin mandibular bone thickness and dental apices� proximity to the mandibular canal. This study highlights the findings of a patient who exhibits clinical features consistent with Seckel syndrome based on observed physical, oral, and maxillofacial alterations despite the absence of confirmed genetic characterization. It also highlights the absence of standardized clinical approaches in the care plan for this patient group.
Keywords: Dental clinics, Seckel syndrome, Special needs patients
�
Resumo
Este estudo tem como objetivo descrever os achados orais e craniomaxilofaciais de uma paciente em investiga��o gen�tica relacionada com s�ndrome de Seckel. Uma paciente de 36 anos, durante o exame cl�nico, apresentou manifesta��es gerais possivelmente associadas � s�ndrome de Seckel, como microcefalia, estatura baixa harmoniosa e cardiopatia compensada com o uso de pacemaker, al�m de d�fice intelectual. Entre os achados orofaciais, observou-se significativa atrofia mandibular com descontinuidade do canal do feixe neurovascular alveolar inferior, taurodontia em dentes posteriores e micrognatia. A necessidade de procedimentos como extra��es e/ou tratamento endod�ntico, evidenciada ap�s an�lise da hist�ria cl�nica e exame f�sico, especialmente nos dentes inferiores, apresentou-se como um desafio cl�nico devido � fina espessura �ssea mandibular e � proximidade dos �pices dent�rios com o canal mandibular. Este estudo destaca os achados de uma paciente que apresenta caracter�sticas cl�nicas consistentes com a s�ndrome de Seckel, com base em altera��es f�sicas, orais e maxilofaciais observadas, apesar da aus�ncia de caracteriza��o gen�tica confirmada. Destaca-se ainda a aus�ncia de padroniza��o de abordagens cl�nicas no plano de cuidados deste grupo de pacientes.
Palavras-chave: Cl�nica dent�ria, S�ndrome de Seckel, Pacientes com necessidades especiais
�
Introduction
Seckel syndrome (SS) is a rare form of primordial dwarfism, characterized as a genetic condition involving chondrodysplasia with an autosomal recessive inheritance. Its incidence is estimated at 1:10,000 live births, affecting both sexes equally and, to date, showing no specific association with any particular ethnicity or defined geographic boundaries.1 The manifestations of SS are notably heterogeneous, and due to the limited number of cases, the available literature provides only brief descriptions.2
SS was first described by Rudolph Virchow in 1892 as �bird-headed dwarfism,� owing to the typical physical and facial characteristics observed in affected individuals. Later, in 1960, Seckel studied the condition based on cases of microcephaly in dwarfs, consolidating current knowledge on the syndrome.3 Diagnosis is based on clinical, radiographic, and genetic findings, which may involve more than one genetic locus, as well as various concomitant conditions that may manifest in mild or severe forms.2, 4
Studies involving genetic analysis in families with multiple members exhibiting characteristics consistent with SS and a history of consanguinity observed mutations in the CENPJ gene, initially described as associated with microcephaly.5 Another gene, CDK5RAP2, has also been linked to isolated cases of SS. This association may be related to errors in the mitotic spindle formation, resulting in cells with abnormal centrosomal proteins and nuclei.6
Among the main clinical findings of SS are proportional dwarfism from fetal development, microcephaly, intelectual disability, and a �bird-like face� due to recessed glabela and chin and a prominent or hooked nose. Other features include skeletal and dental abnormalities, sparse hair, delayed bone age observed in radiographs of the hand and wrist, phonological limitations or absence of speech, and vascular, coronary, hematologic, genitourinary, and nervous system abnormalities.4, 7, 8
Radiographically, panoramic and lateral facial radiographs may show marked mandibular hypoplasia and significant nasal cartilage projection.9 Reported oral manifestations include malformed and missing teeth, micrognathia, palatal arch abnormalities such as a high-arched palate, and incomplete palatal closure presenting as cleft palate. Other findings observed are enamel hypoplasia, oligodontia, taurodontia, mandibular and zygomatic hypoplasia, and a Class II facial pattern.10
Considering SS oral and craniofacial findings and their potential relevance for treatment and therapeutic planning, this case report aims to describe a patient with facial and physical characteristics consistent with SS, treated at the Integrated Dentistry Clinic of the Federal University of Cear� (UFC), Fortaleza, Brazil.
Case Report
A 36-year-old Caucasian woman with clinical findings and phenotypic characteristics suggestive of SS was under investigation for SS molecular characterization at the genetics clinic of the UFC. She had a history of heterozygous genes for recessive syndromes. The patient sought dental care at UFC, reporting localized sensitivity in the lower right posterior region associated with halitosis, and pain in the temporomandibular joint region. She also expressed aesthetic and functional dissatisfaction with her maxillomandibular relationship, mentioning difficulties in maintaining proper oral hygiene due to the reduced size of her oral cavity and motor incoordination.
Extraoral physical examination (Figure 1) detected a Class II maxillomandibular relationship with an anterior open bite, a retruded chin, fine and sparse hair, small ears with low implantation, strabismus, and a syndromic facial appearance characteristic of SS, with a prominent and pointed or hooked nose. Clinically, the patient presented with na increased distance between her eyes, a prominent frontal region, microcephaly, proportional short stature (1.5 meters), low weight (39.9 kg), small hands and feet, a narrow face, and micrognathia.
�
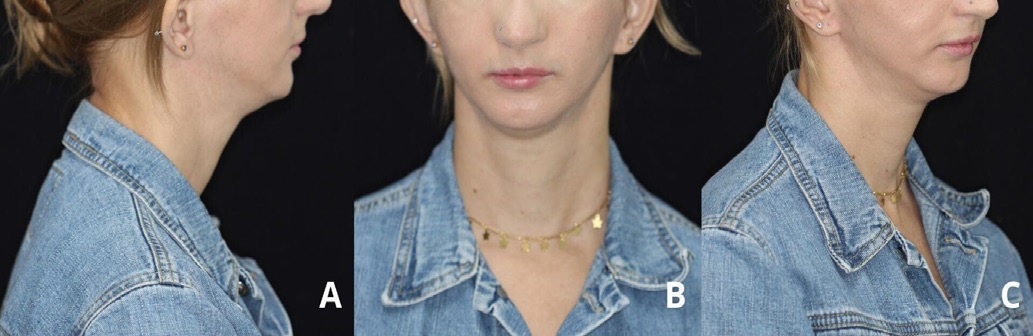
Figure 1. Extraoral photographs of the patient: (A) Lateral view showing a Class II maxillomandibular relationship and a retruded chin; (B) Frontal view displaying the prominent, pointed or hooked nose; (C) Oblique view showing the small ears with low implantation.
�
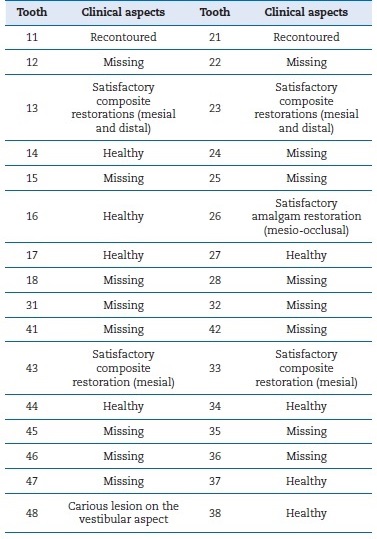
Intraoral examination (Figure 2 and Table 1) revealed a reduced oral cavity size. Inspection of the mucosa showed no alterations or pathologies. Multiple dental elements�18, 24, 25, 28, 47, 46, 45, 35, and 36�were missing due to extractions secondary to early caries and agenesis of teeth 12, 22, 31, 32, 41, and 42. Additionally, supragingival calculus was detected in all sextants, and a large carious lesion was identified on the buccal surface of tooth 48, near the gingival margin. Satisfactory composite resin restorations were observed on teeth 13, 11, and 21, which, according to the patient, had been recontoured due to their previous �cone-shaped� appearance. There were also other satisfactory composite resin restorations on teeth 23, 33, and 43 and a satisfactory Class II mesio-occlusal amalgam restoration on tooth 26. The patient had been using removable upper and lower partial dentures for 20 years, with good adaptation but poor hygiene. Radiographic examinations were requested: panoramic X-ray, lateral cephalogram, and hand and wrist radiographs.
�

Figure 2. Preoperative intraoral photographs of the patient: (A) Occlusal view of the maxilla showing agenesis of the upper lateral incisors; (B) Frontal view showing anterior open bite; (C) Occlusal view of the mandible showing some teeth missing.
�
Table 1. Description of dental findings observed during intraoral examination and planning
�
The panoramic X-ray (Figure 3) revealed significant mandibular hypoplasia, discontinuity of the mandibular canal, and bon� resorption near teeth 34, 35, 44, and 45. The lateral cephalogram (Figure 4) highlighted a disproportion between the neurocranium and the viscerocranium, Class II maxillomandibular relationship, anterior open bite, and notable projection of the nasal cartilage. The hand and wrist radiographs (Figure 5) showed clinodactyly of the first and fifth fingers and shortening of the middle phalanges.

Figure 3. Panoramic radiograph of the patient showing considerable mandibular hypoplasia and discontinuity of the mandibular canal on both sides.
�

Figure 4. Lateral face radiograph showing considerable disproportion between the neurocranium and viscerocranium, Class II maxillomandibular relationship, and anterior open bite.
�

Figure 5. Hand and wrist radiograph revealing clinodactyly of the first and fifth digits and shortening of the middle phalanges.
Regarding her general health, the patient reported a history of congenital heart disease and a pacemaker implanted 15 years prior. She complained of episodes of disorientation, psychomotor agitation, memory loss of recent events, myalgia, muscle fatigue, and frequent antibiotic use due to genitourinary tract infections.
The patient reported that her parents were non-consanguineous and unaffected, and there had been no complications during pregnancy or childbirth. She had a healthy full sibling and three half-siblings unaffected by syndromes or developmental issues. Her maternal half-brother died at 24 years of age from an unspecified cancer. Additionally, her paternal and maternal grandparents were non-consanguineous and were not known to be affected by any genetic conditions.
The patient also mentioned that her paternal grandmother had short stature and low body weight, with features that she believed resembled her own, but no investigation had been done to confirm whether she was affected. Therefore, this relative was considered healthy, as there was no evidence to the contrary. The patient also reported having a daughter born via vaginal delivery without complications, with appropriate height and weight, from a non-consanguineous relationship, and unaffected by any syndrome or developmental deficit (Figure 6).
�
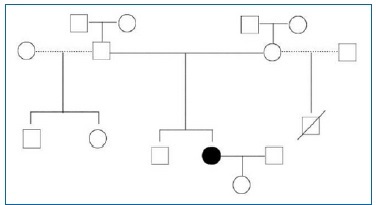
Figure 6. Squares: males; Circles: females; Strikethroughs: deceased; Filled symbol: affected by the syndrome; Unfilled symbol: unaffected; Dashed lines between symbols: extramarital relationships; Solid lines between symbols: non-consanguineous marriages.
�
After documenting all issues in the clinical chart and prioritizing the most urgent complaints, the proposed treatment plan included supragingival scaling of all sextants, restoration of tooth 48, and fabrication of a new removable partial denture.
As an urgent measure, the carious tissue from the buccal surfasse of tooth 48 was partially removed, avoiding pulp exposure.
Its composite resin restoration was performed only after supragingival scaling and prophylaxis of all sextants. The patient was instructed on the importance of proper oral hygiene, emphasizing the use of children�s toothbrushes for better adaptation.
Electric toothbrushes were also recommended. Two weeks after the initial treatment, the patient returned with complaints of pain and malodor in the region of tooth 48, where the composite resin restoration had been performed.
Clinical evaluation revealed that the restoration did not cover the entire cavity, and a less conservative approach was needed to remove more compromised tissue, resulting in pulp tissue exposure. Consequently, an endodontic therapy approach was required for tooth 48, using absolute isolation with a pediatric rubber dam. The periodontal tissues showed improvement two weeks after the supragingival scaling.
One week after the endodontic treatment, the patient returned without pain complaints, showing a significant improvement in periodontal tissues and her oral hygiene. Subsequently, she was referred to the UFC�s Prosthodontics Clinic for the fabrication of a new removable partial denture.
Discussion and Conclusions
This clinical case report describes the oral and craniofacial findings, the clinical management, and the dental treatments performed on a patient under investigation for SS at UFC�s Genetics Outpatient Clinic. The patient had a history of heterozygous genes for recessive syndromes. The evaluation of extraoral and intraoral clinical characteristics identified a Class II maxillomandibular relationship, anterior open bite, micrognathia, conoid teeth, and agenesis of some teeth. These findings led to a clinical diagnosis of SS due to aligning with previous studies.10, 11 However, other oral characteristics mentioned in previous studies, such as generalized enamel hypoplasia, root dysplasia, and palatal shape abnormalities,1, 12 were not observed in this case. Additionally, no previous studies addressed the periodontal health of patients with SS, although periodontal disease with supragingival calculus in all sextants and bone rarefaction were identified.
Bakhshani et al.,13 who reported a case of a patient with SS, observed agenesis of the left central incisor, right second premolar, and lower second permanent molars, contrary to the agenesis of upper lateral incisors, lower central and lateral incisors found in the present case. This discrepancy highlights the variation in dental manifestations of SS, emphasizing the need for personalized evaluations. Furthermore, Bakhshani et al.13 found generalized enamel hypoplasia and disproportionately large crowns, which also contrast with the present case findings.
Considering that SS involves bone alterations, radiographic analysis plays a crucial role in diagnosis. The patient presented with microcephaly, Class II facial profile, mandibular hypoplasia, dental agenesis, short roots, discontinuity of the mandibular canal, and bone resorptions. These findings are consistent with previous research.9 10
Nihill et al.14 outlined the challenges encountered during dental procedures in this patient group due to their pronounced micrognathia, which required rehabilitation methods adapted to the exceptionally short dental arches and the use of pediatric dental instruments. A personalized and multidisciplinar approach was adopted in the present case, considering the limitations and adapting available clinical instruments.
Namely, a pediatric isolation arch and mechanized instrumentation were used during endodontic treatment to reduce the number of sessions and the time with the mouth open, given that the patient reported pain in the temporomandibular joint area.
Due to its phenotypic and genotypic heterogeneity, SS can be confused with other conditions, sharing characteristics such as dwarfism, microcephaly, and skeletal and facial alterations.
Among the syndromes to consider in the differential diagnosis is Silver-Russell Syndrome, also associated with short stature, body asymmetry, and distinct facial features
such as a triangular face and micrognathia. However, the absence of significant microcephaly in Silver-Russell Syndrome is a relevant distinguishing factor,15 and marked microcephaly was observed in the patient in question, reinforcing the diagnosis of SS.
This study highlights several limitations in the literature. Firstly, there is a notable scarcity of information regarding clinical management guidelines for this patient group. Additionally, the literature lacks updated data on oral and craniofacial findings associated with SS.
In the present case, communication during consultations was challenging due to the patient�s difficulty in retaining information, as she frequently attended appointments alone. Despite this, the patient remained friendly, cooperative, and interested in the treatments and oral health during the sessions, understanding the need for multidisciplinar follow-up.
Further studies are recommended to expand knowledge on clinical oral and craniofacial manifestations of SS and to update the available information, aiming to establish more refined practices that meet the specific needs of patients with SS. Such research is essential for developing more robus and effective treatment guidelines for this unique clinical condition.
This study highlights the findings of a patient who exhibited clinical features consistent with SS based on observed physical, oral, and maxillofacial alterations despite the absence of confirmed genetic characterization. SS�s oral and craniofacial manifestations vary significantly. Thus, standardized clinical practices for managing and treating this patient group are required.
�
References
1. Arnold SR, Spicer D, Kouseff B, Lacson A, Gilbert-Barness E. Seckel-like syndrome in three siblings. Pediatr Dev Pathol. 1999;2:180-7.
2. Faivre L, Le Merrer M, Lyonnet S, Plauchu H, Dagoneau N, Campos-Xavier AB, et al. Clinical and genetic heterogeneity of Seckel syndrome. Am J Med Genet. 2002;112:379-83.
3. Reddy S, Starr C. Seckel syndrome and spontaneously dislocated lenses. J Cataract Refract Surg. 2007;33:910-2.
4. Gupta A, Fazal TS, Arora R. Antenatal diagnosis of seckel syndrome. J Obstet Gynaecol India. 2014;64:6-8.
5. Al-Dosari MS, Shaheen R, Colak D, Alkuraya FS. Novel CENPJ mutation causes Seckel syndrome. J Med Genet. 2010;47:411-4.
6. Yigit G, Brown KE, Kayserili H, Pohl E, Caliebe A, Zahnleiter D, et al. Mutations in CDK5RAP2 cause Seckel syndrome. Mol Genet Genomic Med. 2015;3:467-80.
7. Salman BN, Biglar N, Mirkeshavarz M, Ansari G. Clinical Findings and Dental Manifestations Associated With Microcephalic Osteodysplastic Primordial Dwarfism Type II: A Case Report. J Pediatr Rev. 2022;10:321-30.
8. Donmez YN, Giray D, Epcacan S, Goktas E, Aypar E. Cardiovascular anomalies in Seckel syndrome: report of two patients and review of the literature. Cardiol Young. 2022;32:487-90.
9. Brito AF, Baldrighi SEZM. Repercuss�es fonoaudiol�gicas na S�ndrome de Seckel: estudo de caso. Rev CEFAC. 2015;17:1698�715
10. Kjaer I, Hansen N, Becktor KB, Birkebaek N, Balslev T. Craniofacial morphology, dentition, and skeletal maturity in four siblings with Seckel syndrome. Cleft Palate Craniofac J. 2001;38:645-51.
11. Seymen F, Tuna B, Kayserili H. Seckel syndrome: report of a case. J Clin Pediatr Dent. 2002;26:305-9.
12. De Coster PJ, Verbeeck RM, Holthaus V, Martens LC, Vral A. Seckel syndrome associated with oligodontia, microdontia, enamel hypoplasia, delayed eruption, and dentin dysmineralization: a new variant? J Oral Pathol Med. 2006;35:639-41.
13. Bakhshani S, Zarch SHH, Moghadam MI, Pakfetrat A. Seckel syndrome associated dental anomaly; case report. Academic Journal of Health Sciences. 2021;36:76-83.
14. Nihill P, Lin LY, Salzmann LB, Stevens S. Esthetic overdenture for a patient with possible Seckel syndrome. Spec Care Dentist. 1996;16:210-3.
15. Kılın� MO, Ninis VN, Uğur SA, T�ys�z B, Seven M, Balcı S, et al. Is the novel SCKL3 at 14q23 the predominant Seckel locus? Eur J Hum Genet. 2015;23:140.
�
Eduardo Frederico Eduardo Maferano
E-mail address: maferanoeduardo@gmail.com
�
CRediT authorship contribution statement
Lorena Sousa do Bonfim Costa: Conceptualization, Data curation, Investigation, Methodology. Eduardo Frederico Maferano: Data curation, Methodology, Validation, Writing � review & editing. Sara Maria Silva: Methodology, Validation. Thyciana Rodrigues Ribeiro: Methodology, Validation, Visualization. F�bio Wildson Gurgel Costa: Methodology, Validation, Supervision, Writing � review & editing.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
