
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (1) | 10-16
Original research
Relationship between the position of the impacted third molar and associated pathologies – A retrospective CBCT study
Relação entre a posição do terceiro molar impactado e patologias associadas – Estudo retrospetivo em imagens CBCT
a Faculdade de Medicina Dentária da Universidade do Porto, Porto, Portugal
Sofia Scapini - sofiascapini1@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 1
Original research
Pages - 10-16
Go to Volume
Article History
Received on 20/11/2024
Accepted on 07/03/2025
Available Online on 31/03/2025
Keywords
Original Research
�
Relationship between the position of the impacted third molar and associated pathologies � A retrospective CBCT study
Rela��o entre a posi��o do terceiro molar impactado e patologias associadas � Estudo retrospetivo em imagens CBCT
�
Sofia Scapini1,* 0009-0004-5820-4345
Pedro Mesquita1 0000-0003-0735-2482
1 Faculdade de Medicina Dent�ria da Universidade do Porto, Porto, Portugal
�
�
Article history:
Received 20 November 2024
Accepted 7 March 2025
Available online 24 March 2025
�
Abstract
Objectives: This study aims to evaluate, through an imaging analysis, the correlation between the position of the impacted third molar and the incidence of associated pathologies. It also seeks to analyze the prevalence of these pathologies and their correlation with the sex and age of the patients.
Methods: A total of 585 imaging exams of patients seen at a Portuguese institution of higher education in dentistry were evaluated, from which 235 impacted third molars were selected. The position and associated pathologies were analyzed individually in cone-beam computed tomography scans based on Winter�s, Pell & Gregory�s and Ericson et al.�s classification using Planmeca Romexis software. The data were statistically analyzed in the Statistical Package for the Social Sciences program, using the chi-square and Fisher's exact tests.
Results: Statistically significant differences were found between the incidence of pathology and the position of the third molar. According to Winter's classification, external root resorption was associated with the mesioangular position (p=0.001) and decreased bone density with the distoangular position (p=0.051). Based on Pell & Gregory's classification, external root resorption is related to Position C (p<0.001), caries to Position B (p<0.001), and decreased bone density to Position B (p=0.013) and Class II (p=0.021). Age and sex influenced caries (p=0.006) and decreased bone density (p=0.065), respectively.
Conclusions: This study concluded that there is a correlation between the position of impacted third molars and certain associated pathologies, which can be influenced by age and sex.
Keywords: Cone-beam computed tomography, Dental caries, Odontogenic cysts, Odontogenic tumors, Pericoronitis, Root resorption, Third molar
�
Resumo
Objetivos: Este estudo visa avaliar a correla��o entre a posi��o do terceiro molar impactado e a incid�ncia de patologias associadas atrav�s de uma an�lise imagiol�gica. Procura, igualmente, analisar a preval�ncia dessas patologias e a sua correla��o com o sexo e a idade.
M�todos: Foram avaliados 585 exames imagiol�gicos de pacientes observados numa institui��o portuguesa de ensino superior de medicina dent�ria, de onde se selecionaram 235 terceiros molares impactados. A an�lise e classifica��o da posi��o e das patologias associadas foi realizada atrav�s da observa��o de tomografias computorizadas de feixe c�nico, recorrendo �s classifica��es de Winter, Pell & Gregory e Ericson et al., utilizando o programa inform�tico Planmeca Romexis. Os dados foram analisados no programa Statistical Package for the Social Sciences, recorrendo aos testes de qui-quadrado e exato de Fisher.
Resultados: Detetaram-se diferen�as estatisticamente significativas entre a incid�ncia de patologia e a posi��o do terceiro molar. Segundo a classifica��o de Winter, a reabsor��o radicular externa est� associada � posi��o mesioangulada (p=0,001) e a diminui��o de densidade �ssea � distoangulada (p=0,051). De acordo com a classifica��o de Pell & Gregory, a reabsor��o radicular externa est� relacionada com a Posi��o C (p<0,001), a c�rie com a Posi��o B (p<0,001) e a diminui��o da densidade �ssea com a Posi��o B (p=0,013) e a Classe II (p=0,021). A idade e o sexo influenciaram a c�rie (p=0,006) e a diminui��o da densidade �ssea (p=0,065), respetivamente.
Conclus�es: Este estudo permitiu concluir que h� correla��o entre a posi��o dos terceiros molares impactados e determinadas patologias associadas, que podem ser influenciadas pela idade e pelo sexo.
Palavras-chave: Tomografia Computorizada de Feixe Cónico, Cárie dentária, Quistos odontogénicos, Tumores odontogénicos, Pericoronarite, Reabsorção radicular, Terceiro molar
�
Introduction
Third molars (M3) are the teeth with the highest impaction rate in the human dentition.1 - 3 A tooth is considered impacted when, after at least 2/3 of the roots are formed, it cannot reach the occlusal plane within the expected time interval.4 The causes of impaction include lack of space, malposition, or mechanical barriers along its path.2, 5, 6
Depending on their position, impacted M3 are often associated with different pathologies, such as external root resorption (ERR), carious lesions, pericoronitis, and odontogenic tumors/cysts.2, 7 The detection and diagnosis of these lesions require a detailed anamnesis, a careful clinical assessment, and complementary diagnostic tests.8
ERR of second molars (M2) occurs due to osteoclastic activity triggered by the increased pressure caused by the impacted tooth.2, 3, 9 This pathology is difficult to diagnose and usually progresses silently, with symptoms appearing later when the root pulp is affected (poor prognosis).2, 3, 9
Dental caries is a multifactorial disease that depends on individual, temporal, and sociodemographic factors.10 When distal to the M2, dental caries develop gradually and result from bacterial biofilm accumulation. The M3 position may promote food impaction and create a favorable environment for caries evolution.9, 11
Pericoronitis corresponds to inflammation of the soft tissues surrounding an impacted tooth caused by bacterial action.12 It is usually directly related to local conditions (periodontal pockets) that promote the proliferation of bacteria.12 This condition is often associated with pain, swelling, increased probing depth, and, in more severe cases, decreased bone density distal to the impacted M3.12 Diagnosis is clinical and may be detected radiographically in advanced stages.12
As for odontogenic cysts/tumors associated with impacted M3, their diagnosis requires clinical and radiographic evaluation with histological confirmation.13 This pathology might be asymptomatic, hindering early diagnosis and treatment.1, 2, 14
The gold standard method to analyze and classify M3 is panoramic radiographs.2, 14 Conversely, two-dimensional (2D) images are subject to distortion, artifacts, and overlaps that can lead to misinterpretations.14, 15 Therefore, cone-beam computed tomography (CBCT) has emerged as a solution that allows analyzing structures in their three-dimensional volume, with greater detail and less distortion � essential for detailed diagnoses.14, 16 CBCT involves more exposure to radiation and a higher cost, so its prescription must be responsible.16, 17 This exam should be requested when the dentist has a clinical question that cannot be answered using 2D images,14, 17, 18 bringing a clear benefit to the surgery.<6, 19
This research aims to assess a possible correlation between the position of the impacted M3 and the prevalence of associated pathologies exclusively through an imaging analysis in a population of patients who attended an appointment at the Faculty of Dental Medicine of the University of Porto (FMDUP). We also aim to assess the prevalence of these pathologies and the corresponding influence of sex and age.
Material and methods
The CBCT scans of patients who attended an appointment at the FMDUP clinic between January 2023 and March 2024 were analyzed. Only cases with at least one impacted M3 were selected.
The FMDUP Ethics Committee for Health and the Responsible for Access to Information approved the project. The anonymity of all participants was maintained throughout the research.
The CBCT scans used the following parameters: 10 mA, 90 kV, 150 μm voxel size, 10 s (localized) or 15 s of exposure time, and a field of view of 40x50 mm (localized), 100x60 mm (maxillary/mandibular), and 100x100 mm (bimaxillary).
The data collected included age, sex, the position of the impacted tooth, and the existence of a pathology. The inclusion criteria were patients 18 years or older who had a CBCT with an impacted M3 without artifacts compromising the accuracy of the analysis. The exclusion criteria were M3 with less than 2/3 of the roots formed, a supernumerary distal to M3, exodontia of M2, or simultaneous impaction of M2 and M3.
A single researcher collected and analyzed the data obtained using the Planmeca Romexis� 4.6.0.R software. The analysis was conducted in three planes (sagittal, coronal, and axial) using images with a thickness of 0.1 mm.
The M3 position was classified according to Winter�s20 and Pell & Gregory�ss21 classifications (Figures 1 and 2). The following pathologies were assessed: ERR, based on irregularity/discontinuity with loss of structure on the root�s distal surface or in the cervical region of the adjacent M2 (Figure 3); carious lesion, based on radiolucency on the M2 distal coronal surfasse with a gap between these two teeth and communication between them and the oral environment (Figure 4); and pathological lesions (Figure 5), such as decreased bone density distal to M3 based on radiolucency with more than 3 mm in diameter or odontogenic tumors/cysts represented by uni or multilocular lesions with distinct borders.
�
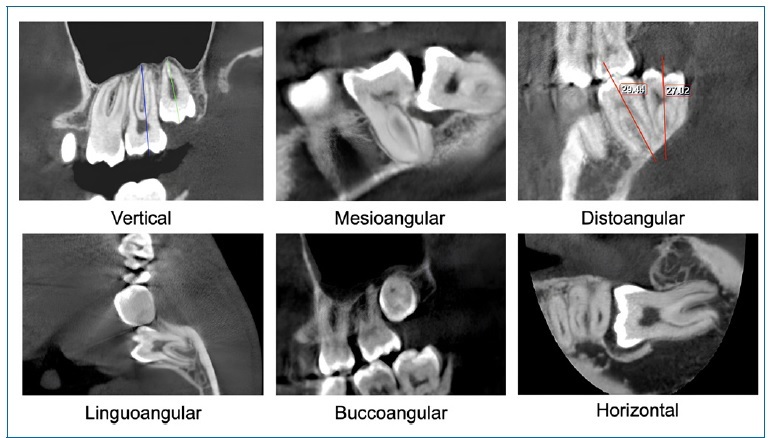
Figure 1. Winter�s classification.
�
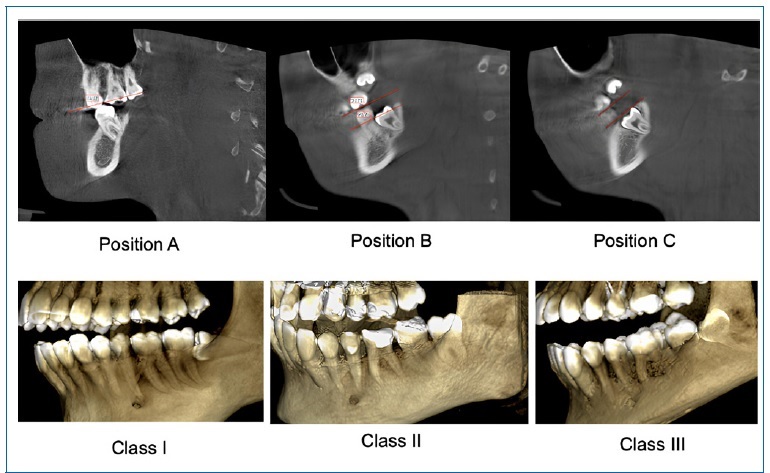
Figure 2. Pell & Gregory�s classification.
�
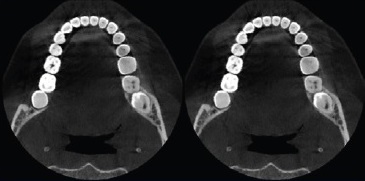
Figure 3. External root resorption (axial section).
�
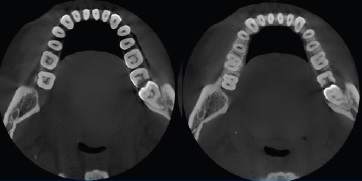
Figure 4. Carious lesion (axial section).
�
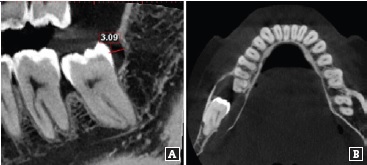
Figure 5. Pathological lesions: A � Decreased bon� density, B � Odontogenic tumor/cyst.
�
Statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS) software, version 29 for Windows. The chi-squared test of independence was used to study the association between the prevalence of the diferente pathologies and sex, age, and M3 position. In cases where at least one of the conditions failed, Fisher�s exact test was used.
A 5% significance level was considered (p<0.05). An intra-evaluator error analysis was conducted on a random sample of 30 teeth selected from the 235 evaluated. The same evaluator repeated these evaluations.
Results
Among a total of 585 CBCT scans evaluated, 382 were excluded due to not including an M3. Of the remaining 203 exams with one or more M3, only 114 had at least one impacted M3 (56.2% impaction rate). Therefore, our sample consisted of 114 patients with a mean age of 30.1 � 12.3 years, corresponding to 235 impacted M3: 137 lower and 98 upper teeth.
Among the impacted M3, 57% had an associated pathology, of which ERR was the most prevalent, occurring in one of three impacted teeth. Due to the small number of patients with odontogenic tumors/cysts (2 patients), this variable was not included in our analysis.
ERR prevalence did not show any association with sex or age. In turn, M2 distal caries showed a statistically significant relation with age (p=0.006), being more prevalent at ages over 30. Decreased bone density distal to M3 was more prevalent in women, without statistical significance (p=0.065).
The overall pathology prevalence depended on the M3 position (p=0.023) according to Winter�s classification, being higher in mesioangular (MA) and linguoangular (LA) teeth.
Although the prevalence of M2 distal caries showed no association with the impacted M3 position, the prevalence of ERR did (p=0.001), being higher in teeth in the MA position. On the other hand, decreased bone density association with position was at the limit of statistical significance (p=0.051). The analysis did not include the horizontal, Linguoangular (LA), and Inverted (I) positions of Winter�s classification due to the small number of cases.
Concerning Pell & Gregory�s classification, the prevalence of three pathologies analyzed was associated with the distance from the occlusal plane (ERR, p<0.001, distal caries of 2nd M, p<0.001 and decrease in bone density, p=0.013). On the other hand, only decreased bone density showed a statistically significant relation (p=0.021) with the distance to the anterior ramus of the mandible.
Regarding measurement error, the results indicate a low error, with high percentages of agreement and Cohen�s kappa values indicating excellent agreement.
Discussion
The literature reports variable M3 impaction rates.22, 23 This study�s impaction rate was 56,2%, agreeing with Bj�rk et al.,24 who estimated a population rate of 55 to 60% with at least one impacted22, 24
The most frequent positions of M3 were MA (Winter�s classification20), Position B, and Class II (Pell & Gregory�s classification21).23, 25 Alsaegh et al.23suggest that rotation to the MA position may result from a less developed mesial root compared to the distal one. Other authors refer to an erratic eruption path resulting from a lack of space in the arch.3, 22
The prevalence of pathology varies according to the M3 position, with a higher incidence associated with the MA position (Winter�s classification<20), as shown by Altan and Akbulut.26 Regarding the Pell & Gregory classification<21, although Ye et al.27 mentioned that teeth in a position closer to the occlusal plane were more likely to cause pathology, our study found no statistically significant relationship between the M3 position and the existence of pathology.
The ERR prevalence obtained (33.2%) aligns with the systematic review by Moreira-Souza et al.,(14) which reports values between 22.8 and 62%.25, 28 Although we concluded that ERR prevalence was not related to sex or age,29, 30 Wang et al.(31) identified the age of 35 or over as a risk factor probably because the eruption process of the M3 does not stop even after rhizogenesis ends, keeping the pressure over time.29, 31
As the average age of this sample was 30.1 years, a young sample, it is understandable that no statistical significance was found.
A statistically significant relationship was found between the MA position and ERR, estimating that a higher contact area between M2 and M3 leads to increased pressure and higher ERR.8, 25 It was also found that ERR depends on the distance from the occlusal plane (more prevalent in Position C), which is in line with the literature, emphasizing that contact points below the cementoenamel junction (CEJ) have a higher risk of ERR. On the other hand, this pathology prevalence was not related to the distance from the anterior ramus of the mandible. Although there is no statistically significant relation, our study�s results align with Haddad et al.,32 who found that Class I was the most frequent in cases of ERR.
Regarding M2 distal caries, this sample found a prevalence of 20.4%, consistent with other studies, which report figures between 7 and 32%. 26, 33 This value depends on oral hygiene literacy, cultural, and socio-economic factors.22, 33, 34 M2 distal caries prevalence is not related to sex,25, 34, 35 but is related to age (over 30 years old). Since carious lesions develop gradually, a higher incidence of this complication has been reported in older patients whose M3 are in an inappropriate position.33,35 Although without statistical significance, dental caries were more prevalent in the MA and LA positions.25, 34, 36, 37 Syed et al.4 state that inappropriate contact points between M2 and M3 promote food impaction and the accumulation of bacterial plaque, especially when these are located below or at the level of the CEJ.27 According to Chen et al.,34 when the M3 is LA, the cusp position further promotes this bacterial accumulation, leading to caries development over time.4
M2 distal caries is more prevalent in Position B teeth, probably due to communication with the oral cavity environment, as deeper positions are surrounded by alveolar bone, preventing contact with the oral cavity microbiota.23, 32 On the other hand, we found that dental caries prevalence was not related to the distance from the anterior ramus of the mandible. This finding contrasts with Alsaegh et al.,23 who reported that this lesion is more prevalent in Classes I and II.
According to the literature, pericoronitis is the main indication for extraction of M3.6, 38 However, in our study, the prevalence of this pathology was 7.2%. This result may derive from our analysis being based exclusively on images, so only cases of severe pericoronitis with repercussions at bone level were considered.38, 40 Pericoronitis prevalence has been reported as sex-dependent, being higher in women, probably due to the early cessation of jaw growth in women, which stops developing roughly when the M3 begins to erupt.41, 42
We found a statistically significant correlation between pericoronitis and the DA position, which aligns with Altan and Akbulut.26 The M3 faces an additional obstacle in this position since the retromolar tissue is more compact than the gengiva tissue found in the normal eruption path41 In contrast, Shirzadeh et al.42 reported that the MA position is also associated with pericoronitis because malposition promotes food impaction, bacterial deposition, and consequently, soft tissue inflammation.
As no clinical assessment was carried out in this study, it is understandable that this relation was not detected. The low prevalence of odontogenic tumors (0.9%) in our study aligns with the literature7, 40 and limits meaningful correlations. The same applied to teeth in the horizontal, Linguoangular (LA), and Inverted (I) positions of Winter�s classification.
Among this study�s limitations is that it was a retrospective study carried out in a reduced sample and restricted to na FMDUP patient population, which may not represent the population in general. Moreover, the analysis was exclusively imaging-based and conducted by a single researcher without collecting clinical history or anamnesis, which can limit the accuracy of the results. It would be important to evaluate a larger and more heterogeneous sample in the future, complementing the imaging analysis with clinical and histological evaluation.
Conclusions
The prevalence of pathology depends on the M3 position according to Winter�s classification: the ERR correlates with the MA position and decreased bone density with the DA position.
There is a significant relationship between Position C and ERR and between the Position B and M2 distal caries, according to Pell & Gregory�s classification. In turn, pericoronitis correlates with Position B and Class II. Age influences the prevalence of M2 distal caries (higher at ages over 30), and sex affects the prevalence of decreased bone density distal to the M3 (higher in females).
�
References
1. Ryalat S, AlRyalat S, Kassob Z, Hassona Y, Al-Shayyab M, Sawair F. Impaction of lower third molars and their association with age: radiological perspectives. BMC Oral Health. 2018;18:58.
2. Santos KK, Lages FS, Maciel CAB, Gl�ria JCR, Douglas-de- Oliveira DW. Prevalence of Mandibular Third Molars According to the Pell & Gregory and Winter Classifications. J Maxillofac Oral Surg. 2022;21:627-33.
3. Smailienė D, Trakinienė G, Beinorienė A, Tutlienė U. Relationship between the Position of Impacted Third Molars and External Root Resorption of Adjacent Second Molars: A Retrospective CBCT Study. Medicina (Kaunas). 2019;55:305.
4. Syed KB, Alshahrani FS, Alabsi WS, Alqahtani ZA, Hameed MS, Mustafa AB, et al. Prevalence of Distal Caries in Mandibular Second Molar Due to Impacted Third Molar. J Clin Diagn Res. 2017;11:ZC28-30.
5. Miliro M, ghali GE, Larsen PE, Waite P editors. Peterson�s Principles of Oral and Maxillofacial Surgery. 4th ed. Cham: Springer Nature Switzerland AG, 2022.
6. Patel PS, Shah JS, Dudhia BB, Butala PB, Jani YV, Macwan RS. Comparison of panoramic radiograph and cone beam computed tomography findings for impacted mandibular third molar root and inferior alveolar nerve canal relation. Indian J Dent Res. 2020;31:91-102.
7. Santosh P. Impacted Mandibular Third Molars: Review of Literature and a Proposal of a Combined Clinical and Radiological Classification. Ann Med Health Sci Res. 2015;5:229-34.
8. Oenning ACC, Neves FS, Alencar PNB, Prado RF, Groppo FC,Haiter-Neto F. External root resorption of the second molar associated with third molar impaction: comparison of panoramic radiography and cone beam computed tomography. J Oral Maxillofacial Surg. 2014;72:1444-55.
9. Oenning ACC, Melo SLS, Groppo FC, Haiter-Neto F. Mesial Inclination of Impacted Third Molars and Its Propensity to Stimulate External Root Resorption in Second Molars � A Cone-Beam Computed Tomographic Evaluation. J Oral Maxillofac Surg. 2015;73:379-86.
10. Le SH, Nguyen NM, Nguyen NT, Nguyen LT. Anatomical Positions of Mesially/Horizontally Impacted Mandibular Third Molars are Significant Predictors for Distal Caries in Adjacent Second Molars. Int J Dent. 2022:2022;8482209.
11. Gl�ria JCR, Martins CC, Armond ACV, Galv�o EL, Dos Santos CRR, Falci SGM. Third Molar and Their Relationship with Caries on the Distal Surface of Second Molar: A Metaanalysis. J Maxillofac Oral Surg. 2018;17:129�41.
12. Schmidt J, Kunderova M, Pilbauerova N, Kapitan M. A Review of Evidence-Based Recommendations for Pericoronitis Management and a Systematic Review of Antibiotic Prescribing for Pericoronitis among Dentists: Inappropriate Pericoronitis Treatment Is a Critical Factor of Antibiotic Overuse in Dentistry. Int J Environ Res Public Health. 2021;18:6796.
13. Wang L, Olmo H. Odontogenic Cysts. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574529/.
14. Moreira-Souza L, Oliveira LB, Ga�ta-Araujo H, Almeida- Marques M, Asprino L, Oenning AC. Comparison of CBCT and panoramic radiography for the assessment of bone loss and root resorption on the second molar associated with third molar impaction: a systematic review. Dentomaxillofac Radiol. 2022;51:20210217.
15. Li D, Tao Y, Cui M, Zhang W, Zhang X, Hu X. External root resorption in maxillary and mandibular second molars associated with impacted third molars: a cone-beam computed tomographic study. Clin Oral Investig. 2019;23:4195-203.
16. Matzen L, Petersen L, Wenzel A. Radiographic methods used before removal of mandibular third molars among randomly selected general dental clinics. Dentomaxillofac Radiol. 2016;45:20150226.
17. Matzen LH, Wenzel A. Efficacy of CBCT for assessment of impacted mandibular third molars: a review - based on a hierarchical model of evidence. Dentomaxillofac Radiol. 2015;44:20140189.
18. Matzen LH, Berkhout E. Cone beam CT imaging of the mandibular third molar: a position paper prepared by the European Academy of DentoMaxilloFacial Radiology (EADMFR). Dentomaxillofac Radiol. 2019;48:20190039.
19. Mendon�a LM, Ga�ta-Araujo H, Cruvinel PB, Tosin IW, Azenha MR, Ferraz EP, et al. Can diagnostic changes caused by cone beam computed tomography alter the clinical decision in impacted lower third molar treatment plan? DentomaxillofacRadiol. 2021;50:20200412.
20. Winter GB. Principles of Exodontia as Applied to the Impacted Mandibular Third Molar: A Complete Treatise on the Operative Technic with Clinical Diagnoses and Radiographic Interpretations. St. Louis: American Medical Book Company, 1926.
21. Pell GJ, Gregory GT. Impacted mandibular third molars: Classification and modified technique for removel. The Dental Digest. 1933;39:330.
22. Skitioui M, Jaoui D, Khalaf LH, Tour� B. Mandibular Second Molars and Their Pathologies Related to the Position of the Mandibular Third Molar: A Radiographic Study. Clin Cosmet Invest Dent. 2023;15:215-23.
23. Alsaegh MA, Abushweme DA, Ahmed KO, Ahmed SO. The pattern of mandibular third molar impaction and its relationship with the development of distal caries in adjacent second molars among Emiratis: a retrospective study. BMC Oral Health. 2022;22:306.
24. Bj�rk A, Jensen E, Palling M. Mandibular growth and third molar impaction. Acta Odontol Scand. 1956;14:231�272.
25. Akkitap MP, Gumru B. Can the Position of the Impacted Third Molars Be an Early Risk Indicator of Pathological Conditions? A Retrospective Cone-Beam Computed Tomography Study. J Oral Maxillofac Res. 2023;14:e3.
26. Altan A, Akbulut N. Does the Angulation of an Impacted Mandibular third Molar Affect the Prevalence of Preoperative Pathoses? J Dent (Shiraz). 2019;20:48-52.
27. Ye Z, Qian W, Wu Y, Yang C. Pathologies associated with the mandibular third molar impaction. Sci Prog. 2021;104:368504211013247.
28. Choi J. Risk factors for external root resorption of maxillary second molars associated with third molars. Imaging Sci Dent. 2022;52:289-94.
29. G�rses G, Ak�akaya A, Aktı A, Aydin O. The effect of impacted third molars on second molar external root resorption, a cross-sectional cone beam computed tomography study. Med Oral Patol Oral Cir Bucal. 2023;28:e504-11.
30. Sakhdari S, Farahani S, Asnaashari E, Marjani S. Frequency and Severity of Second Molar External Root Resorption Due to the Adjacent Third Molar and Related Factors: A Cone-Beam Computed Tomography Study. Front Dent. 2021;18:36.
31. Cui L, Jiang E, Liu Z, Li J. Relationship between the impacted mandibular third molar and adjacent second molar� external root resorption by cone-bean computed tomography analysis. Med Oral Patol Oral Cir Bucal. 2024;29:e27-35.
32. Haddad Z, Khorasani M, Bakhshi M, Tofangchiha M, Shalli Z. Radiographic Position of Impacted Mandibular Third Molars and Their Association with Pathological Conditions. Int J Dent. 2021;2021:8841297.
33. Marques J, Montserrat-Bosch M, Figueiredo R, Vilchez-P�rez M, Valmaseda-Castell�n E, Gay-Escoda C. Impacted lower third molars and distal caries in the mandibular second molar. Is prophylactic removal of lower third molars justified? J Clin Exp Dent. 2017;9:e794-6.
34. Chen Y, Zheng J, Li D, Huang Z, Huang Z, Wang X, et al. Three-dimensional position of mandibular third molars and its association with distal caries in mandibular second molars: a cone beam computed tomographic study. Clin Oral Investig. 2020;24:3265-73.
35. Kang F, Huang C, Sah MK, Jiang B. Effect of Eruption Status of the Mandibular Third Molar on Distal Caries in the Adjacent Second Molar. J Oral Maxillofac Surg. 2016;74:684-92
36. Toedtling V, Coulthard P, Thackray G. Distal caries of the second molar in the presence of a mandibular third molar � a prevention protocol. Br Dent J. 2016;221:297-302.
37. Jin X, Zhang X, Jin C, Xuan Y. Analysis of Factors Related to Distal Proximal Caries on the Distal Surface of the Mandibular Second Molar Induced by an Impacted Mandibular Third Molar. Int J Gen Med. 2021;14:3659-67.
38. Baeza S, C�ceres N, Gonz�lez G, Guzm�n C, Sep�lveda MP, Valenzuela I. Caracterizaci�n de exodoncia de terceros molares. Rev Cient Odontol (Lima). 2021;9:e075.
39. Pe�arrocha-Diago M, Camps-Font O, S�nchez-Torres A, Figueiredo R, S�nchez-Garc�s M, Gay-Escoda C. Indications of the extraction of symptomatic impacted third molars � A systematic review. J Clin Exp Dent. 2021;13:e278-86.
40. Gupta P, Naik SR, Ashok L, Khaitan T, Shukla AK. Prevalence of periodontitis and caries on the distal aspect of mandibular second molar adjacent to impacted mandibular third molar: A guide for oral health promotion. J Family Med Prim Care. 2020;9:2370-4.
41. Singh P, Nath P, Bindra S, Rao SS, Reddy KVR. The predictivity of mandibular third molar position as a risk indicator for pericoronitis: A prospective study. Natl J Maxillofac Surg. 2018;9:215-21.
42. Shirzadeh A, Shirvan SB, Alizadeh O, Grillo R, Vida M, Samieirad S. What is the Most Prevalent Type of Third Molar Impaction in Patients with Pericoronitis? World J Plast Surg. 2023;12:57-63.
�
Sofia Scapini
E-mail address: sofiascapini1@hotmail.com
�
CRediT authorship contribution statement
Sofia Scapini: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing � original draft. Pedro Mesquita: Project administration, Supervision, Validation, Visualization, Writing � review & editing.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
1646-2890/� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
