
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (1) | 38-43
Clinical case
Isolated oral lesions as an uncommon manifestation of secondary syphilis: A clinical case
Lesões orais isoladas como manifestação incomum de sífilis secundária: Caso clínico
a Faculty of Dentistry, University of Passo Fundo, Passo Fundo, Brazil
b Family Health Strategy of the Municipality of Nova Prata, Nova Prata, Brazil
c Faculty of Dentistry, Federal University of Santa Catarina, Florianópolis, Brazil
Felipe Gomes Dallepiane - dallepianefe@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 1
Clinical case
Pages - 38-43
Go to Volume
Article History
Received on 16/09/2023
Accepted on 10/02/2025
Available Online on 31/03/2025
Keywords
Clinical Case Report
�
Isolated oral lesions as an uncommon manifestation of secondary syphilis: A clinical case
Les�es orais isoladas como manifesta��o incomum de s�filis secund�ria: Caso cl�nico
�
Julia Zandon�1 0000-0002-9816-0293
Sandro Adail Alves2 0000-0002-1035-5820
Dicleia Marzzaro Ossani2 0009-0008-7054-9652
Let�cia Copatti Dogenski1 0000-0001-6174-5485
Felipe Gomes Dallepiane3,* 0000-0001-9677-9984
Jo�o Paulo De Carli1 0000-0002-4705-6226
1Faculty of Dentistry, University of Passo Fundo, Passo Fundo, Brazil.
2 Family Health Strategy of the Municipality of Nova Prata, Nova Prata, Brazil.
3 Faculty of Dentistry, Federal University of Santa Catarina, Florian�polis, Brazil.
�
�
Article history:
Received 16 September 2023
Accepted 10 February 2025
Available online 21 March 2025
�
Abstract
This study aims to report a clinical case of an isolated oral manifestation of secondary syphilis. A Caucasian 30-year-old female patient presented to a public oral health servisse in Southern Brazil, complaining of symptomatic oral ulcerative lesions without spontaneous regression for over 30 days. Intraoral examination revealed a larger lesion in the central region of the hard palate with confluent mucous plaques, resulting in "slug-shaped ulcers" surrounded by erythema, and smaller mucous patches with irregularly shaped, whitish fibrinous pseudomembranes in the region of the lower vestibular sulcus, near teeth 41, 42, 33, and 34. Rapid syphilis and VDRL tests confirmed Treponema pallidum contamination (titer 1:128). After 3 weeks of treatment with Penicillin G Benzathine, the clinical signs and titers significantly decreased. This case report underscores the importance of integrating and continually incorporating oral health care into public health, as dentists can diagnose and monitor many systemic diseases with repercussions in the oral cavity.
Keywords: Diagnosis, Syphilis, Treatment outcome, Treponema pallidum, VDRL antigen
�
Resumo
O objetivo deste estudo � relatar um caso cl�nico de manifesta��o oral isolada de s�filis secund�ria. Paciente do sexo feminino, cau- 42 rev port estomatol med dent cir maxilofac . 2025;66(1):38-43 casiana, 30 anos de idade, compareceu ao servi�o p�blico de sa�de no Sul do Brasil, com queixa de les�es ulcerativas orais sintom�ticas sem regress�o espont�nea, surgidas h� mais de 30 dias. Ao exame intraoral, diagnosticou-se les�o maior na regi�o central do palato duro com placas mucosas confluentes criando ��lceras em forma de lesma� circundadas por eritema, e manchas mucosas menores com pseudomembranas fibrinosas esbranqui�adas de formato
irregular na regi�o do sulco vestibular inferior, pr�ximas � localiza��o dos dentes 41, 42, 33 e 34. Os testes r�pido para s�filis e VDRL confirmaram contamina��o por Treponema pallidum (titula��o 1:128). Ap�s 3 semanas de tratamento com penicilina G Benzatina, os sinais cl�nicos e a titula��o diminu�ram significativamente. O presente relato evidencia a import�ncia da integra��o e inser��o cont�nua dos cuidados de sa�de oral no contexto da sa�de p�blica, visto que o cirurgi�o-dentista pode diagnosticar e acompanhar muitas doen�as sist�micas com repercuss�o na cavidade oral.
Palavras-chave: Diagn�stico, S�filis, Tratamento, Treponema pallidum, Antig�neo VDRL
�
Introduction
Syphilis is a sexually transmitted disease caused by Treponema pallidum,1 a helical anaerobic bacterial species.2, 3 It represents a significant public health issue worldwide, with more than 6 million estimated new cases of syphilis each year and severe health consequences if left untreated.4, 5, 6, 7 Brazil is experiencing a significant increase in syphilis cases compared to other Latin American countries, following a trend contrary to the eradication goal.8, 9 This increase may be related to the compulsory notification throughout the country in force since 2010,10 and the reduction in condom use.11 This is a significant risk to public health and underscores the importance of prioritizing investments in prevention and promotion that target Health Care Networks, especially for improving the quality of care provided to populations engaging in risky behaviors.9
Syphilis can have various clinical manifestations and progresses through four different stages with varying levels of activity and infectivity: primary, secondary, latent, and tertiary syphilis.5 The typical lesion of primary syphilis consists of a frequently single, painless, and non-pruritic cutaneous ulceration called a �chancre,� which appears at the site of inoculation approximately three weeks after exposure and may be associated with regional lymphadenopathy, both of which resolve spontaneously.10 The secondary stage results from hematogenous and lymphatic dissemination of treponemes, usually causing mucocutaneous and systemic manifestations six to eight weeks after the initial infection.3, 12 In secondary syphilis, the manifestations are more heterogeneous and nonspecific.13 Primary and secondary lesions can resolve spontaneously, and the infection enters a latent stage that can persist for years. Then, the disease may progress to the tertiary stage, in which a range of late manifestations might lead to destructive neurological and cardiovascular complications, severe skin or visceral lesions (gummas), or bone involvement.4, 5
Syphilis can exhibit pathognomonic signs in the oral cavity in different stages.14 However, multiple oral lesions are more commonly seen in secondary syphilis. Among its clinical oral manifestations, the most common are described as �mucous patches� or �macules� and may appear as slightly elevated, usually oval-shaped plaques, occasionally ulcerated, covered by a grayish or whitish fibrinous pseudomembrane.2, 3, 15, 16
Another manifestation consists of multiple mucous patches that can coalesce, giving rise to serpiginous lesions described as �slug track ulcers.�3, 17, 18 Syphilitic lesions of the oral mucosa are often associated with systemic and cutaneous manifestations, and exclusive oral involvement is quite uncommon in secondary syphilis.15, 17, 18
This study aimed to report a clinical case of an isolated oral manifestation of secondary syphilis diagnosed in a public oral health service, confirmed by treponemal and non-treponemal serological tests.
Case Report
The patient provided written consent for the publication of her clinical case in accordance with the Declaration of Helsinki by signing an informed consent form prior to the drafting of this study.
A Caucasian 30-year-old female patient sought medical attention at a public health service in Southern Brazil, complaining of symptomatic oral ulcerative lesions that did not show spontaneous regression. After clinical evaluation, treatment with triamcinolone acetonide 1 mg/g for 7 days was prescribed due to suspicion of aphthous ulcers. The patient returned five days later seeking dental services, reporting the lack of lesion regression and persistent painful symptoms. During the dental consultation, the clinical history of the lesions was thoroughly investigated for differential diagnosis.
The patient reported that the oral manifestations had first presented at least 30 days previously and were initially asymptomatic before becoming symptomatic. She reported no other skin or genital lesions and no systemic manifestations such as fever, sore throat, or lymphadenopathy.
Intraoral clinical examination diagnosed a larger lesion in the central region of the hard palate with confluent mucous plaques, giving rise to �slug-shaped ulcers� surrounded by erythema (Figure 1). Smaller mucous patches with irregularly shaped, whitish fibrinous pseudomembranes were identified in the region of the lower vestibular sulcus near teeth 41, 42, 33, and 34 (Figure 2). Another larger mucous patch with na irregular appearance and coalescence, slightly elevated with a whitish fibrinous pseudomembrane and surrounded by erythema, was detected in the central region of the lower labial mucosa (Figure 3).
�
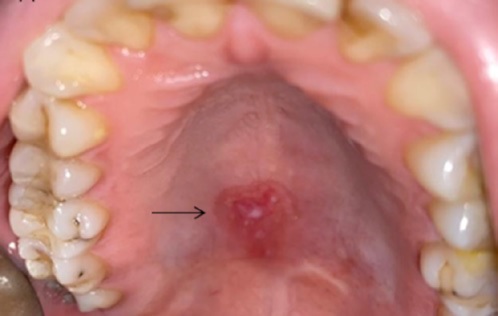
Figure 1. Larger lesion in the central region of the hard palate with confluent mucous plaques, giving rise to �slug-shaped ulcers� surrounded by erythema.

Figure 2. Smaller mucous patches with irregularly shaped white fibrinous pseudomembranes in the lower vestibular sulcus near teeth 41 and 42 and teeth 33 and 34.

Figure 3. Larger mucous patch with an irregular appearance and coalescence, slightly elevated with white fibrinous pseudomembrane and surrounded by erythema in the central region of the lower labial mucosa.
Upon suspicion of syphilitic oral lesions and for differential diagnosis, rapid tests were requested and performed by the nursing service at the healthcare unit. The results showed a reactive test for syphilis (treponemal serological test VDRL) and non-reactive results for other rapid screening tests (HIV, hepatitis C, and hepatitis B). After confirming the diagnosis, the patient was referred to the medical service for treatment with Penicillin G Benzathine 2.4 million IU, administered via intramuscular injection once a week for three weeks. The diagnostic VDRL test showed a titer of 1:128.
Dental follow-up was conducted to observe the regression of oral manifestations during the treatment period (Figures 4 and 5) and 15 days after the last dose of antibiotic therapy, when complete regression of oral manifestations was observed (Figures 6 and 7). After completing the treatment with Penicillin G Benzathine, a new VDRL test showed a titer of 1:16. A drop in titer from 1:128 to 1:16 after the treatment period indicates treatment success since a four-fold or higher change in titer, equivalent to a change of at least two dilutions, is considered a significant difference between two sequential tests.19
�
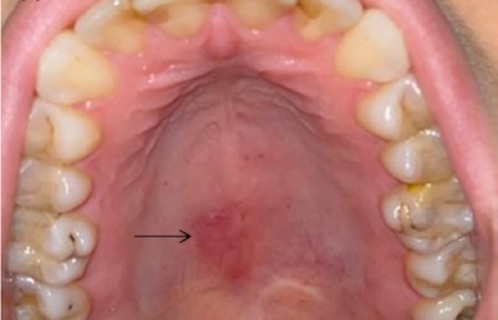
Figure 4. Partial regression of the larger lesion in the central region of the hard palate 14 days after starting treatment with Penicillin G Benzathine.
�

Figure 5. Complete regression of the larger mucous patch in the central region of the lower labial mucosa 14 days after starting treatment with Penicillin G Benzathine.
�

Figure 6. Complete regression of the larger lesion in the central region of the hard palate 30 days after starting treatment with Penicillin G Benzathine.
�

Figure 7. Complete regression of the larger mucous patch in the central region of the lower labial mucosa 30 days after starting treatment with Penicillin G Benzathine.
�
Discussion and Conclusions
This case report emphasizes the importance of paying attention to oral manifestations of syphilis, especially to the clinical differential diagnosis of this disease, which may initially have an uncertain etiology. Moreover, the possibility of isolated oral manifestations should be considered in the absence of other systemic signs or symptoms. Delayed diagnosis of syphilis can lead to disease progression to the latent and tertiary stages, potentially causing more severe and sometimes fatal consequences.20 It is important to consider that syphilitic lesions can be confused with other diseases as they can mimic various conditions and have significantly variable manifestations. The differential diagnosis of syphilis includes, for example, lichen planus, eosinophilic ulcers, traumatic ulcers, leukoplakia, HIV, gonorrhea, necrotizing sialometaplasia, and squamous cell carcinoma.21
In the present case, the suspicion of a syphilitic lesion arose from the lesions� clinical appearance, consistent with what is normally seen in these cases, namely, prolonged (over four weeks) erythematous macules and plaques in lips, tongue, gums, or tonsils. Although the patient did not report other skin or genital lesions or systemic manifestations such as fever, sore throat, or lymphadenopathy, the VDRL test was conducted. This test is available in the public health network in Brazil and is always recommended when syphilis is suspected, such as in the case of a small painless wound, swelling in the lymph nodes near the wound, or skin rashes that do not cause itching.
Before the discovery of penicillin, syphilis was a public health problem controlled for decades with the use of antibiotics.7, 22 However, considering the current increasing incidence of syphilis,23 it is of utmost importance to discuss the dentist�s knowledge and experience for the differential diagnosis of lesions affecting the oral cavity. Awareness is especially important when the only manifestation is oral ulcers, as in the present case, making the differential diagnosis and the possible etiological origin of these lesions more challenging.
The oral manifestations of syphilis can occur in all three stages of the disease, as described earlier. In secondary syphilis, the lesions are usually multiple and more diverse,11 but a single lesion can often be the only manifestation of the disease,21 more commonly presenting as mucous patches, papules, or ulcerations with erosive areas.3, 16, 21 Such reports corroborate the findings of the present case, where multiple ulcerated lesions with diverse characteristics were observed.
The Unified Health System, a Brazilian public health policy, advocates for the prevention of Treponema pallidum contamination and provides free diagnosis and treatment to the population.24 Treponemal tests, such as the rapid syphilis test, and non-treponemal tests, such as VDRL, are available through the Unified Health System and, due to being quick and low-cost, are widely used for screening and disease detection. The rapid test is easier to perform since it is available in Unified Health System Primary Care for sexually transmitted disease screening, and it is reactive in the secondary and latent stages, although it is less sensitive in primary syphilis.25 Serosurvey tests, in conjunction with a well-conducted clinical examination and diagnosis, play a crucial role in diagnosing syphilis.26 Accordingly, in this case, after conducting a differential clinical diagnosis during the dental consultation, serological testing for syphilis was immediately performed, confirming the diagnosis and expediting treatment onset.
This case report emphasizes the need for effective integration and interdisciplinary collaboration within healthcare teams, particularly within public health. The relationship between oral and systemic health is well-documented in the literature, highlighting that the exchange of diagnoses between dental and medical professionals plays a crucial role in the early identification of health issues.
Additionally, it is important to underscore that the rising number of new syphilis cases relates to the social and behavioral aspects of society,21 namely, risky sexual behavior such as reduced safe sexual practices, which is the primary reason for this resurgence.25 This situation highlights the urgent need for public health education measures or campaigns, especially in the affected countries.
This case report emphasizes the importance of integrating and incorporating oral health into the public health context. Moreover, it reflects the importance of updating and continuously training health professionals, as many systemic diseases have oral manifestations that can be diagnosed and monitored by dentists. Additionally, the multidisciplinary approach of public health teams is essential for comprehensive healthcare coverage for patients.
�
References
1. van Staden SM, de Villiers C, Alwan J, Moloi M, Mahlangu S. Oral manifestations of syphilis: Report of four cases. Pathogens. 2022;11:612.
2. De Paulo LFB, Servato JPS, Oliveira MTF, Durighetto Jr AF, Zanetta-Barbosa D. Oral manifestations of secondary syphilis. Int J Infect Dis. 2015;35:40-2.
3. Mari E, Nudo M, Palese E, Cotticelli L, Cotticelli C, Zino G, et al. Beyond appearance: An unusual manifestation of isolated oral secondary syphilis. Int J Immunopathol Pharmacol. 2019;33:2058738419845566.
4. Hook III EW, Peeling RW. Syphilis control - a continuing challenge. N Engl J Med. 2004;351:122-4.
5. Zoni AC, Gonzalez MA, Sjoegren HW. Syphilis in the most at-risk populations in Latin America and the Caribbean: a systematic review. Int J Infect Dis. 2013;17:e84-92.
6. Newman L, Rowley J, Hoorn SV, Wijesooriya NS, Unemo M, Low N, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PloS One. 2015;10:e0143304.
7. Chen T, Wan B, Wang M, Lin S, Wu Y, Huang J. Evaluating the global, regional, and national impact of syphilis: results from the global burden of disease study 2019. Sci Rep. 2023;13:11386.
8. Silveira MF, de Leon RGP, Becerra F, Serruya SJ. Evolution towards the elimination of congenital syphilis in Latin America and the Caribbean: a multicountry analysis. Ver Panam Salud P�blica. 2019;43:e31.
9. dos Santos MM, Lopes AKB, Roncalli AG, Lima KCD. Trends of syphilis in Brazil: a growth portrait of the treponemic epidemic. PloS One. 2020;15:e0231029.
10. Minist�rio da Sa�de do Brasil. Semin�rio apresenta projeto �Resposta r�pida � s�filis nas redes de aten��o� a profissionais de sa�de Available from: https://antigo.aids.gov.br/pt-br/noticias/seminario-apresenta-projeto-respostarapida-sifilis-nas-redes-de-atencao-profissionais-de. Accessed 16 September, 2023.
11. Stover J, Rosen JE, Carvalho MN, Korenromp EL, Friedman HS, Cogan M, et al. The case for investing in the male condom. PLoS One. 2017;12:e0177108.
12. Peeling RW, Mabey D, Kamb ML, Chen XS, Radolf JD, Benzaken AS. Syphilis. Nat Rev Dis Primers. 2017;12:17073.
13. Pires FR, Da Silva PJS, Natal RF, Alves FA, Pinto CAL, Rumayor A, et al. Clinicopathologic features, microvessel density, and immunohistochemical expression of ICAM-1 and VEGF in 15 cases of secondary syphilis with oral manifestations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121:274-81.
14. Meseli SE, Pelit S. Syphilis and dentists: The data about knowledge and awareness of clinicians in Turkey. Int J STD AIDS. 2023;34:408-15.
15. Aquilina C, Viraben R, Denis P. Secondary syphilis simulating oral hairy leukoplakia. J Am Acad Dermatol. 2003;49:749-51
16. de Andrade RS, de Freitas EM, Rocha BA, J�nior HM. Oral findings in secondary syphilis. Med Oral Patol Oral Cir Bucal. 2018;23:e138.
17. Carlesimo M, Palese E, Mari E, Feliziani G, La Pietra M, De Marco G, et al. Isolated oral erosions: an unusual manifestation of secondary syphilis. Dermatol Online J. 2008;14:23.
18. Liu XK, Li J. Secondary syphilis-related oral mucous patches. IDCases, 2017;9:34-5.
19. World Health Organization. WHO guidelines for the treatment of Treponema pallidum (syphilis). Geneva: WHO Document Production Services, 2016. p.12
20. Udd SD, Lund B. Oral syphilis: A reemerging infection prompting clinicians� alertness. Case Rep Dent. 2016;2016:6295920.
21. Matias MDP, Jesus AO, Resende RG, Caldeira PC, Aguiar MCF. Diagnosing acquired syphilis through oral lesions: The 12 year experience of an Oral Medicine Center. Braz J Otorhinolaryngol. 2020;86:358-63.
22. Neto BG, Soler ZASG, Braile DM, Daher W. A siflis no s�culo XVI- o impacto de uma nova doen�a. Arq Cienc Sa�de. 2009;16:127-9.
23. Ditzen AK, Braker K, Zoellner KH, Teichmann D. The syphilis-HIV interdependency. Int J STD AIDS. 2005;16:642-3.
24. Lazarini FM, Barbosa DA. Educational intervention in Primary Care for the prevention of congenital syphilis. Rev Lat Am Enfermagem. 2017;25:e2845.
25. Cohen SE, Klausner JD, Engelman J, Philip S. Syphilis in the modern era: An update for physicians. Infect Dis Clin North Am. 2013;27:705-22.
26. Ficarra G, Carlos R. Syphilis: The renaissance of an old disease with oral implications. Head Neck Pathol 2009;3:195-206.
�
Felipe Gomes Dallepiane
E-mail address: dallepianefe@gmail.com
�
CRediT authorship contribution statement
Julia Zandon�: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, administration, Resources, Supervision, Validation, Visualization, Writing � original draft; Writing � revision & editing. Sandro Adail Alves: Conceptualization, Data curation, Methodology, Project administration, Supervision, Validation, Writing � original draft, Writing � revision & editing. Dicleia Marzzaro Ossani: Conceptualization, Data curation, Methodology, Supervision, Validation; Writing � original draft; Writing � revision & editing. Let�cia Copatti Dogenski: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Supervision, Validation, Visualization, Writing � original draft, Writing � revision & editing. Felipe Gomes Dallepiane: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing � original draft, Writing � revision & editing. Jo�o Paulo De Carli: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing � original draft, Writing � revision & editing.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. Th
�
Acknowledgements
Julia Zandon� and Let�cia Copatti Dogenski are CAPES 1 scholarship holders.
�
� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria.
Published by SPEMD. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
