
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2025 | 66 (1) | 31-37
Clinical case
Report of two rare cases of plasma cell granuloma of the gingiva
Relato de dois casos raros de granuloma de células plasmocitárias da gengiva
a Postgraduate Program in Dental Sciences, Department of Dentistry, Federal University of Rio Grande do Norte, Natal, RN, Brazil
b Federal University of Rio Grande do Norte, Natal, RN, Brazil
c Private practice, Natal, RN, Brazil
Roseana de Almeida Freitas - roseanafreitas@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 66
Issue - 1
Clinical case
Pages - 31-37
Go to Volume
Article History
Received on 18/04/2024
Accepted on 08/02/2025
Available Online on 31/03/2025
Keywords
Clinical Case Report
�
Report of two rare cases of plasma cell granuloma of the gengiva
Relato de dois casos raros de granuloma de c�lulas plasmocit�rias da gengiva
�
Hannah Gil de Farias Morais1 0000-0003-3488-3465
Renata Roque Ribeiro1 0000-0002-1685-8955
Jos� Nazareno Moreira de Aguiar J�nior2 0000-0002-8305-2572
Victor Diniz Borborema dos Santo3 0000-0002-5924-9543
Hevio Freitas de Lucena2 0009-0005-3052-3261
Roseana de Almeida Freitas1,* 0000-0002-7577-5375
1Postgraduate Program in Dental Sciences, Department of Dentistry, Federal University of Rio Grande do Norte, Natal, RN, Brazil.
2Federal University of Rio Grande do Norte, Natal, RN, Brazil.
3Private practice, Natal, RN, Brazil.
�
�
Article history:
Received 18 April 2024
Accepted 8 February 2025
Available online 21 March 2025
�
Abstract
Plasma cell granuloma is a rare benign, occasionally aggressive lesion with an unclear etiopathogenesis characterized by plasma cell infiltration. It occurs mainly in the lungs but can also affect the liver, kidneys, brain, and heart. Its occurrence in the oral cavity is rare. In this study, we report two rare cases of plasma cell granuloma involving the maxillary gengiva in a middle-aged male patient and a pregnant woman. In both cases, the lesion appeared red and bleeding. Following excisional biopsy, the specimens were subjected to histopathological analysis and immunohistochemical confirmation, leading to a diagnosis of plasma cell granuloma. Both patients are under monitoring and show no signs of recurrence.
The authors also discuss plasma cell granuloma�s clinical, histopathological, and immunohistochemical features. Histopathological examination and complementary immunohistochemistry are crucial for its correct diagnosis. Despite its benign behavior, plasma cell granuloma�s local aggressiveness, rarity in the oral cavity, and similarity with other benign and malignant lesions of the gingiva make its diagnosis difficult.
Keywords: Case reports, Gingiva, Plasma cell granuloma, Plasma cells
�
Resumo
O granuloma de c�lulas plasmocit�rias � uma les�o benigna rara, ocasionalmente agressiva, com etiopatogenia obscura, caracterizada pela infiltra��o de c�lulas plasm�ticas. Ocorre principalmente nos pulm�es, mas tamb�m pode afetar o f�gado, os rins, o c�rebro e o cora��o. A sua ocorr�ncia na cavidade oral � rara. Neste estudo, relatamos dois casos raros de granuloma de c�lulas plasmocit�rias envolvendo a gengiva maxilar num paciente do sexo masculino de meia-idade e numa mulher gr�vida. Em ambos os casos, a les�o apresentava-se avermelhada e sangrante. Ap�s a bi�psia excisional, os esp�cimes foram submetidos a an�lise histopatol�gica e confirma��o imuno-histoqu�mica, levando ao diagn�stico de granuloma de c�lulas plasm�ticas. Ambos os pacientes est�o sob acompanhamento e n�o demonstraram sinais de recidiva.
Os autores tamb�m discutem as caracter�sticas cl�nicas, histopatol�gicas e imuno-histoqu�micas. O exame histopatol�gico e a imunohistoqu�mica complementar s�o cruciais para o correto diagn�stico do granuloma de c�lulas plasmocit�rias. Apesar do seu comportamento benigno, a agressividade local do granuloma de c�lulas plasmocit�rias, a sua raridade na cavidade oral e o facto de poder mimetizar outras les�es benignas e malignas da gengiva dificultam o diagn�stico desta les�o.
Palavras-chave: Relatos de caso, Gengiva, Granuloma de c�lulas plasm�ticas, C�lulas plasm�ticas
�
Introduction
Plasma cell granuloma (PCG), also known as inflammatory pseudotumor, was first described by Bhaskar, Levin, and Frisch in 1968.1 The lungs and airways are the most commonly affected sites, but the involvement of extrapulmonary sites such as skin, brain, and oral cavity has also been reported. In the oral cavity, PCG can affect the tongue, lips, cheek mucosa, and gingiva.2 3 However, few cases have been documented so far.1
Although PCG etiopathogenesis remains unknown, some authors have suggested that it arises from a hyperreactive response to idiopathic allergens/antigens, long-standing periodontitis, and periradicular inflammation.4 - 6
Clinically, intraoral PCG appears as an asymptomatic, exophytic, and nodular lesion with a relatively smooth surface. Nevertheless, it may be ulcerated due to trauma and present bleeding on touch in some cases. It has no gender or age predilection.5, 6 Although PCG appears to be benign and non-recurrent, bone resorption, local aggressiveness, and recurrences have been reported, which can simulate malignancy and represent a diagnostic challenge.6 Thus, histopathological examination is necessary for diagnostic confirmation.7, 8 Histopathologically, PCG is characterized by dense infiltration of plasma cells in the subepithelial region.5 Its treatment consists of surgical excision and vigorous scraping of the area. The prognosis is usually favorable, and recurrence is uncommon. However, continuous monitoring of the patient is essential.8, 9
Studies on PCG in the oral cavity are still scarce. Therefore, further discussion about this lesion is necessary to better understand its etiology, natural history, and epidemiology.
This knowledge will enable careful and confirmatory diagnoses and, consequently, accurate prognosis prediction and management of the disease. The present article aims to report two cases of PCG in the oral cavity and provide an update of the literature.
Case report
Case 1
A 42-year-old male patient was referred for evaluation of a 2-year slow-growing, reddish, nodular lesion with ulcerated areas that measured approximately 5 cm in its largest point and was located in the gingival mucosa adjacent to teeth 15,16, and 17 (Figure 1). The patient reported no pain but complained of difficulty in performing oral hygiene.
�

Figure 1. Clinical appearance of the lesion. Reddish nodules with ulcerative areas measuring approximately 5 cm in their largest point, located in the gingival mucosa adjacent to teeth 15, 16, and 17.
�
The patient�s medical history was noncontributory, and he was not using any medication. Radiographic analysis revealed horizontal and vertical bone resorption in the lesion area, as well as displacement of teeth 15 and 16 and grade III mobility of tooth 17. Given the clinical characteristics, the diagnostic hypotheses were peripheral ossifying fibroma and pyogenic granuloma.
An excisional biopsy was performed using the elliptical technique, with a 3 mm safety margin around the lesion, followed by second molar removal during the same procedure (Figure 2). A #15 scalpel was used for the incision, with adjacente bone curettage to ensure complete removal of the affected tissue. The procedure was completed with a simple resorbable suture. In the postoperative period, the patient was prescribed 1 g of dipyrone every 6 hours as needed for pain relief. A 0.12% chlorhexidine mouthwash was recommended twice daily for 7 days.
�
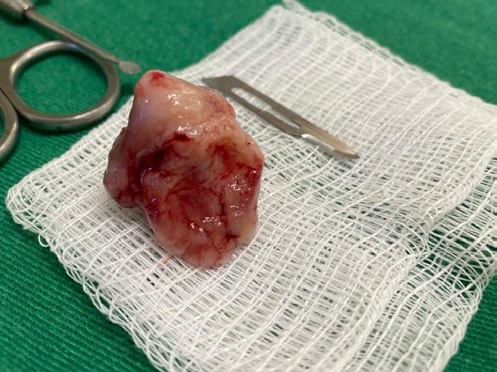
Figure 2. Macroscopic inspection of the surgical specimen measuring approximately 4.5 cm in its largest diameter.
�
The excised material was sent for histopathological analysis, which revealed a fragment of oral mucosa with abundant plasma cells and some Russell bodies in the connective tissue (Figures 3 and 4). Dense bundles of interlaced collagen fibers were also prominent, interspersed with loosely organized fibrous tissue areas. Additionally, the analysis detected moderate vascularization, with vessels of varying calibers, many of which appeared congested. The inflammatory infiltrate was particularly prominent in the subepithelial region, supporting the diagnostic hypothesis of PCG.
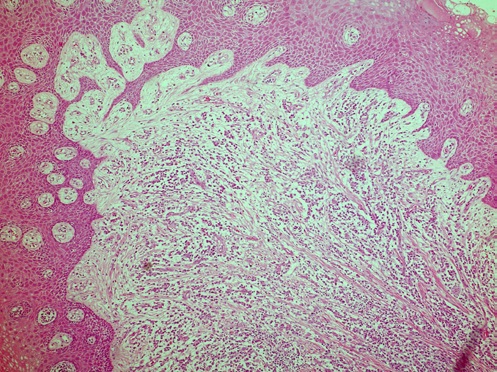
Figure 3. Photomicrograph at lower magnification showing oral mucosa�s loosely organized connective tissue with an intense and diffuse inflammatory infiltrate (H&E, 100X).
�
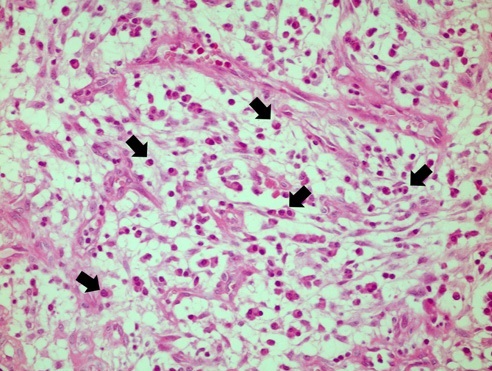
Figure 4. Marked presence of plasma cells (arrows) (H&E, 400X).
�
The tissue was then submitted to immunohistochemical analysis of kappa (κ) and lambda (λ) light chains for diagnostic confirmation and differentiation of reactive and lymphoproliferative lesions. It revealed strong and diffuse cytoplasmic positivity for both chains, with the κ chain being more abundant (Figures 5 and 6). The immunohistochemical results suggested polyclonal proliferation of plasma cells and confirmed the histopathological findings.
�
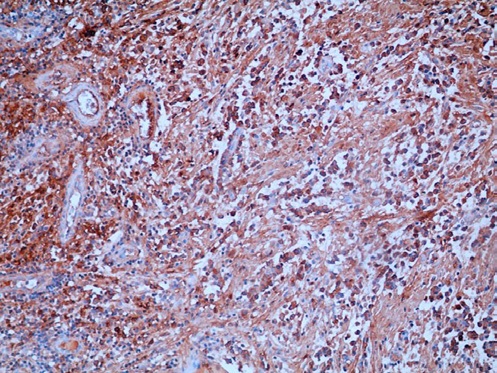
Figure 5. Immunohistochemical findings showing strong positivity for κ light chains (200X).
�
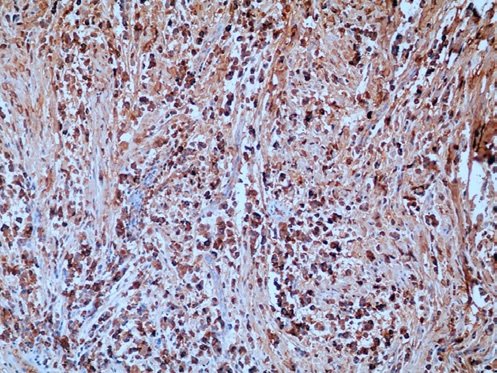
Figure 6. Immunohistochemical findings showing strong positivity for λ light chains (200X).
�
The clinical, histopathological, and immunohistochemical findings indicated the final diagnosis of PCG. The patient has been under follow-up for 2 years and shows no signs of clinical or radiographic recurrence.
Case 2
A 24-year-old, five-month pregnant woman attended an oral diagnostic service complaining of a bleeding lesion on her gengiva that had appeared a few months earlier. During anamnesis, she reported no systemic changes or medication use. Intraoral examination revealed a reddish lesion of soft consistency located in the upper gingiva between the central incisor (tooth 21) and the mesial part of the canine (tooth 13).
The lesion measured approximately 2 cm. A nodular mass was also detected between teeth 11 and 12 (Figure 7). The patient used fixed orthodontic appliances but denied regular maintenance visits with her orthodontist. Periapical radiography revealed no bone alterations in the region.
�

Figure 7. Clinical aspect of the lesion. Reddish, shiny, exophytic lesion between teeth 21 and 13, highlighting a small nodule in the interproximal gingiva between teeth 11 and 12.
�
A clinical diagnosis of pyogenic granuloma was hypothesized. Thus, an excisional biopsy was performed using the elliptical technique, with a 3-mm safety margin around the lesion to ensure complete removal of the affected tissue. Careful curettage of the surgical area was performed to eliminate any potential lesion remnants, thereby reducing the risk of recurrence. The surgical approach was discussed and approved in advance by the patient�s attending obstetrician, ensuring the safety of both the patient and the fetus during the procedure.
The excised tissue sample was then sent for histopathological analysis. In the postoperative period, the patient was prescribed 500 mg of paracetamol every 6 hours as needed for pain relief, with guidance to avoid the use of other analgesics without medical recommendation. A 0.12% chlorhexidine mouthwash twice daily for 7 days was advised.
The histopathological findings revealed a fragment of oral mucosa whose fibrous connective tissue of varying density exhibited dense bundles of intertwined collagen fibers permeated by areas of loosely organized fibrous tissue containing numerous plasma cells and exuberant vascularization (Figure 8). Immunohistochemistry was conducted for diagnostic confirmation and revealed a polyclonal pattern and mixed populations of the κ (Figure 9) and λ (Figure 10) light chains. Thus, the final diagnosis was PCG, and follow-up was recommended. The patient has shown no signs of recurrence for 6 months.
�
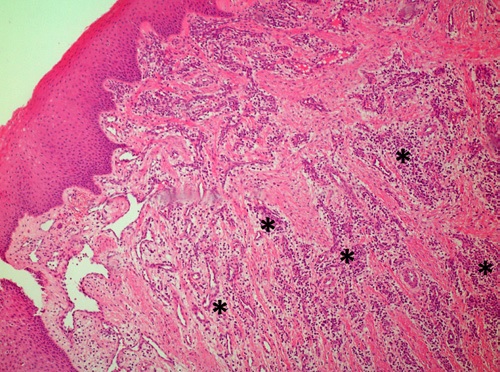
Figure 8. Histopathological features. At lower magnification, a fragment of oral mucosa containing dense bundles of intertwined collagen fibers can be seen permeated by areas of loosely organized connective tissue. Numerous plasma cells can be observed in more loose areas (arrows) (H&E, 100X).
�
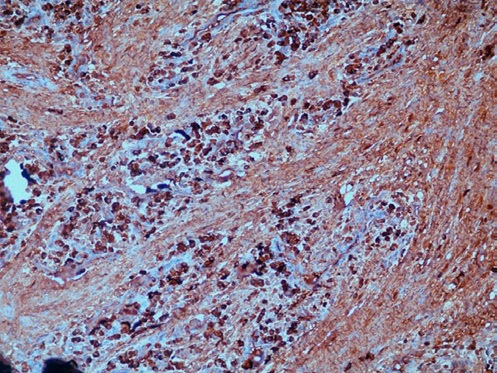
Figure 9. Immunohistochemical findings showing strong positivity for κ light chains (200X).
�
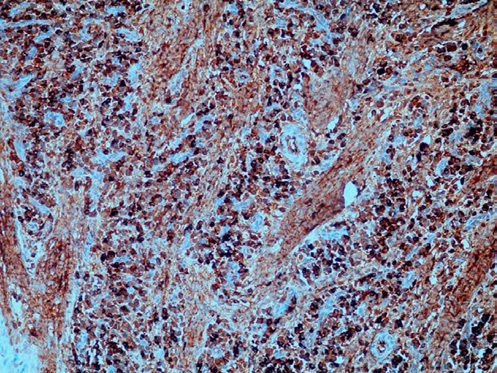
Figure 10. Immunohistochemical findings showing strong positivity for λ light chains (200X).
�
Discussion and conclusions
Different names have been attributed to PCG, such as inflammatory pseudotumor, inflammatory myofibro-histiocytic proliferation, and xanthomatous pseudotumor.4, 10 This lesion occurs most commonly in the lungs, with the head and neck region accounting for less than 5% of all extrapulmonary cases.11 In the latter, the orbit is the most commonly affected site, followed by the meninges, paranasal sinuses, infratemporal fossa, and soft tissues.
PCG can also occur in the oral cavity, with the gingiva being the most commonly affected site,10, 12 as demonstrated in the two cases reported here. Table 1 summarizes the main clinical data of cases diagnosed as PCG in the oral cavity over the past 10 years. All of these cases involved the gingiva, with a predilection for the upper gingiva (7:2). One case had multiple oral lesions in the upper and lower gingiva.8
The pathogenesis of PCG is still uncertain. Some authors suggest the lesion is reactive and associated with a foreign antigen such as EBV and HHV8, periodontitis, periradicular inflammation secondary to the presence of a foreign body, or abundant biofilm/dental calculus caused by poor oral hygiene.5, 11, 13 Drug-induced gingival growth is not uncommon, and medications such as antiepileptics, calcium channel blockers, and immunosuppressants are known to cause gingival hyperplasia.14 One such drug cited in gingival PCG cases reported in the literature is amlodipine.4, 8 Studies have suggested a multifactorial etiology of amlodipine-induced PCG, highlighting drug/cell interactions as a possible mechanism.4, 13
Another etiological factor associated with PCG development is the influence of hormones such as progesterone and estrogen, whose role in gingival overgrowth is well documented.8 Elevated circulating levels of these hormones in the blood are observed during puberty and pregnancy.8 The pregnant patient case reported here shows a temporal association with the case reported in 2022 by Albert et al.8 on a patient who underwent estrogen therapy for infertility, with the very rare occurrence of gingival PCG. These findings are consistent with the fact that middle-aged women with a mean age of 42.4 years are the most affected (Table 1), suggesting an impact of female sex hormones on inflammation regulation.6
�
Table 1. Characteristics of plasma cell granulomas (2013 � 2023).
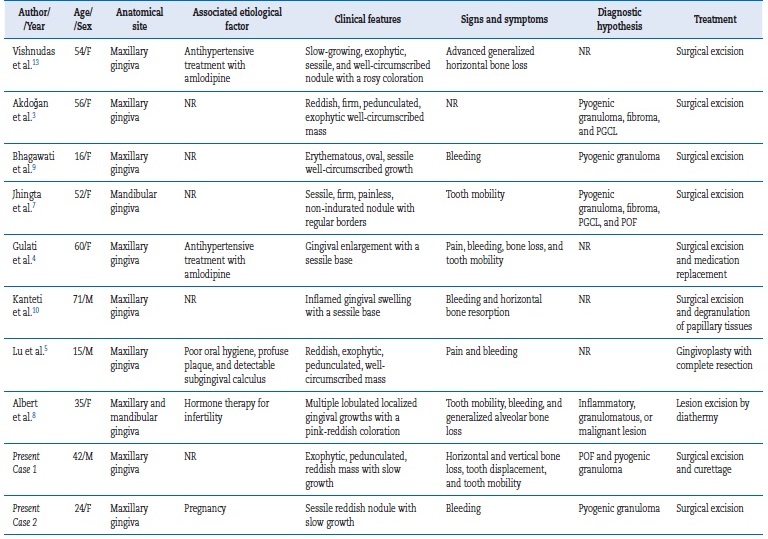
� female; M � male; NR � not reported; PGCL � peripheral giant cell lesion; POF � peripheral ossifying fibroma.
�
In general, PCG clinically manifests as an exophytic, solitary, well-circumscribed lesion that tends to bleed easily because of its friable nature.7 Possible bone loss has also been reported.5, 7 Table 1 summarizes the clinical presentations and signs and symptoms reported in publications on gingival PCG. Bone loss, tooth mobility, and bleeding were common characteristics in the cases analyzed. Although PCG is a benign condition, its ability for bone infiltration and erosion in the oral cavity demonstrates its potential local aggressiveness, which can often represent a diagnostic challenge by mimicking malignant conditions and can affect the disease outcome.7, 8
The histological findings of the two cases reported here agree with the histopathological features reported for gingival PCG, including aggregates of numerous mature plasma cells surrounded by scarce lymphocytes, neutrophils, eosinophils, and histiocytes and separated by dense and intertwined collagen fibers.5 This fibrosis may be related to certain growth factors released by myofibroblasts, which induce collagen fiber production necessary for tissue remodeling and repair.15 Russell bodies are observed occasionally,5 and this finding supports the reactive nature of the plasma cell aggregates.3,6 Cytological abnormalities are usually not found.5
Unlike PCG, plasmacytoma consists of typical and atypical plasma cells. Differentiation between plasmacytoma and PCG is important since the latter is benign, while the former can behave more aggressively and progress to multiple myeloma.8
Despite the typical histopathological features of PCG, immunohistochemistry is mandatory to determine the exact clonality and diagnosis.5 Plasma cells are polyclonal, and immunohistochemistry or in-situ hybridization shows uniform and positive reactivity to κ and λ light chains.10 The ratio of κ to λ light chains is 2:1 in PCG, whereas it is probably greater than 10:1 in malignant lesions.5 In the cases reported here, the results revealed a polyclonal immunohistochemical staining pattern, with positivity for κ and λ light chains (2:1), confirming the diagnosis of PCG.
PCG treatment consists of scraping and curettage, complete excision of the lesion, and extraction of compromised teeth adjacent to the lesion.3 This approach was used in Case 1. Overall, the prognosis of gingival PCG is good due to its low recurrence rate, but long-term follow-up is recommended.8 The patients of the two reported cases are being followed up and have shown no clinical or radiographic signs of recurrence.
The primary limitation of this study is the limited number of cases in the literature that could support and guide the definition of this lesion pathogenesis. This limitation stems from the rarity of PCG in oral mucosa, which may restrict the generalizability of the findings to other populations.
Further studies with more cases are required to confirm the results and provide a more comprehensive understanding of this rare lesion�s clinical, histopathological, and prognostic characteristics. In conclusion, this study describes two cases of a rare PCG lesion in the mouth. In the oral cavity, this lesion shows a predilection for the gingiva. Despite its uncertain etiology, irritating, medicinal, and hormonal factors appear to substantially impact PCG pathogenesis. This study�s findings reinforce the evidence of gingival PCG and the need to include this entity in the differential diagnosis of gingival lesions.
Careful examination, including histopathological analysis, must be performed, as well as confirmation using more advanced techniques such as immunohistochemistry when necessary.
�
References
1. Bhaskar SN, Levin MP, Frisch J. Plasma cell granuloma of periodontal tissues. Report of 45 cases. Periodontics. 1968;6:272-6.
2. Soares J, Nunes JF, Sacadura J. Plasma cell granuloma of the tongue. Report of a case. Histol Histopathol. 1987;2:199-201.
3. Akdoğan N, Yal�ın B, Aksoy GG, Tuna EE, �nal DT. A Case of Plasma Cell Granuloma Located on the Gingiva. Am J Dermatopathol. 2017;39:393-6.
4. Gulati R, Ratre MS, Khetarpal S, Varma M. A Case Report of a Gingival Plasma Cell Granuloma in a Patient on Antihypertensive Therapy: Diagnostic Enigma. Front Dent. 2019;16:144-8.
5. Lu W, Qi GG, Li XJ, He FM, Hong B. Gingival Plasma Cell Granuloma: A case Report of Multiple Lesions. J Clin Pediatr Dent. 2020;44:436-41.
6. Ibrahim MMA. Role of myofibroblasts in oral plasma cell granuloma: Immunohistochemical evaluation of α-SMA and ALK in a retrospective study of 30 cases. J Stomatol Oral Maxillofac Surg. 2023;124:101595.
7. Jhingta PK, Mardi K, Sharma D, Bhardwaj VK, Bhardwaj A, Saroch N, et al. An Enigmatic Clinical Presentation of Plasma Cell Granuloma of the Oral Cavity. Contemp Clin Dent. 2018;9:132-6.
8. Albert D, Muthusekhar MR, Kumar SP, Krishnan M. A Rare Case of Hormone-Induced Plasma Cell Granuloma of th Gingiva. Cureus. 2022;14:e23897.
9. Bhagawati BT, Sharanamma B, Kanwar D. Plasma cell granuloma of gingiva: A rare entity. J Indian Acad Oral Med Radiol. 2018;30:82-4.
10. Kanteti AP, Kelsey WP, Duarte EM. A Rare Case of Plasma Cell Granuloma. Case Rep Dent. 2020;2020:8861918.
11. Ajibade DV, Tanaka IK, Paghdal KV, Mirani N, Lee HJ, Jyung RW. Inflammatory pseudotumor (plasma cell granuloma) of the temporal bone. Ear Nose Throat J. 2010;89:E1-13.
12. Laco J, Kamar�dov� K, Mottl R, Mottlov� A, Dole�alov� H, Tuček L, et al. Plasma cell granuloma of the oral cavity: a mucosal manifestation of immunoglobulin G4-related disease or a mimic? Virchows Arch. 2015;466:255-63.
13. Vishnudas B, Sameer Z, Shriram B, Rekha K. Amlodipine induced plasma cell granuloma of the gingiva: A novel case report. J Nat Sci Biol Med. 2014;5:472-6. 36 rev port estomatol med dent cir maxilofac . 2025;66(1):31-37
14. Lauritano D, Lucchese A, Di Stasio D, Della Vella F, Cura F, Palmieri A, et al. Molecular Aspects of Drug-Induced Gingival Overgrowth: An In Vitro Study on Amlodipine and Gingival Fibroblasts. Int J Mol Sci. 2019;20:2047.
15. Smith PC, Mart�nez C, Mart�nez J, McCulloch CA. Role of Fibroblast Populations in Periodontal Wound Healing and Tissue Remodeling. Front Physiol. 2019;10:270.
�
Roseana de Almeida Freitas
E-mail address: roseanafreitas@hotmail.com
�
CRediT authorship contribution statement
Hannah Gil de Farias Morais: Conceptualization, Writing � original draft, Writing � review & editing. Renata Roque Ribeiro: Writing � review & editing. Jos� Nazareno Moreira de Aguiar J�nior: Data curation. Victor Diniz Borborema dos Santos: Data curation. Hevio Freitas de Lucena: Data curation. Roseana de Almeida Freitas: Project administration, Supervision
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Acknowledgments
This study was supported by the Postgraduate Program in Dental Sciences (Oral Pathology and Stomatology area), UFRN, and by the National Council for Scientific and Technological Development. RAF is a recipient of a productivity fellowship from the National Council for Scientific and Technological Development.
�
� 2025 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria.
Published by SPEMD. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
