
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2024 | 65 (4) | 165-172
Original research
Psychometric properties of the Dental Fear Schedule Subscale in a Portuguese pediatric population: exploratory study
Propriedades psicométricas da Dental Fear Schedule Subscale numa população pediátrica portuguesa: estudo exploratório
a Universidade de Lisboa, Faculdade de Medicina Dentária, Unidade de Investigação e Ciências Orais e Biomédicas (UICOB), Lisbon, Portugal
Sónia Mendes - sonia.mendes@fmd.ulisboa.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 65
Issue - 4
Original research
Pages - 165-172
Go to Volume
Article History
Received on 16/11/2023
Accepted on 17/10/2024
Available Online on 18/12/2024
Keywords
Original Research
�
Psychometric properties of the Dental Fear Schedule Subscale in a Portuguese pediatric population: exploratory study
Propriedades psicom�tricas da Dental Fear Schedule Subscale numa popula��o pedi�trica portuguesa: estudo explorat�rio
�
In�s Esteves1 0009-0009-5405-1149
Andreia Costa1 0009-0001-0930-4997
Ana Coelho Canta1 0000-0003-2419-771X
S�nia Mendes1,* 0000-0001-8831-5872
1 Universidade de Lisboa, Faculdade de Medicina Dent�ria, Unidade de Investiga��o e Ci�ncias Orais e Biom�dicas (UICOB), Lisbon, Portugal
�
Article history:
Received 16 November 2023
Accepted 17 November 2024
Available online 18 December 2024
�
�
Abstract
Objectives: To conduct a psychometric evaluation of the Dental Fear Schedule Subscale-Short Form (DFSS-SF) in a Portuguese pediatric population.
Methods: In this cross-sectional study, the DFSS-SF was applied to a convenience sample of 48 children (aged 3�9 years) in a university dental clinic. Child behavior during the consultation was assessed using the Frankl Behaviour Rating Scale (FBRS). The analysis included item frequency, internal consistency (Cronbach's α), and factor structure of the DFSS-SF. Criterion validity was assessed by correlating the DFSS-SF and FBRS scores (Spearman correlation). Discriminant validity was analyzed using the variables sex, age, treatment complexity, and child�s behavior during the appointment, employing the Mann-Whitney test (for items) and Student�s t test (for the scale's total score) (α=0.05).
Results: Anxiety prevalence was 20.8%. Items linked to higher anxiety included extractions, injections, and drills. Items showed good distribution, and the scale's internal consistency was α=0.49. Factor analysis identified two factors: �Fear of unknown people� and �Fear of invasive procedures,� explaining 54.1% of the variance. A significant inverse correlation was observed between DFSS-SF and FBRS scores (r=-0.346; p=0.008). Younger children exhibited higher anxiety levels (p=0.03).
Conclusion: The DFSS-SF demonstrated adequate performance in assessing anxiety related to dental consultations in the studied sample. Items showed good distribution and inter- item correlation. Internal consistency was acceptable, and there was an inverse correlation between anxiety and the child's behavior.
Keywords: Child behavior, Dental anxiety, Oral health, Reliability and Validity
�
Resumo
Objetivos: Realizar um estudo psicom�trico da escala Dental Fear Schedule Subscale-Short Form (DFSS-SF) numa popula��o pedi�trica portuguesa.
M�todos: Estudo transversal com aplica��o da DFSS-SF a uma amostra de conveni�ncia de 48 crian�as (3�9 anos) numa cl�nica dent�ria universit�ria. O comportamento infantil durante a consulta foi classificado pela Frankl Behaviour Rating Scale (FBRS). Avaliaram-se a frequ�ncia dos itens, a consist�ncia interna (α de Cronbach) e a estrutura fatorial da DFSSSF. A validade de crit�rio foi estudada pela correla��o entre as escalas DFSS-SF e FBRS (correla��o de Spearman). A validade discriminante foi analisada com as vari�veis sexo, idade, complexidade do tratamento e comportamento na consulta, usando os testes Mann-Whitney (no caso dos itens) e t de Student (no caso do somat�rio da escala) (α=0,05).
Resultados: A preval�ncia de ansiedade foi 20,8%. Os itens associados a n�veis superiores de ansiedade inclu�ram extra��es, inje��es e instrumentos rotat�rios. Os itens apresentaram boa distribui��o e a consist�ncia interna da escala foi α=0,49. A an�lise fatorial identificou dois fatores: "Medo de pessoas desconhecidas" e "Medo de procedimentos invasivos", explicando 54,1% da vari�ncia. Observou-se uma correla��o inversa significativa entre os valores da DFSS-SF e da FBRS (r=-0,346; p=0,008). Crian�as mais jovens demonstraram maior ansiedade (p=0,03).
Conclus�o: A DFSS-SF apresentou desempenho adequado para medir a ansiedade associada � consulta dent�ria na amostra estudada. Os itens mostraram boa distribui��o e correla��o inter-item. A consist�ncia interna foi aceit�vel e verificou-se a correla��o inversa entre ansiedade e comportamento infantil.
Palavras-chave: Comportamento infantil, Ansiedade dent�ria, Sa�de oral, Fiabilidade e Validade
�
Introduction
According to the Diagnostic and Statistical Manual of Mental Disorders, anxiety disorders are mainly characterized by excessive fear and anxiety accompanied by behavioral changes.1
While fear focuses on a known external threat that exists and is imminent, anxiety is a generalized response to unknown threats characterized by their uncontrollability and potential future negative events. The main function of these states is to react to signs of danger or conflict, triggering appropriate adaptive responses2 Anxiety disorders differ from physiological anxiety or fear experienced in everyday activities by exceeding these states� appropriate degree and duration.1, 3
The literature sometimes uses the terms �dental fear� and �dental anxiety� indistinctively. However, they correspond to different degrees of the same psychological condition:4 the response to anticipated or immediate threats during dental treatment.5 These psychological states are expressed by various defense behaviors aimed at avoiding the threat or conflict.6
Although anxiety can be an adaptive physiological reaction, when pathological and disproportionate to the threat, it can interfere with functioning during stressful activities or events.2, 6
Namely, odontophobia is characterized by a state of marked, persistent, excessive, and irrational anxiety regarding dental treatment, simultaneously causing alterations such as hypertension, malaise, and distress, interfering with the patient�s functioning.1, 3, 6, 7 Dental anxiety is characterized by an irrational negative emotional state, specific to situations about dental treatment, associated with a feeling of loss of control and the unpredictability of the appointment.6, 7 It is often associated with greater difficulty in dental treatment, recurrent missed appointments, and consequent oral health deterioration.5, 8
The anxiety associated with dental appointments can derive from various situations, such as the choking sensation, the gag reflex, a fear of injections, or an aversion to blood.7 It may also be triggered by other factors, such as the sensation of anesthesia, low pain tolerance, confidence in the dentist�s abilities, previous negative experiences, or the office environment.6, 7
The prevalence of dental anxiety in children and adolescentes ranges from 13.3% to 29.3%.4 Sex and age are among the most frequently assessed factors in studies related to anxiety at dental appointments, and younger and female patients show more anxiety.2
On the other hand, behavioral problems at dental appointments have a prevalence of around 9% in the pediatric population.6, 9 Children�s behavior is influenced by various factors, including age, intellectual capacity, maturity degree, and coping mechanisms, but also the child�s temperament, general behavior, socioeconomic status, cultural and family factors, and their parent�s level of anxiety.6, 8, 9 Children with increased levels of anxiety have shown changes in their behavior during appointments, especially during more invasive treatments.8, 9
Recognizing the anticipatory nature of anxiety during dental appointments allows for better communication and adaptation of the dental treatment plan for pediatric patients with this condition.10
The anxiety associated with dental appointments can be measured by three
methods: behavioral assessment, psychometric assessment, and analysis of the
physiological response.11 Psychometric assessment is the most
common technique due to its high
convenience. It involves the child
or parents filling in questionnaires before or after
treatment. The child answers questions,
which can be accompanied by visual scales, providing information about their dental anxiety without the involvement
of parents or guardians. There
are various visual scales, such as the Venham Picture Test, the Children�s
Dental Fear Picture Test, and, the simplest,
the Facial Image Scale, which consists
of images with five contrasting
emotions, from �very happy� to �very sad.�12
One of the most frequently
used instruments for measuring dental anxiety in children is the
Children�s Fear Survey Schedule � Dental Subscale (CFSS-DS), created by Cuthbert and
Melamed in 1982.13 This
scale consists of 15 items on
general, medical, and dental situations,
each rated from 1 (not afraid)
to 5 (very afraid), with total values ranging from 15 to 75. Compared to other dental anxiety assessment scales, the CFSS-DS covers more aspects of the
dental appointment, measures
dental anxiety more accurately,
and has better
psychometric properties, with good test-retest
reliability and internal consistency.14 However,
a study revealed that the agreement
between the psychometric assessment of questionnaires completed by the
children or their parents and
the child�s level of dental anxiety was not
high.6 Some items
in the CFSS-DS scale are irrelevant to explaining the variance in results, so modified
versions of the original scale were created with
fewer items.15 The
scale created by Carson and
Freeman (Dental Fear Survey Subscale Short Form � DFSS-SF) resulted from reducing the
CFSS-DS scale from 15 to eight items.10 This shorter scale classifies
each of the
eight items on a five-point scale, like the
CFSS-DS, so its sum varies between eight and 40 points, with higher values corresponding
to higher anxiety levels. The behavioral assessment of anxiety
consists of the dentist evaluating
the child�s behavioral and emotional reactions during treatment using standardized descriptive scales.11 Some examples
of these scales are the Frankl Behavior Rating Scale (FBRS),16 the Clinical Anxiety
Rating Scale (CARS),17 and the Behavior Evaluation
Scale (BES).18 The
FBRS scale is a frequently used behavioral rating scale based on rating the child�s attitude
as positive or negative. The
behavioral assessment by the dentist
can be a useful method of measuring
anxiety in very young children. Assessing the anxiety associated with a child�s dental appointment could be valuable, as it can help effectively
control behaviors, anxiety, and, ultimately,
pain.5 Therefore, this
study aims to contribute to the Portuguese validation of the DFSS-SF by conducting a psychometric study of the Portuguese version of this
scale when applied to a Portuguese pediatric
population at a university clinic. Material and methods An observational
cross-sectional study was conducted on
children who attended pediatric dentistry appointments from the pre
and post-graduate courses at a university
dental clinic in Portugal. The
health ethics committee of the
same Portuguese university approved the study. The convenience
sample included children between 3 and 9 years old. Their
parent/guardian�s informed, free, voluntary consent and the
child�s assent were obtained for the study participation.
Patients with special needs and
institutionalized patients were excluded. The sample included children who met
the above criteria and attended
the appointment on the specific
days of data collection. The data was collected in the 2020/21 and 2022/23 school years by two
trained researchers in the waiting room
of the university
clinic before the appointment. The child�s parents/guardians were given a questionnaire on demographic information and information about the child�s previous
appointments and experiences. The children�s version of the DFSS-SF10 was applied to measure anxiety related to dental appointments. Since the CFSS-DS scale had already
been validated for Brazilian Portuguese by Cademartori et al.,8 this Brazilian version was adapted
for European Portuguese, and
only the DFSS-SF items were used.
The modifications to the Brazilian Portuguese version were limited
to minor linguistic adaptations to maintain the original meaning of the questions
for the target population. The DFSS-SF consists
of 8 items: tooth extraction, injections, dentist drilling, meeting the dentist, mouth examinations, tooth cleaning by others,
people in white uniforms, and having
to open the mouth wide. The child
classifies each item with five possible
responses: 1 � Not afraid;
2 � Slightly afraid; 3 � Somewhat afraid; 4 � Afraid; 5 � Very afraid. The child�s
anxiety score corresponds to
the sum of the answers to the eight items,
with a minimum of 8 points and
a maximum of 40 points. Higher scores correspond to higher levels of anxiety.10 The child was considered anxious when the
score of the DFSSSF exceeded 20 points. Since the study
population included very young children,
as in other similar studies,
the child�s response options were complemented
with a validated image scale, the
Facial Image Scale (FIS), consisting of five
images of faces showing different emotions, from happy to sad.19 After the appointment, the dentist responsible for the treatment was
asked to describe the child�s behavior
using the FBRS.16 The present study used a Portuguese version of this
scale that had been previously
used in another study carried out at the same
university clinic.20 Information
about the type of dental treatment was also
requested based on its classification
as invasive or minimally invasive. A higher score in the FBRS corresponds to a more positive behavior.
The dentist responsible for the appointment was unaware of the
child�s previous answers. Statistical analysis included calculating the absolute and
relative frequencies of the variables
and, in the case of numerical variables,
the mean and standard deviation. Internal consistency was analyzed using
Cronbach�s α. Principal componente factor analysis with varimax rotation
was calculated, considering that all factors should
contain a minimum of three items.21 Criterion validity was studied using
Spearman�s correv relation between the mean values
of the DFSS-SF and the FBRS. The Mann-Whitney test was used
to analyze the DFSS-SF questionnaire items and the parametric
t test for the total
DFSS-SF sum, considering the
characteristics and normality of the
variables. A statistical
significance level of 5% was set for all tests. Results The sample included
48 children, with a mean age of 6.98 (SD=1.5). Most children (85.4%) had a previous dental treatment, and 29.2% had a traumatic experience at a dental
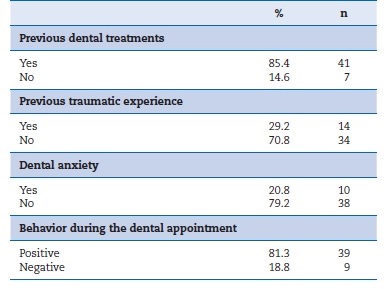
appointment. Around a fifth of the sample (20.8%) had dental anxiety, and 18.8% had negative behavior during the appointment (Table 1). � Table
1. Characterization
of the sample in terms of previous
dental treatments and experiences, anxiety, and behavior during
the dental appointment.
�
The item analysis revealed a mean DFSS-SF score of 17.6 (SD=4.7), with minimum and maximum values of 8 and 34, respectively. The various possible responses were well-distributed in most items, and no response showed very high frequency (greater than 95%) in any item. Only the item �Cleaning your teeth� showed no �Very afraid� responses. The items �Tooth extraction,� �Injections,� and �Dentist drilling� had the highest mean values of 3.1, 3.5, and 3.0, respectively. The remaining items had relatively low mean values, between 1 and 2, with �Meeting the dentist� having the lowest mean value of 1.4 (Table 2).
�
Table 2. Frequency, mean, and standard deviation of DFSS-SF items.
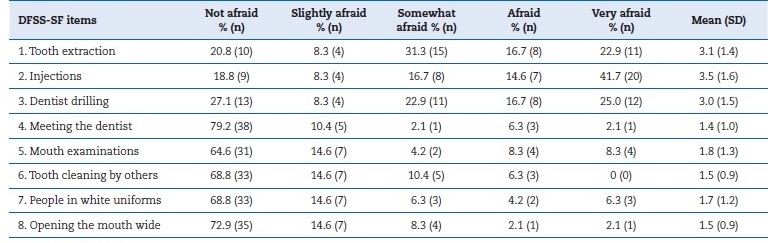
SD, standard deviation.
�
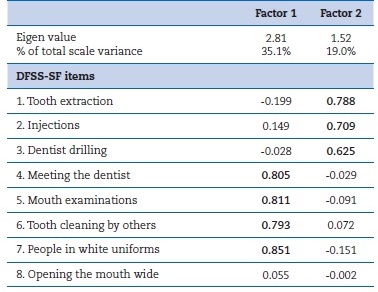
The factor analysis indicated two main factors that together explained 54.1% of the scale�s total variance. The Kaiser-Meyer-Olkin test value was 0.675, and Bartlett�s test of sphericity rejected the null hypothesis, indicating that the sample was suitable for this type of analysis (Table 3). As item 8 had a low factor loading (less than 0.3), a new factor analysis was made with only the remaining seven items. However, the exclusion of the eighth item revealed no significant improvements or differences in inter-item correlation or internal consistency, so the eight-item assessment was maintained. Moreover, because there are very few validation studies of the DFSS-SF scale and few items assessed, keeping the eighth item is prudent to allow comparison between existing studies. The internal consistency of the 8-item scale showed a Cronbach�s α value of 0.49. No item led to a significant increase in Cronbach�s α when eliminated.
�
Table 3. Rotated component matrix of the two DFSS-SF factors.
�
The item-total correlation analysis confirmed the non-redundancy of the items, with all items being moderately correlated with each other. The criterion validity showed a moderate correlation between the DFSS-SF and the FBRS scores (r=-0.346; p=0.008), showing an inverse relationship between the two scales: as the DFSS-SF score increased, the FBRS score decreased. This finding indicates a correlation between increased child�s anxiety and a worse assessment of their behavior during dental treatment. Table 4 shows the discriminant validity with the relationships between the DFSS-SF items and the variables sex, age group, type of treatment, and behavior during the appointment.
�
Table 4. Discriminant validity of the DFSS-SF.
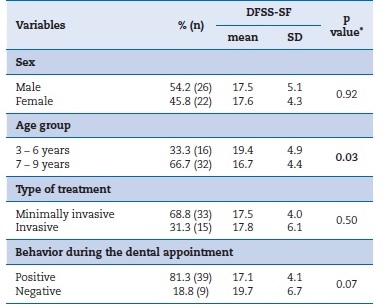
*Student�s t test; SD, standard deviation.
Values in bold indicate statistically significant differences.
�
There were no significant differences in the total DFSSSF score between the variables sex, type of treatment, and behavior during the dental appointment.
The variables sex and type of treatment showed very similar DFSS-SF score means, and no significant differences were found (p<0.05). In turn, children in the 3�6 age group had higher DFSS-SF scores than children aged 7�9 years (p=0.03). Although not significant, but close to the decision value, children with positive behavior had lower DFSS-SF scores than children with negative behavior in the dental appointment (p=0.07).
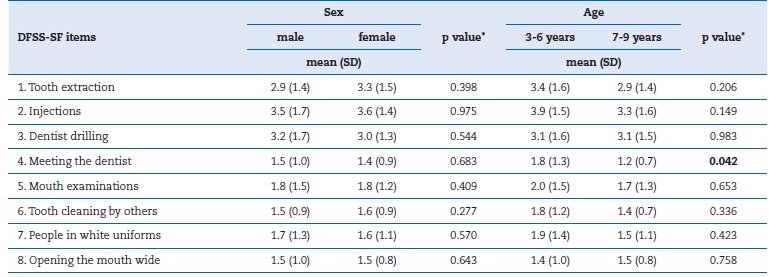
Table 5 shows the mean scores of the DFSS-SF items by sex and age group. None of the variables evaluated showed statistically significant differences (p<0.05), except for item 4 (�Meeting the dentist�), for which the 3�6 age group showed a higher mean score than the 7�9 years old (p=0.042). Table 6 shows the mean scores of the DFSS-SF items by behavior during the dental appointment and type of treatment. None of the variables evaluated showed statistically significant differences (p<0.05).
�
Table 5. Mean and standard deviation of DFSS-SF items by sex and age.
�
Table 6. Mean and standard deviation per DFSS-SF item, according to FBRS and type of treatment
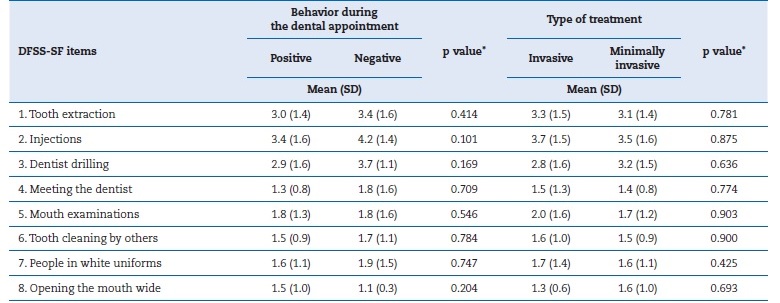
*Mann-Whitney test. SD, standard deviation.
�
Discussion
Assessing dental anxiety is relevant to clinical practice, and there is a need for simple and effective assessment methods. Clinical examinations alone may not correctly assess the patient�s dental anxiety. Their association with psychometric methods, such as the scale used in this study, would provide more accurate assessments. In this study, a cut-off value of 20 points in the DFSS-SF score indicated that 20.8% of the sample had dental anxiety.
This result is in line with the literature, which shows a variable prevalence of anxiety with higher values for younger children, 4, 8, 22, 23 as in this study. The behavior during the dental appointment, assessed by the FBRS, showed an 18.8% frequency of uncooperative children. Nakai et al. found a similar prevalence of 15%,(24) while Cademartori et al8 observed a higher value (39.1%).
The mean DFSS-SF score (17.6) was much lower than what Carson et al.11 found (25.7) but closer to that reported by Foylayan et al.25 (16.9). The participating children indicated tooth extractions, injections, and the use of drills as the most anxiety-inducing stimuli, with these items showing a higher mean score. Carson et al. also found higher mean values for the items �Tooth extraction� and �Injections,�10 while Andrade et al. found the highest mean values for �Dentist drilling�.26
These results show, as expected, that children fear more invasive procedures. The similar dental anxiety results between boys and girls found in this study agree with other studies.8, 26 - 28 However, some studies have shown higher dental anxiety scores in girls.2, 24 The DFSS-SF items behaved quite reasonably, showing good distribution and good inter-item correlation. The internal consistency value can be considered somewhat low, but Cronbach�s α values lower than 0.5 are considered acceptable for samples of 25 to 50 individuals.29 As the inter-item analysis revealed values generally greater than 0.4 and the scale has only eight items, this result may indicate an acceptable internal consistency, even if Cronbach�s α is below what is normally considered satisfactory. Thus, the 8-item scale showed na acceptable internal consistency for the study sample size (Cronbach�s α= 0.49). Other studies using the 15-item CFSS-DS scale have shown higher internal consistency values, ranging between 0.83 and 0.92.24, 27, 28, 30, 31
Factor analysis showed two main factors in the scale construct. The first, �Fear of unknown people,� explained 35.1% of the variance, and the second, �Fear of invasive procedures,� explained 19.0%. Carson et al.�s original scale study10 and Rantavuori et al.32 also detected two factors. The former10found a total variance of 64%, with Factor 1 (invasive treatments) having a variance of 47% and Factor 2 (items related to the dental examination) a variance of 15%. The latter study32 showed a total variance o f 60.8%, with Factor 1 (invasive treatments) having a variance of 44.7% and Factor 2 (experiencing the dental appointment) having a variance of 16.1%. The constructs of the factors obtained in the present study are inversely ordered compared to these studies, with �Fear of unknown people� as the first factor and the one with the most relevant explained variance. The variations between the factors could be associated with different types of samples, and social, cultural, or demographic differences.
Several studies that used the 15-item CFSS-DS had more factors in the factor analysis. Three factors were obtained in the Netherlands,28 Finland,30 India,27, and Japan,24 with explained variance values between 54% and 65%. Other studies have found four factors in the factor analysis.8, 31
There was a moderate inverse correlation between the DFSS-SF and the FBRS scores, which indicated a correlation between increased dental anxiety and worse behavior during dental treatment. Other studies also found this inverse correlation between the CFSS-DS and the FBRS.24, 33 This finding demonstrates and supports the importance of studying dental anxiety, ideally before the appointment, so that procedures can be adapted and, if possible, treatments carried out in a way that promotes a more pleasant appointment and experience.
Younger children have higher DFSS-SF scores than older children. This result is supported by the literature and explained by the fact that younger children have less cognitive development, less impulse control, and less ability to adapt their behavior to stressful situations.2, 12 Younger children�s behavior is affected by immature cognition, increased sensitivity to anxiety-inducing situations, lower behavioral adjustment skills, and lower attention span. Moreover, they have increased pain perception, with worse responses to conventional communication and behavior control techniques.5, 9
Dental anxiety is an important factor that contributes to postponing or not attending dental appointments, which can result in a worsening of the patient�s oral health condition and the need for more complex treatments. Thus, it may lead to a vicious cycle of appointment avoidance and worsening oral health status, decreasing the patient�s quality of life.3, 7
Dental procedures and the patient�s positioning in the chair can create feelings of lack of control and represent na invasion of their personal space, so communication skills and positive previous experiences with the patient are essential for future procedures. To adequately control dental anxiety, the dental team plays an essential role in drawing up individualized treatment plans for the patient and using communication and empathy techniques to increase comfort during the appointment.3Encompassing pediatric knowledge, including regarding dental anxiety, can lead to a dental appointment properly planned and result in a better experience and increased treatment success.6, 7 This is particularly important in younger children, as they are the ones who usually presente higher levels of dental anxiety, as previously explained.
This study used a convenience sample of children seeking oral health care, so its results cannot be extrapolated to the Portuguese pediatric population. The sample size, although small, complies with the general rule adopted by many researchers that the number of respondents for each item equals the number of response options in each statement. Since the scale has 8 items and 5 response options for all items, it would require a minimum sample of 40 individuals. Moreover, it is recommended that the sample includes at least 20 percent more respondents, which was also met with the 48 individuals in this study.34 Obtaining a larger sample was difficult because the data were collected during the COVID-19 pandemic years when there were specific rules and procedures implemented for controlling the pandemic and a lower demand for oral health care by individuals who met the study inclusion criteria.
Therefore, it would be important to apply this scale to a bigger sample and study its behavior in a representative population, including not only children in dental clinics but also children in schools, where dental anxiety could be assessed not directly related to dental appointments and treatments.
Further studies must be carried out to validate instruments for measuring dental anxiety, ideally with larger samples that include children from community settings and not just clinics. Despite its limitations, this study can be considered na important contribution to the validation of the DFSS-SF for the Portuguese population. The validation of psychometric scales, such as the DFSS-SF, is important as they could become a useful clinical tool for measuring dental anxiety in pediatric patients and assessing its causal factors, allowing the treatment plan to be adapted and avoiding potential negative experiences.
Obtaining psychometric information on the anxiety associated with dental appointments could improve our understanding of this type of disorder by helping us identify the stimuli that induce it and adapt the procedures to prevent it.
Conclusions
In this exploratory study, the DFSS-SF performed adequately and acceptably. This scale can be used to assess dental anxiety in the studied population. The items showed a good distribution and a good inter-item correlation. The internal consistency value was acceptable, and the factor analysis showed two main factors in the scale construct. There was an inverse correlation between increased dental anxiety and worse behavior during dental treatment. Younger children had higher values of dental anxiety than older children. The DFSS-SF seems to have adequate behavior and is appropriate for the evaluation of anxiety associated with dental appointments in the studied population.
�
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-5-TR. 5th ed. American Psychiatric Association, 2022: p 215�217.
2. Steimer T. The biology of fear- and anxiety-related behaviors. Dialogues Clin Neurosci. 2002;4:231-49.
3. Murad MH, Ingle NA, Assery MK. Evaluating factos associated with fear and anxiety to dental treatment-A systematic review. J Family Med Prim Care. 2020;9:4530-5.
4. Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, et al. Dental fear/anxiety among children and adolescents. A systematic review. Eur J Paediatr Dent. 2017;18:121-30.
5. Lin CS, Wu SY, Yi CA. Association between Anxiety and Pain in Dental Treatment: A Systematic Review and Meta-analysis. J Dent Res. 2017;96:153-62.
6. Klingberg G, Broberg AG. Dental fear/anxiety and dental behaviour management problems in children and adolescents: a review of prevalence and concomitante psychological factors. Int J Paediatr Dent. 2007;17:391-406.
7. Armfield JM, Heaton LJ. Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 2013;58:390-407.
8. Cademartori MG, Cara G, Pinto GDS, da Costa VPP. Validity of the Brazilian version of the Dental Subscale of Children�s Fear Survey Schedule. Int J Paediatr Dent. 2019;29:736-47.
9. Jain A, Suprabha BS, Shenoy R, Rao A. Association of temperament with dental anxiety and behaviour of the preschool child during the initial dental visit. Eur J Oral Sci. 2019;127:147-55.
10. Carson P, Freeman R. Assessing child dental anxiety: the validity of clinical observations. Int J Paediatr Dent. 1997;7:171-6.
11. Porritt J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children�s dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol. 2013;41:130-42.
12. Yon MJY, Chen KJ, Gao SS, Duangthip D, Lo ECM, Chu CH. Na Introduction to Assessing Dental Fear and Anxiety in Children. Healthcare (Basel). 2020;8:86.
13. Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child. 1982;49:432�6.
14. Aartman IH, van Everdingen T, Hoogstraten J, Schuurs AH. Self-report measurements of dental anxiety and fear in children: a critical assessment. ASDC J Dent Child. 1998;65:229-30,252-8.
15. Bajrić E, Koba�lija S, Jurić H, Huseinbegović A, Zukanović A. The Reliability and Validity of the Three Modified Versions of the Children�s Fear Survey Schedule-Dental Subscale of 9-12 Year Old Children in a Clinical Setting in Bosnia and Herzegovina. Acta Med Acad. 2018;47:1-10.
16. Frankl SN, Shiere FR, Fogels H. Should the parent remain with the child in the dental operatory? J Dent Child. 1962;29:150�63.
17. Venham LL, Gaulin-Kremer E, Munster E, Bengston-Audia D, Cohan J. Interval rating scales for children�s dental anxiety and uncooperative behavior. Pediatr Dent. 1980;2:195�202.
18. Shinohara S, Nomura Y, Shingyouchi K, Takase A, Ide M, Moriyasu K, et al. Structural relationship of child behavior and its evaluation during dental treatment. J Oral Sci. 2005;47:91-6.
19. Buchanan H, Niven N. Validation of a Facial Image Scale to assess child dental anxiety. Int J Paediatr Dent. 2002;12:47�52.
20. Costa A. Ansiedade na popula��o pedi�trica da cl�nica universit�ria da Faculdade de Medicina Dent�ria da Universidade de Lisboa. escolar [Master thesis]. Lisboa: Universidade de Lisboa; 2020. Available from: https://repositorio.ul.pt/handle/10451/50121. Accessed 16 November, 2023.
21. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6:284�90.
22. Grisolia BM, Dos Santos APP, Dhyppolito IM, Buchanan H, Hill K, Oliveira BH. Prevalence of dental anxiety in children and adolescents globally: A systematic review with metaanalyses. Int J Paediatr Dent. 2021;31:168-183.
23. 23 Sun IG, Chu CH, Lo ECM, Duangthip D. Global prevalence of early childhood dental fear and anxiety: A systematic review and meta-analysis. J Dent. 2024;142:104841.
24. Nakai Y, Hirakawa T, Milgrom P, Coolidge T, Heima M, Mori Y, et al. The Children�s Fear Survey Schedule�Dental Subscale in Japan. Community Dent Oral Epidemiol. 2005;33:196�204.
25. Folayan MO, Adekoya-Sofowora CA, D Otuyemi O, Ufomata D. Parental anxiety as a possible predisposing factor to child dental anxiety in patients seen in a suburban dental hospital in Nigeria. Int J Paediatr Dent. 2002;12:255-9.
26. Andrade NM, Laureano ICC, Farias L, Fernandes LHF, Prates CC, Cavalcanti AL. Moderate and high dental fear by sex and age using the Children�s Fear Survey Schedule-Dental Subscale. Rev Port Estomatol Med Dent Cir Maxilofac. 2021;62:157-62.
27. Singh P, Pandey RK, Nagar A, Dutt K. Reliability and factor analysis of children�s fear survey schedule-dental subscale in Indian subjects. J Indian Soc Pedod Prev Dent. 2010;28:151-5.
28. ten Berge M, Hoogstraten J, Veerkamp JSJ, Prins PJM. The Dental Subscale of the Childrens Fear Survey Schedule: a factor analytic study in the Netherlands. Community Dent Oral Epidemiol. 1998;26:340�3.
29. Flanagan JC. Book Review: Davis, Frederick B. Educational Measurements and Their Interpretation. Belmont, Calif. Am Educ Res J. 1965;2:247�8.
30. Alvesalo I, Murtomaa H, Milgrom P, Honkanen A, Karjalainen M, Tay KM. The Dental Fear Survey Schedule: a study with Finnish children. Int J Paediatr Dent. 1993;3:193-8.
31. Bajrić E, Koba�lija S, Jurić H. Reliability and validity of Dental Subscale of the Children�s Fear Survey Schedule (CFSS-DS) in children in Bosnia and Herzegovina. Bosn J Basic Med Sci. 2011;11:214-8.
32. Rantavuori K, Lahti S, Sepp� L, Hausen H. Dental fear of Finnish children in the light of different measures of dental fear. Acta Odontol Scand. 2005;63:239-44.
33. El-Housseiny AA, Alamoudi NM, Farsi NM, El Derwi DA. Characteristics of dental fear among Arabic-speaking children: a descriptive study. BMC Oral Health. 2014;14:118.
34. Hair Jr JF, Marcelo GLDS, da Silva D, Braga Junior S. Development and validation of attitudes measurement scales: fundamental and practical aspects. RAUSP Management Journal. 2019;54(4):490-507.
�
S�nia Mendes
E-mail address:sonia.mendes@fmd.ulisboa.pt
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
CRediT authorship contribution statement
In�s Esteves: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Writing � original draft. Andreia Costa: Investigation, Methodology, Resources, Writing � review & editing. Ana Coelho Canta: Conceptualization, Methodology, Supervision, Validation, Writing � review & editing. S�nia Mendes: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing � review & editing.
�
1646-2890/� 2024 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
