
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2024 | 65 (3) | 148-155
Clinical case
Non-metal framework for removable partial dentures – A 2-year follow-up clinical report
Infraestrutura não metálica de prótese parcial removível – Caso clínico controlado com 2 anos
a Universidade de Lisboa, Faculdade de Medicina Dentária, Unidade de Investigação e Ciências Orais e Biomédicas (UICOB), Lisbon, Portugal
b Faculdade de Medicina Dentária da Universidade de Lisboa, Lisbon, Portugal
c Laboratório de Instrumentação, Engenharia Biomédica e Física da Radiação (LIBPhys), Lisbon, Portugal
Isabel Gomes - isabel.gomes@fmd.ulisboa.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 65
Issue - 3
Clinical case
Pages - 148-155
Go to Volume
Article History
Received on 29/06/2024
Accepted on 08/08/2024
Available Online on 30/09/2024
Keywords
linical Case Report
�
Non-metal framework for removable partial dentures � A 2-year follow-up clinical report
Infraestrutura n�o met�lica de pr�tese parcial remov�vel � Caso cl�nico controlado com 2 anos
�
Isabel Gomes1,* 0000-0002-9509-7495
Joana Gon�alves2 0009-0006-2249-1914
Jo�o Paulo Martins1 0000-0001-9330-772X
Lu�s Miguel Pires Lopes1,3 0000-0001-8633-827X
1 Universidade de Lisboa, Faculdade de Medicina Dent�ria, Unidade de Investiga��o e Ci�ncias Orais e Biom�dicas (UICOB), Lisbon, Portugal
2 Faculdade de Medicina Dent�ria da Universidade de Lisboa, Lisbon, Portugal
3 Laborat�rio de Instrumenta��o, Engenharia Biom�dica e F�sica da Radia��o (LIBPhys), Lisbon, Portugal
�
�
Article history:
Received 29 February 2024
Accepted 8 August 2024
Available online 30 September 2024
�
Abstract
Traditional removable partial dentures (RPDs) with cobalt-chromium frameworks have been used for several decades, restoring the masticatory function. However, these frameworks have been documented as aesthetically unacceptable due to the display of metal clasps. The patients' increased demands regarding the aesthetic aspects of rehabilitation treatment led to the introduction of new, more aesthetic materials in clinical practice. One of the main materials is polyetheretherketone (PEEK). This clinical report presents PEEK as an alternative material for fabricating RPD frameworks for a Class III Kennedy partial edentulous mandible. The framework was constructed using CAD/CAM manufacturing, and the process combined laboratory scanning, digital framework design, resin try-in milling, and PEEK framework milling. The framework showed good adaptation to the abutment teeth and surrounding tissues. The patient was followed for 2 years without complaints and was grateful for the aesthetics. During this period, there were no signs of degradation in the framework, and the clasps were still as retentive as they were at the initial appointment, with only some pigmentation of the structure being observed.
Keywords: CAD-CAM, PEEK, Removable partial denture
�
Resumo
As estruturas das pr�teses parciais remov�veis (PPR) em cobalto-crómio (Co-Cr), utilizadas h� v�rias d�cadas, t�m permitido devolver a fun��o mastigat�ria aos pacientes parcialmente desdentados. No entanto, estas estruturas n�o preenchem na totalidade o crit�rio est�tico, sendo uma queixa recorrente a visibilidade do metal das unidades gancho. Com a crescente exig�ncia est�tica imposta pelos pacientes em rela��o ao tratamento reabilitador, surgiu a necessidade do desenvolvimento de novos materiais com esta capacidade. Um material que tem permitido dar resposta a este requisito é o poli�ter-�ter-cetona (PEEK). O caso cl�nico apresentado descreve o fabrico da estrutura de uma PRR para a reabilita��o de uma desdenta��o mandibular Classe III de Kennedy, usando o PEEK como material alternativo ao Co-Cr. A estrutura foi constru�da com tecnologia CAD/CAM. O processo combinou a digitaliza��o dos modelos de gesso em laborat�rio, desenho digital da estrutura, fresagem duma estrutura de prova em resina e fresagem da estrutura em PEEK. A estrutura mostrou-se bem-adaptada aos dentes pilares e tecidos de suporte. A paciente foi seguida durante 2 anos, tendo-se mostrado muito satisfeita em rela��o ao tratamento reabilitador, quer quanto ao conforto e fun��o, quer quanto ao resultado est�tico. Passado este per�odo, a estrutura da PPR n�o mostrou sinais de degrada��o e os ganchos apresentavam-se retentivos como na consulta de inser��o, observando-se apenas alguma pigmenta��o da estrutura.
Palavras-chave: CAD-CAM, PEEK, Pr�tese parcial remov�vel
�
Introduction
The population�s improved oral health in developed countries leads to fewer teeth loss in adults, reducing the need for complete edentulism treatments. On the other hand, due to the increased life expectancy, the need for partial edentulism treatments is increasing.1 2 Accordingly, the 2023 OMD Oral Health Barometer revealed that 59.0% of the Portuguese population is missing at least one natural tooth, excluding third molars, and 6.4% is completely toothless.3 Among the rehabilitation options, removable partial dentures (RPD) remain na important treatment solution compared to more costly alternatives.4 In Portugal, 35.9% of the population with missing teeth opts for this rehabilitation treatment.3
The most used material for RPD metal frameworks is the cobalt-chromium (Co-Cr) alloy due to its low cost, high mechanical and corrosion resistance, and high modulus of elasticity.2, 4 Despite all its advantages, reports of metallic taste and allergic reactions, possible oral galvanism phenomena, and, especially, the unesthetic metal clasps have made it unpopular among patients.2, 5 - 7
Patients� preference for nonmetallic materials led to the development of other alternatives, such as polyoxymethylene (POM), also known as acetal resins. POM was introduced in 1971 as an alternative to conventional polymethylmethacrylate resins (PMMA).8, 9 Despite its initial success, POM�s low rigidity made its use in major connectors unfeasible, becoming a contraindicated material for RPD structures used for more than 6 months. 10, 11
Continued advancements in materials research led to the development of a new generation of high-performance polymers, which have largely replaced acetal resins. This new generation includes the aryl-ketone polymer (AKP) and the polyaryletherketone (PAEK), a group of polymers that includes polyetheretherketone (PEEK) and polyetherketoneketone (PEKK).1, 4
PEEK was developed by a group of English scientists in 1978.1 It was first commercialized for industrial and aerospace applications. By the late 1990s, PEEK had become an importante high-performance thermoplastic resin candidate for replacing metal implant components in the orthopedical field. Its use in dentistry is more recent, and currently, PEEK is used to manufacture dental implants,12 abutments,13 crowns and bridges,14 intra-radicular posts,15 maxillary obturator prostheses,16 orthodontic wires,17 and RPD structures.5, 18 PEEK materials are available in numerous shades, from classic pearl white to various tooth colors.19 PEEK is biocompatible, radiolucent, rigid, and has low plaque affinity.11, 14, 18 It has a flexural modulus of 140-170 MPa, 1300 kg/m3 of density, and a thermal conductivity of 0.29 W/mK.11, 20 PEEK�s mechanical properties do not change during sterilization and have high thermal stability � up to 335.8�C. PEEK became an importante high-performance resin candidate for replacing metal implant components in vertebral surgery and femoral prostheses in artificial hip joints.21 Furthermore, PEEK can be processed using computer-aided design/computer-aided manufacturing (CAD-CAM)20-22 with framework fabrication by milling under two possible protocols already described that combine conventional and digital workflow steps.23These digrev itally designed frameworks have proven to have similar, if not better, accuracy and fit compared to those fabricated by traditional methods.(1)
This paper aims to describe a clinical case where an RPD was fabricated with a digital workflow and a milled PEEK framework. PEEK�s clinical performance was assessed after 2 years of use.
Case report
A 40-year-old healthy female patient attended the Department of Removable Prosthodontics at the Faculty of Dental Medicine of the University of Lisbon. Clinical examination revealed a complete maxillary fixed denture opposing a partially edentulous mandible with a Kennedy-Applegate Class III with modification 1 (Figures 1 and 2).
�

Figure 1. Frontal view of the patient showing visible metal clasps.
�

Figure 2. Intraoral photographs of the patient with the removable partial denture.
�
The patient wished to rehabilitate the mandible. She had previously undergone lower rehabilitation with a Co-Cr RPD but rarely used it due to finding its framework unaesthetic. Detailed examination of the existing prostheses showed adequate adaptation and retention but visible unaesthetic clasps on abutment teeth.
All possible alternative rehabilitation treatments were explained. Due to financial constraints, the patient agreed to na RPD with a PEEK framework for replacing the missing teeth 36, 44, and 45. The study case was previously approved by the Ethics Committee of the Faculty of Dental Medicine of the University of Lisbon, and the patient�s written informed consente was obtained.
Firstly, both maxillary and mandibular preliminary impressions were taken with an irreversible hydrocolloid impression material (Hydrogum 5, Zhermack, Italy) using a stock tray. After disinfection, the impressions were poured with dental stone Type III (Pro-Solid Super, Pro-Dental, Germany) to obtain the preliminary casts. The mandibular preliminary cast was then fixed on the scanner table and scanned using a 3D scanner (S600 ARTI, Zirkonzahn, Italy) to obtain a digital cast. The lower custom tray was designed (Zirkonzahn.Tray, Zirkonzahn, Italy) and 3D printed (NextDent 5100, 3D SYSTEMS, The Netherlands) with light-polymerizing PMMA resin (NextDent Tray, 3D SYSTEMS, The Netherlands) (Figure 3). The digital cast was surveyed to determine the most acceptable insertion path, and then the survey line was drawn on the abutment teeth, and the retention zones were identified and represented on the cast with a color map (Figure 4).
�
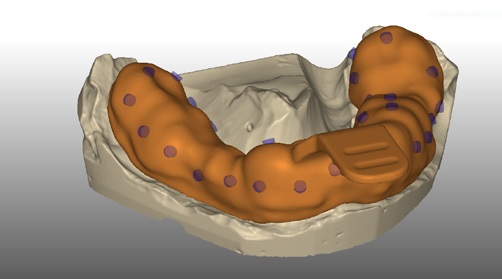
Figure 3. CAD of the custom tray.
�
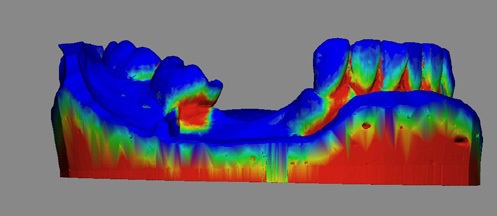
Figure 4. Survey of the preliminary cast with identification of retentive zones.
�
Dental preparations were performed following the design outlined on the preliminary cast to produce guide planes in the distal surface of tooth 35 and the mesial surfaces of teeth 37 and 46. A wear guide indicating the places to be reduced was printed to help with tooth preparations (Figure 5). Occlusal rests in teeth 37, 35, and 46 and cingulum rests in tooth 43 had been done previously, and no improvements were necessary.
�

Figure 5. Printed wear guide.
�
After the dental preparations, a definitive impression was performed with the custom tray and irreversible hydrocolloid impression material (Hydrogum 5, Zhermack, Italy), as well as a preliminary registration with a wax occlusal rim (ANUTEX, kemdent, Purton, UK). This impression was poured with gypsum Type III (Pro-Solid Super, Pro-Dental, Germany) to obtain the master cast. The master casts were scanned (S600 ARTI, Zirkonzahn, Italy) and digitally surveyed according to the selected insertion path. Initially, the software identified the retentive areas in the teeth and soft tissues.
Then, all undesirable undercuts were blocked out into flattened surfaces, and the lingual bar had a relief of 0.2 mm.
The relief was removed where the active ends of the clasps would be placed Figure 6). Because of PEEK�s low elastic modulus compared to Co-Cr alloys, adequate clasp retentive force requires thicker and wider clasp arms, which should be balanced considering the clasp arms� length and the degree of undercuts. A 0.5-mm undercut was used for clasp retention. In this case, retention zones of 0.5 mm were found buccally on teeth 34 and 43 and lingually on teeth 37 and 46 since these were lingualized. The framework was digitally drawn (Zirkonzahn.Partial-Planner, Zirkonzahn, Italy) following the biomechanical principles recommended for this case (Figure 7). The workflow steps to design the framework were followed. The shape of connectors, rests, and clasps followed typical recommendations.
�
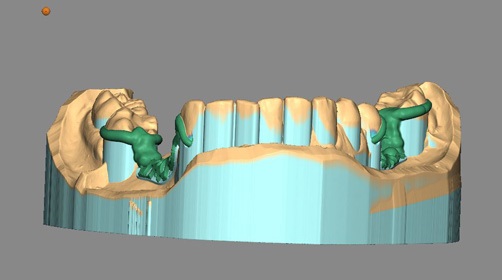
Figure 6. Digital cast with relief of retention �reas except on the places where the clasps end.
�
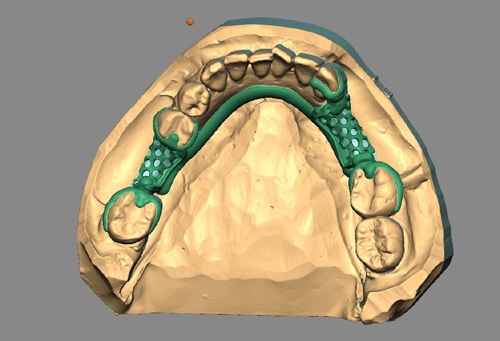
Figure 7. CAD of structure: mesh for resin base retention, major connector, and clasp placement.
�
A try-in resin pattern of the framework was fabricated (Try-In&Burnout Weiss, ZirkonZahn, Italy) using subtractive manufacturing technology to evaluate the fit of the designed framework intraorally before milling the PEEK framework (Figure 8). The visual fit was satisfactory in the patient�s cast and intraorally (Figures 9 and 10). After this positive adaptation test, the framework was milled from PEEK dental disks (Tecno Med; ZirkonZahn, Italy). The milling process took approximately 3 hours. The PEEK framework was then finished with tungsten drills and tried in the patient�s cast and intraorally to check its fit. It had an excellent fitting in the patient�s cast (Figure 11).
�
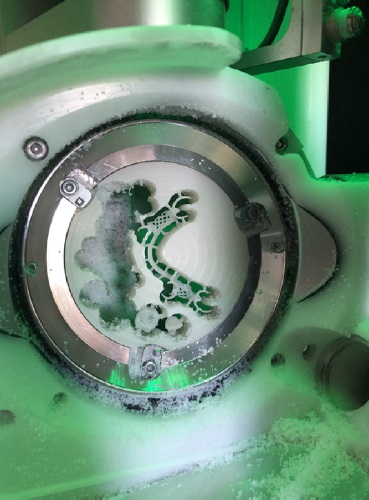
Figure 8. Milling of resin try-in.
�

Figure 9. Try-in in the cast.
�

Figure 10. Intraoral adaptation test of try-in.
�

Figure 11. PEEK structure adaptation in the cast.
�
When tested intraorally, the framework was passive, stable, and well adapted to hard and soft tissues, with only minor occlusal adjustments necessary in the cingular rest of tooth 43 and the occlusal rest of tooth 35 (Figure 12). The wax (Alminax, Kemdent, Kinsale, Ireland) was placed on the metal mesh of the framework, and an interocclusal record was obtained. Both maxillary and mandibular casts were mounted on an articulator (Asa Dental, Massarosa, Italy), and artificial teeth (Stein Vit, New Stetic S.A., Antioquia, Colombia) were arranged.
�

Figure 12. PEEK structure adaptation in the mouth.
�
After the try-in appointment, the RPD was processed with heat-curing acrylic resin (Probase Hot, Ivoclar Vivadent, Liechtenstein) for 6 hours at 80 �C (Figures 13 and 14). The edentulous regions of the PEEK framework were sandblasted with aluminum oxide at 10 μm, 2 bar, and a 10-mm distance prior to the acrylic application. After minor occlusal adjustments in tooth 36, the RPD was delivered to the patient with proper care instructions (Figures 15 and 16).
�

Figure 13. Lateral view of the finished prosthesis.
�
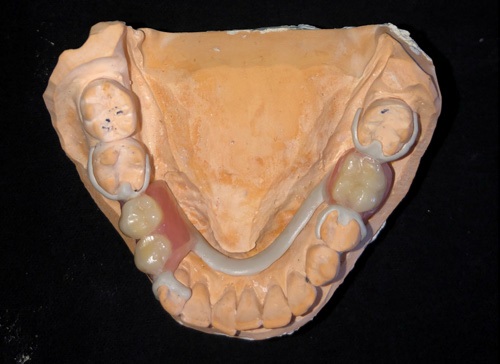
Figure 14. Occlusal view of the finished prosthesis.
�
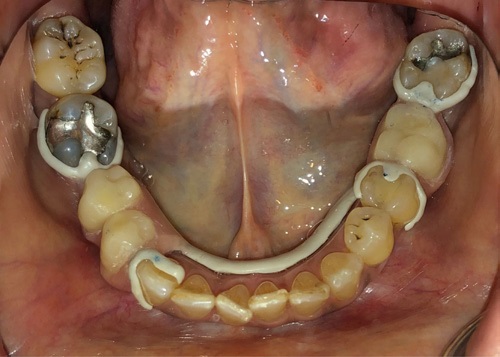
Figure 15. Intraoral view of the finished removable partial denture.
�

Figure 16. Final photograph of the patient.
�
At the post-insertion appointment, the patient had minor pain complaints due to mucosa compression near tooth 36.
The compression zone was relieved after using a pressure indicator paste (Colt�ne PSI, Altst�tten, Switzerland). Good stability and retention were achieved, and the patient was satisfied with the function and aesthetics.
One month later, in the second post-insertion appointment, the patient reported being more comfortable, emphasizing the new prosthesis� lighter weight. When evaluated on a digital balance, the Co-Cr structure prosthesis weighed 7.54 g, while the PEEK structure prosthesis weighed just 3.64 g.
At the 2-year follow-up (Figure 17), the patient mentioned that she was very satisfied with the rehabilitation and used it without complaints of discomfort or a notorious feeling of lack of retention. All prosthesis components were intact, and the PEEK structure showed some extrinsic pigmentation, which was easily removed with polishing, especially evident on the major and minor connectors.
�

Figure 17. 2-year follow-up.
�
Discussion and conclusions
The material for constructing RPDs should be chosen based on clinical examination, patient demands, and scientific evidence. An aesthetically unacceptable display of metal clasps, increased prosthesis weight, metallic taste, and allergic reactions to metals have led to the introduction of several new resin materials in clinical practice.
This case involves a patient with high aesthetic demands. Implants would be the better option, but the patient rejected this treatment due to cost concerns and fear of additional oral surgery. In order to not involve irreversible and complex treatments on teeth adjacent to edentulous spaces, the choice fel on an RPD with a PEEK framework.
PEEK is a high-performance machinable polymer and a promising alternative to conventional Co-Cr frameworks because of its favorable biocompatibility, low weight, and adequate physical, mechanical, and chemical properties.5, 18, 20, 24
However, PEEK has low rigidity compared to conventional Co-Cr alloys (elastic modulus of 3.0�5.5 GPa in PEEK versus >200 GPa in Co-Cr alloys). The need for retention represents a key challenge for the clinical application of PEEK frameworks, so clasps should be thicker and have a deeper undercut to be clinically effective.7, 8, 20 These characteristics make the clasps more bulky and closer to the marginal gingiva. Fortunately, this material has low plaque adhesion, and periodontal issues may not necessarily be a problem.24, 27 Nonetheless, some concerns have arisen about the long-term performance of these clasps and their possible loss of retention. Unlike Co-Cr, one of the main limitations of using PEEK for RPD structures is the inability to adjust the clasps units if necessary.16 Promisingly, studies have shown no decrease in the retention of these clasps after simulated aging in the laboratory.7 26 28
Regarding the final weight of the prosthesis, PEEK is known to have a low density of 1.3 g/cm3, which allows the production of a low-weight RPD structure compared to Co-Cr, with a density of 8.5 g/cm3.29 When both the patient�s RPDs were weighted on a digital scale, the final PEEK prosthesis was approximately 52% lighter than the Co-Cr prosthesis. The patient was pleased with the reduced weight of her new denture. This added value had been previously reported by Zoidis in 2015;5 however, this assessment is not rigorous since the acrylization and the type of teeth were not standardized.
Despite PEEK�s high resistance to fracture,14 no repair protocol for a potential fracture is described in the literature. The impossibility of repair also limits the possibility of adding teeth, which is a major limitation of PEEK. More research is needed on this issue. Another limitation is that the PEEK structure fabrication method is more expensive than that of Co-Cr RPD frameworks and the conventional lost-wax technique. PEEK disks cost around 300 euros and allow the production of only two frameworks. This economic limitation might be overcome when 3D-printed PEEK becomes common. 3D-printed PEEK is finding applications in numerous industries, but most are still in the research phase.30
Finally, we must mention that the final aesthetics achieved are not perfect, as the color of the clasps is whiter and more opaque than the color of the teeth. Other authors described similar results.5, 18, 31
Despite this work�s limitations, we can conclude that PEEK should probably be considered an alternative framework material for patients dissatisfied with the aesthetics of conventional Co-Cr frameworks. Further long-term clinical follow-up, longer than 2 years, is needed to consolidate the scientific data.
Using PEEK to construct an RPD metal-free framework resulted in a prosthesis with adequate fit and good patient satisfaction regarding function and aesthetics. With proper patient selection and treatment planning, milled PEEK can be a useful alternative framework material for RPDs restoring Class III Kennedy edentulous patients.
�
References
1. Gray D, Barraclough O, Ali Z, Nattress B. Modern partial dentures - part 2: a review of novel metal-free materials and innovations in polymers. Br Dent J. 2021;230:813�8.
2. Kim JJ. Revisiting the Removable Partial Denture. Dent Clin North Am. 2019;63:263-78.
3. Bar�metro de Sa�de Oral - Ordem dos M�dicos Dentistas 2023. Available from: https://www.omd.pt/observatorio/barometro/. Accessed 7 Dez, 2023.
4. Campbell SD, Cooper L, Craddock H, Hyde TP, Nattress B, Pavitt SH, et al. Removable partial dentures: The clinical need for innovation. J Prosthet Dent. 2017;118:273-80.
5. Zoidis P, Papathanasiou I, Polyzois G. The use of a modified poly-ether-ether- ketone (PEEK) as an alternative framework material for removable dental prostheses. A clinical report. J Prosthodont. 2016;25:580�4.
6. Ismail H, Abbas F, Gindy N. Clinical Evaluation of Polyoxymethylene Partial Dentures Designed and Fabricated by Using CAD/CAM Technology. Alex Dent J. 2019;44:77-83.
7. Micovic D, Mayinger F, Bauer S, Roos M, Eichberger M, Stawarczyk B. Is the high-performance thermoplastic polyetheretherketone indicated as a clasp material for removable dental prostheses? Clin Oral Investig. 2021; 25:2859�66.
8. Abdel-Rahim N, El-Fattah F, El-Sheikh M. Laboratory comparative study of three different types of clasp materials. Tanta Dent J. 2016;13:41-49.
9. Fueki K, Ohkubo C, Yatabe M, Arakawa I, Arita M, Ino S, et al. Clinical application of removable partial dentures using thermoplastic resin. Part II: material properties and clinical features of non-metal clasp dentures. J Prosthodont Res. 2014;58:71�84.
10. Sampaio-Fernandes M, Galhardo J, Campos S, Oliveira S, Reis-Campos C, Figueiral M. Thermoplastic Materials for Infrastructures in Prosthodontic Rehabilitation: A Review. In: Tavares J, Jorge R. ECCOMAS Thematic Conference on Computational Vision and Medical Image Processing. Porto: Springer; 2019. 606-614.
11. Nandal S, Ghalaut P, Shekhawat H, Gulati M. New era in denture base resins: a review. Dental Journal of Advance Studies. 2013;1:136-43.
12. Schwitalla A, Abou-Emara M, Spintig T, Lackmann J, M�ller W. Finite element analysis of the biomechanical effects of PEEK dental implants on the peri-implant bone. J Biomech. 2015;48:1�7.
13. AL-Rabab�ah M, Hamadneh W, Alsalem I, Khraisat A, Abu Karaky A. Use of High Performance Polymers as Dental Implant Abutments and Frameworks: A Case Series Report. J Prosthodont. 2019;28:365�72.
14. Hossam M, Elshahawy W, Masoud G. Evaluation of Marginal Adaptation and Fracture Resistance of BioHPP and Zirconia. Egypt Dent J. 2018;64:1489-501.
15. Lee KS, Shin JH, Kim JE, Kim JH, Lee WC, Shin SW, et al. Biomechanical Evaluation of a Tooth Restored with High Performance Polymer PEKK Post-Core System: A 3D Finite Element Analysis. Biomed Res Int. 2017;2017:1373127.
16. Tasopoulos T, Chatziemmanouil D, Kouveliotis G, Karaiskou G, Wang J, Zoidis P. PEEK Maxillary Obturator Prosthesis Fabrication Using Intraoral Scanning, 3D Printing, and CAD/CAM. Int J Prosthodont. 2020;33(3):333�40.
17. Chainani P, Paul P, Shivlani V. Recent Advances in Orthodontic Archwires: A Review. Cureus. 2023;15:e47633.
18. Harb I, Abdel-Khalek E, Hegazy S. CAD/CAM Constructed Poly(etheretherketone) (PEEK) Framework of Kennedy Class I Removable Partial Denture: A Clinical Report. J Prosthodont. 2019;28:e595�8.
19. Mayinger F, Micovic D, Schleich A, Roos M, Eichberger M, Stawarczyk B. Retention force of polyetheretherketone and cobalt-chrome-molybdenum removable dental prosthesis clasps after artificial aging. Clin Oral Investig. 2021;25:3141-9.
20. Papathanasiou I, Kamposiora P, Papavasiliou G, Ferrari M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health. 2020;20:217.
21. Zheng Z, Liu P, Zhang X, Xin J, Wang Y, Zou X, et al. Strategies to improve bioactive and antibacterial properties of polyetheretherketone (PEEK) for use as orthopedic implants. Mater Today Bio. 2022;16:100402.
22. Mishra S, Chowdhary R. PEEK materials as an alternative to titanium in dental implants: A systematic review. Clin Implant Dent Relat Res. 2019;21:208-22.
23. Concei��o P, Portugal J, Neves CB. Evaluation of Removable Partial Denture Metal Frameworks Produced by Digital Methods�A Systematic Review. Appl Sci. 2023;13:10824.
24. Lo Russo L, Lo Muzio E, Troiano G, Guida L. Cast-free fabrication of a digital removable partial denture with a polyetheretherketone framework. J Prosthet Dent. 2023;129:262-6.
25. Alqurashi H, Khurshid Z, Syed AUY, Habib SR, Rokaya D, Zafar MS. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J Adv Res. 2020;28:87-95.
26. Muhsin S, Wood J, Johnson A. Effects of novel polyetheretherketone (PEEK) clasp design on retentive force at different tooth undercuts. J Oral Dent Res. 2018;5:13-25.
27. Tannous F, Steiner M, Shahin R, Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater. 2012;28:273�8.
28. Mayinger F, Micovic D, Schleic A, Roos M, Eichberger M, Stawarczyk B. Retention force of polyetheretherketone and cobalt-chrome-molybdenum removable dental prosthesis clasps after artificial aging. Clin Oral Investig. 2021;25:3141-9.
29. Alexakou E, Damanaki M, Zoidis P, Bakiri E, Mouzis N, Smidt G, et al. PEEK high performance polymers: a review of properties and clinical applications in prosthodontics and restorative dentistry. Eur J Prosthodont Restor Dent. 2019;27:113�21.
30. Dua R, Rashad Z, Spears J, Dunn G, Maxwell M. Applications of 3D-Printed PEEK via Fused Filament Fabrication: A Systematic Review. Polymers (Basel). 2021;13:4046.
31. Sun F, Shen X, Zhou N, Gao Y, Guo Y, Yang X, et al. A speech bulb prosthesis for a soft palate defect with a polyetherketoneketone (PEKK) framework fabricated by multiple digital techniques: A clinical report. J Prosthet Dent. 2020;124:495-9.
�
Isabel Gomes
E-mail address: isabel.gomes@fmd.ulisboa.pt
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Isabel Gomes: Conceptualization; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Writing � review & editing. Joana Gon�alves: Data curation, Investigation, Formal analysis, Visualization, Writing � original draft. Jo�o Paulo Martins: Methodology; Supervision; Visualization; Conceptualization; Writing � review & editing. Lu�s Miguel Pires Lopes: Visualization; Conceptualization; Writing � review & editing.
�
1646-2890/� 2024 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
