
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Rev Port Estomatol Med Dent Cir Maxilofac | 2017 | 58 (2) | 91-96
Investigação Original
Resonance frequency analysis by the Osstell system, using the transducer screwed to different healings abutments
Sistema de análise de frequência de ressonância - Osstell, utilizando um transdutor aparafusado a diferentes pilares de cicatrização
a Department of Periodontics and Implant Dentistry, Dental School University of Seville, Seville, Spain.
b Faculty of Health Sciences Fernando Pessoa University, Porto, Portugal.
c Bioengineering Research Center (CREB), Department of Materials Science and Metalurgical Engineering, Universitat Politècnica de Catalunya, Barcelona, Spain.
Mariano Herrero-Climent - mariano@herrerocliment.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 2
Investigação Original
Pages - 91-96
Go to Volume
Article History
Received on 07/10/2016
Accepted on 17/03/2017
Available Online on 16/05/2017
Keywords
Original research
�
Resonance frequency analysis by the Osstell system,
using the transducer screwed to different healings abutments
Sistema de an�lise de frequ�ncia
de resson�ncia � Osstell, utilizando um transdutor
aparafusado a diferentes pilares de cicatriza��o
�
Mariano Herrero-Climenta,*, Carmen Mar�a D�az-Castroa, Carlos Fern�ndez Chereguinia, Carlos Falcaob, Francisco Javier Gilc, Jose Vicente R�os-Santosa
a Department of Periodontics and Implant Dentistry, Dental School University of Seville, Seville, Spain.
b Faculty of Health Sciences Fernando Pessoa University, Porto, Portugal.
c Bioengineering Research Center (CREB), Department of Materials Science and Metalurgical Engineering, Universitat Polit�cnica de Catalunya, Barcelona, Spain.
�
�
http://doi.org/10.24873/j.rpemd.2017.05.015�
ABSTRACT
Objectives: compare the ISQ values obtained by the Osstell ISQ, screwing the Smarpeg directly to the implant or to the new designed healing abutments of 2, 3.5 and 5 mm of height.
Methods: 60 rough surface implants were placed in 4 bovine ribs. 30 standard and 30 prototype implants were divided to group A and B, respectively. All were inserted with a torque of 30 N/cm2, so that the rough/smooth interface was placed at bone crest level (the distance between the implants needed to be at least 4 mm). Primary stability was measured by resonance frequency analysis (RFA) with the Osstell ISQ transducer directly to the implant or over three Smartpeg screwed to the top of three different healing abutments of 2, 3.5 and 5 mm of height.
Results: The mean ISQ of the prototype group is 73.9 � 5.3 and of the standard one is 79.8 � 3.7. The mean ISQ values according to where the Smartpeg is screwed to were 76.2 � 4.47 and 75.69 � 4.7 when the Smartpeg was screwed directly to the implant; 78.2 � 5.78, 77.3 � 5.90, 76.0 � 5.90 when the transducer was screwed to the abutments of 2, 3.5 and 5 mm of height respectively.
Conclusions: It may be concluded from the present investigation that similar ISQ values could be obtained measuring the RFA with the transducer screwed directly to the implant or to healing abutments of different heights, in an accurate and reproducible way. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(2):91-96)
Keywords: Abutment design, Bone implant interface, Dental implants, Osseointegration
�
RESUMO
Objetivos: Comparar os valores de ISQ obtidos pelo sistema Osstell, aparafusando o Smartpeg diretamente ao implante ou a pilares de cicatrizacao com 2, 3,5 e 5 mm de altura.
M�todos: Foram colocados 60 implantes com superficie rugosa em 4 costelas bovinas. 30 implantes standard e 30 implantes prototipo foram dividos em grupo A e B, respetivamente. Todos os implantes foram inseridos com um torque de 30N/cm2, de forma a que a interface entre a superficie rugosa e o colo polido ficasse ao nivel da crista ossea (definiu-se uma distancia entre implantes de pelo menos 4 mm). A estabilidade primaria foi medida atraves do sistema de analise de frequ�ncia de ressonancia (AFR) com o transdutor Osstell ISQ colocado diretamente sobre o implante ou colocado sobre tres pilares de cicatrizacao com alturas de 2, 3,5 e 5 mm, respectivamente.
Resultados: A media de valores de ISQ foi de de 76,2 � 4,47 para o grupo prototipo e de 79,8 � 3,7 no grupo standard. A media de valores de ISQ em funcao de onde o smartpeg foi aparafusado foi de 76,2 � 4,47 e 75,7 � 4,72 quando foi diretamente aparafusado ao implante, e de 78,2 � 5,78, 77,3 � 5,90, 76,0 � 5,90 quando o transdutor se aparafusou aos pilares de 2, 3,5 e 5 mm de altura, respetivamente.
Conclus�o: Pode-se concluir da presente investigacao que se podem obter valores similares de ISQ medindo a AFR com o Smartpeg aparafusado diretamente ao implante, bem como aparafusado aos pilares de cicatrizacao de diferentes alturas, de uma forma precisa e reprodutivel. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(2):91-96)
Palavras-chave: Desenho de pilares, Interface ossoimplante, Implantes dent�rios, Osteointegracao
�
Introduction
Primary implant stability is considered an essential requirement for appropriate implant osseointegration. Maintaining appropriate stability through time is also considered a longterm success guarantee.1,2 Different techniques have been described for non-invasive, clinical evaluation of implant stability.
Resonance Frequency Analysis (RFA) represents a widely used technique for an objective assessment of implant stability at any stage of treatment or follow-up, due to its high reliability and reproducibility.3-8 This technique has been demonstrated to evaluate implant stability as a function of interface stiffness.9 RFA is assessed by the instrument Osstell (Osstell AB, Goteborg, Sweden.). The unit of measure of Osstell is the implant stability quotient (ISQ) and its scale values could vary from 1 to 100. The higher the ISQ number, the higher the stability. Moreover, RFA measurements display the micromobility of dental implants. This micromobility seems to be determined by the bone density at the implant site.10
The ISQ values are influenced by different factors11 as the effective implant length, the distance from the transducer to the marginal bone, (the greater the distance from the transducer to the bone, the lower the ISQ value); 1,6,12,13 the osseous quality;14,15 the force with which the Smartpeg (transducer) is torqued;12,16 the presence of soft tissue between the implant and the transducer;14,16 and the amount of bone in contact with the implant.14
It is well known that the disconnections and subsequent reconnections of the abutment compromise the periimplant tissue stability.17Previous study18 reported that these facts had an impact in the mucosal barrier and resulted in a more apically positioned zone of connective tissue what established a consequent bone resorption.
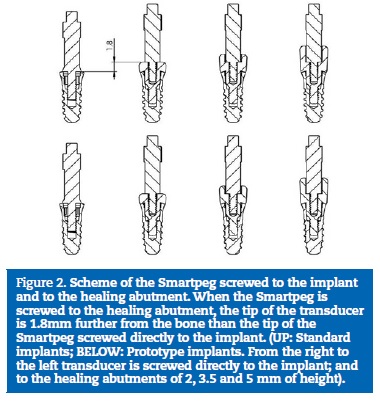
New healing abutments have been designed to allow to directly screwed the Smartpeg to its top part. These healing abutments were developed to avoid the dis/reconnection of the healing abutment to measure the implant stability and to facilitate the ISQ�s registration (since it is not necessary to remove the healing abutment). This also makes the assessment of the stability easier and more convenient for the clinician because the Smartpeg is placed more accessible for the registration (is placed more coronal). Another possible advantage of the new designed abutments is that in cases of low stability, there is no application of counterclockwise forces. So that, implants with no sufficient stability, during the healing time, are no submitted to that force.
The fact of screwing the Smartpeg to the healing abutment and no directly to the implant could affect the ISQ values, as the transducer is torqued farther from the bone than when it is screwed to the implant. That could produce greater vibration of the bone-implant interface and, therefore, the decrease of the ISQ values. For that reason, it is necessary to assess if the ISQ measurements are comparable when using the Smartpeg screwed directly to the implant or to the new healing abutments.
The aim of this trial is to compare the ISQ values obtained by the Osstell ISQ, screwing the Smarpeg to the implant or to the healing abutment. The null hypothesis was that there would be no difference between interventions.
Materials and methods
Sixty rough surface implants (Shot BlastingR: alumina particle sandblasting and acid passivation) screw-shaped implants (EssentialR Cone, Klockner Implant System, Barcelona, Spain) were used. The implants belonged to one of the followinggroups:
� Group A: 30 standard implants. These are an internal connection, double-threaded implants, characterized by an atraumatic apex and a progressive core.
� Group B: 30 prototype implants. These are the same as the standard ones, but the progressive core is 0.2 mm wider and the threads are sharper.
All implants had a diameter of 3.5 mm (diameter at platform level is 4.5 mm), a length of 8 mm and a mechanized collar height of 1.5 mm.
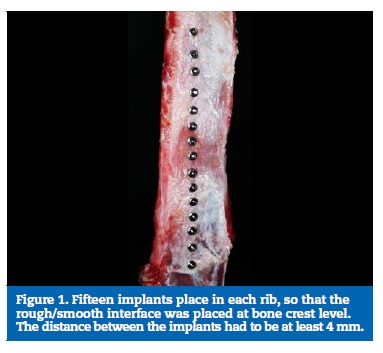
The implants were placed in 4 bovine ribs (bone quality type II19), by a experienced clinician (user and knower of the Klockner Implant System for more than 2 years), following the manufacturer�s protocol. 15 implants were place in each rib.
The osteotomy was performed under abundant irrigation with sterile saline solution 800 rpm. The implants were inserted using the surgical unit, with a torque of 30 N/cm2, so that the rough/smooth interface was placed at bone crest level.
The distance between the implants had to be at least 4 mm (Figure 1).
�
�
�
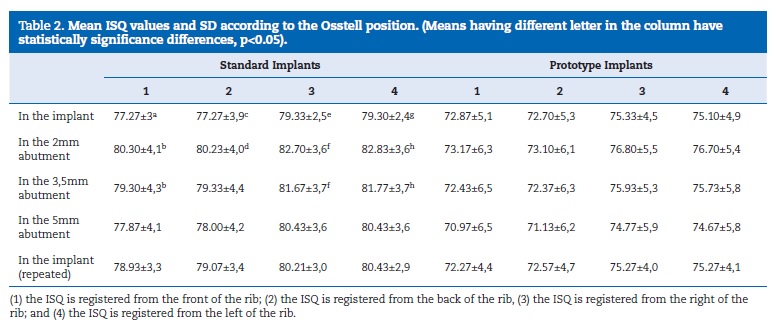
Once the implants were in place, primary stability was measured by means of RFA with the Osstell ISQ in five different situations, by a second experienced clinician in the use of the ISQ device. First, the ISQ was measured over the Smartpeg screwed directly to the implant. Then, it was measured over three Smartpeg screwed to the top of three different healing abutments (2, 3.5 and 5 mm of height). The transducers were screwed by the specific plastic hand-screwdriver. The abutments were torqued to 10 N/cm2 on the implants (with the surgical unit). Finally, the ISQ was measured again over the Smartpeg screwed directly to the implant (to assess the influence of screw/unscrew over the implant stability). One Smartpeg is used for each implant (so 5 measurements were made with each transducer). In each situation, the ISQ was registered perpendicular to the Smartpeg in 4 different positions: (1) the ISQ is registered from the front of the rib; (2) the stability is registered from the back of the rib, (3) the stability is registered from the right of the rib; and (4) the stability is registered from the left of the rib. At each position, the ISQ was registered once.
The healing abutments of 2, 3.5 and 5 mm, in which the Smartpeg are screwed to, are a new design. They have been created to allow the screwing of the Smartpeg in their inner part, so it is placed as close as possible to the bone level (to allow the ISQ measures to be made from a similar point as if the registration were assessed if the Smartpeg were screwed directly to the implant). Despite this, in the three different healing abutments, the Smartpeg is located further from the bone (1.8 mm) than when the Smartpeg is screwed directly to the implants (Figure 2).
�
�
�
SPSS 19.0 software (SPSS, Chicago, IL) was used for the statistical analysis. Mean values and standard deviations were calculated. The normal distribution of the values and the homogeneity of the variances were tested through a Kolmogorov-
Smirnov and Levene tests, respectively. The differences between the mean values were compared with the non-parametric Kruskal-Wallis and Mann-Whitney tests. When significant differences were obtained, 95% confidence intervals were found for average and mean differences (p < 0.05).
Results
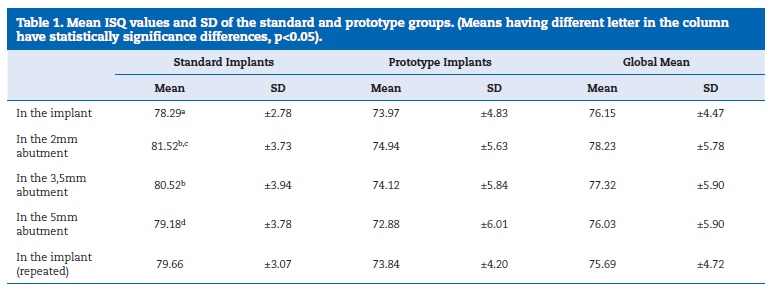
The global mean ISQ of the whole sample was 76.7 � 5.5. The global mean ISQ of the prototype group is 73.9 � 5.3 and of the standard one is 79.8 � 3.7. When the sample were analyzed without having into account which group the implants belong to, the mean ISQ values according to where the Smartpeg is screwed to were 76.2 � 4.47 and 75.7 � 4.72 when the Smartpeg was screwed directly to the implant; 78.2 � 5.78, 77.3 � 5.90, 76.0 � 5.90 when the transducer was screwed to the abutments of 2, 3 and 5 mm of height respectively (Table 1).
�
�
�
The mean ISQ values by groups were also studied (Table 1). In the prototype implants group, no statistically significant differences were found between measuring the stability on the Smartpeg screwed directly to the implant or screwed to different abutments.
However, in the standard implants group statistically significant differences (p < 0.05) were found between measuring the stability on the Smartpeg screwed directly to the implant and screwed to the 2 and 3.5 mm healing abutments (shown in the Table 1 as a-b). Also, statistically significant differences (p < 0.05) were found between measuring the stability on the Smartpeg screwed to the 2 mm healing abutment and to the 5 mm healing abutment (shown in the Table 1 as c-d).
The mean ISQ values related to the position of the Osstell are given in Table 2. No statistically significant differences were found between the different measurements in the prototype implants group; independently of whether they were registered directly to the implant or to the healing abutments.
Nevertheless, in the standard implants group statistically significant differences (p < 0.05) were found between measuring the stability on the Smartpeg screwed directly to the implant and screwed to the 2 mm healing abutments in all the positions (1, 2, 3, 4) (shown in Table 2 as a-b, c-d, e-f, g- h) and between the values registered without healing abutment and 3,5 mm healing abutment, but only in positions 2 and 4 (shown in Table 2 as b-f, b-h).
�
�
�
Data also showed that in both groups, all ISQ values of positions 1 and 2 were statistically equal to each other but statistically different from those of positions 3 and 4 (which were also statistically equal to each other), except for the last situation in the standard group (without healing abutment) in which the 4 values were statistically equal (p < 0.05).Discussion
In the present study, the implant stability was analyzed by RFA with the Osstell ISQ when the Smartpeg was screwed to the implant and to the healing abutments of different heights.
The bone in which the implants were place was type II19. The mean ISQ in our study was 76.7 � 5.5. These results are similar to those of other trials examining the ISQ in cow ribs (also bone quality type II). In 2009, other authors20 found a mean ISQ of 70.86 � 3.4 and 70 � 3.8 when placing two different implants (3.7 x 10 mm ZimmerR Dental and 4x 10 mm Nobel BiocareR) in cow ribs with bone quality type II-III. In 2014, a research was published21 that analyzed the ISQ of three types of implants (two types of straight-screw type implants � one with polished collar and the other one without � and one tapered-screw type implant) placed in cow ribs, bone quality type III. The implants were Straumann, length 10 mm and diameter 3.3 mm. The mean ISQ values were 75.02 � 3.65, 75.98 � 3.00 and 79.83 � 1.85, respectively. The slight differences between the results of those trials and the present one could be due to the different macro design of the implants used. The literature agrees that the most appropriate design is endosseous screw-shaped implants. In 1999, it was found that the implants that achieved the higher primary stability were the 8 mm implants.22 These implants were all placed in posterior lower jaw, where type II bone quality was found in all cases.
The data presented in Table 1 showed that the ISQ from the prototype group was lower. It could be attributed to the design of the prototype implant. The characteristic added to the prototype group made the implant insertion with less friction.
So, if there were less friction between the implant and the bone, the primary stability would be lower.
The results of this trial only showed statistically significant differences in the standard group. In that group the differences were between measuring the stability on the Smartpeg screwed directly to the implant and screwed to the different healing abutments. But in this study the ISQ values registered over the Smartpeg attached to the abutment were higher than the ones registered over the transducer screwed directly to the implant. These results are in disagreement with the previous published literature. In previous investigations a strong correlation (r = 0.94, p < 0.01) was observed between the registered frequency and the height of implantation fixture exposed. According to other authors3 the stiffness of the implant/tissue interface, the distance from the transducer to the first bone contact, the abutment length and the marginal bone resorption have influence in the RFA value.3,23 Our results showed that, despite increasing the bone-transducer distance of 1.8 mm, the ISQ values not decrease but increase.
To our knowledge, we don�t know if these results may have clinical repercussions. More studies are needed to clarify if the bone crest-transducer distance had influence in the ISQ values.
In the prototype group statistically significant differences were not found, probably due to the new design of the threads that block the influence of the bone crest-transducer distance. It could be suggested that in the prototype group the RFA could be analyzed with the Smartpeg screwed directly to the implant or to the healing abutments of different heights.
In the standard group, although statistically significant differences were found in between some groups, that differences were between 2-3 points of ISQ. Several studies provide good indications that the acceptable stability range lies between 55 and 85 ISQ, with an average ISQ level of 70.9,24 All of ISQ values in the standard group are over 78, belonging to the group of high stability.
Conclusions
It may be concluded from the present investigation that similar ISQ values could be obtained measuring the RFA with the transducer screwed directly to the implant or to healing abutments of different heights, in an accurate and reproducible way.
�
References
1. Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Resonance Frecuency measurements of implant stability in vivo. A cross- sectional and longitudinal study of the resonance frecuency measurements on implants in the edentulous and partially dentate maxilla. Clin Oral Impl Res. 1997;8:226-33.
2. Glauser R, Sennerby L, Meredith N, Ree A, Lundgren A, Gottlow J et al. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs. failing implants. Clin Oral Implants Res. 2004;15:428-34.
3. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996;7:261-7.
4. Garg AK. Osstell Mentor: measuring dental implant stability at placement, before loading, and after loading. Dent Implantol Update. 2007;18:49-53.
5. Ersanli S, Karabuda C, Beck F, Leblebicioglu B. Resonance frequency analysis of one-stage dental implant stability during the osseointegration period. J Periodontol 2005;76:1066-71.
6. O�Sullivan D, Sennerby L, Jagger D, Meredith N. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004;6:48-57.
7. Herrero-Climent M, Santos-Garcia R, Jaramillo-Santos R, et al. Assessment of Osstell ISQ�s reliability for implant stability measurement: a cross-sectional clinical study. Med Oral Patol Oral Cir Bucal. 2013;18:e877-82.
8. Jaramillo R, Santos R, Lazaro P, et al. Comparative analysis of 2 resonance frequency measurement devices: Osstell Mentor and Osstell ISQ. Implant Dent. 2014;23:351-6.
9. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications Periodontol 2000. 2008;47:51-66.
10. Pagliani L1, Sennerby L, Petersson A, Verrocchi D, Volpe S, Andersson P. l. The relationship between resonance frequency analysis (RFA) and lateral displacement of dental implants: an in vitro study. J Oral Rehabil. 2013;40:221-7.
11. Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants A review of the literature. Int J Prosthodont. 1998;11:408-20.
12. Friberg B, Sennerby L, Linden B, Grondahl K, Lekholm U. Stability measurements of one-stage Branemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999;28:266-72.
13. Sim CP, Lang NP. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin Oral Implants Res. 2010;21:598-604.
14. Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P.The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implants Res. 1997;8:234-43.
15. Bischof M1, Nedir R, Szmukler-Moncler S, Bernard JP, Samson J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin Oral Implants Res. 2004;15:529-39.
16. Friberg B, Sennerby L, Meredith N, Lekholm U. A comparison between cutting torque and resonance frecuency measurements of maxillary implants. A 20 month clinical study. Int J Oral Maxillofac Surg. 1999;28:297-303.
17. Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997;24:568-72.
18. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006; 26:9-17.
19. Lekholm U, Zarb G. Patient selection and preparation. In: Branemark P, Zarb G, Albrektsson T, ed. Tissue-Integrated Prostheses. Osseointegration in Dentistry, 1st ed. Chicago, Quintessence Publishing Co., Inc. 1985:199-209.
20. Andres-Garcia R, Vives NG, Climent FH, et al. In vitro evaluation of the influence of the cortical bone on the primary stability of two implant systems. Med Oral Patol Oral Cir Bucal. 2009;14:E93-7.
21. Romanos GE, Ciornei G, Jucan A, et al. In vitro assessment of primary stability of StraumannR implant designs. Clin Implant Dent Relat Res. 2014;16:89-95.
22. Misch CE. Implant design considerations for the posterior regions of the mouth. Implant Dent. 1999;8:376-86.
23. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11:491-501.
24. Östman Po, hellman M, Sennerby L. Direct implant loading in the edentulous maxilla using a bone density-adapted surgical protocol and primary implant stability criteria for inclusion. Clin Implant Dent Relat Res. 2005; 7(Suppl 1):S60-9.
�
Mariano Herrero-Climent
E-mail address: mariano@herrerocliment.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflicts of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 7 October 2016
Accepted 17 March 2017
Available online 16 May 2017
