
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2023 | 64 (1) | 12-19
Original research
Mechanical and surface properties of a 3D-printed dental resin reinforced with graphene
Propriedades mecânicas e de superfície de uma resina dentária para impressão 3D reforçada com grafeno
a Universidade Católica Portuguesa, Faculdade de Medicina Dentária, Viseu, Portugal
b Escola Superior de Tecnologia e Gestão, Instituto Politécnico de Viseu, Viseu, Portugal
c INEGI – Instituto de Ciência e Inovação em Engenharia Mecânica e Engenharia Industrial, Porto, Portugal
d Universidade do Porto, Faculdade de Engenharia, Porto, Portugal
e Universidade do Porto, Faculdade de Medicina Dentária, Porto, Portugal
Helena Salgado - hsalgado@ucp.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 64
Issue - 1
Original research
Pages - 12-19
Go to Volume
Article History
Received on 10/10/2022
Accepted on 28/02/2023
Available Online on 31/03/2023
Keywords
Original Research
�
Mechanical and surface properties of a 3D-printed dental resin reinforced with graphene
Propriedades mec�nicas e de superf�cie de uma resina dent�ria para impress�o 3D refor�ada com grafeno
�
Helena Salgado1,* 0000-0001-9134-6688
Joana Fialho2 0000-0002-3910-8292
Marco Marques3 0000-0002-7999-1892
M�rio Vaz4 0000-0002-6347-9608
Maria Helena Figueiral5 0000-0001-8583-8096
Pedro Mesquita5 0000-0003-0735-2482
1 Universidade Cat�lica Portuguesa, Faculdade de Medicina Dent�ria, Viseu, Portugal
2 Escola Superior de Tecnologia e Gest�o, Instituto Polit�cnico de Viseu, Viseu, Portugal
3 INEGI � Instituto de Ci�ncia e Inova��o em Engenharia Mec�nica e Engenharia Industrial, Porto, Portugal
4 Universidade do Porto, Faculdade de Engenharia, Porto, Portugal
5 Universidade do Porto, Faculdade de Medicina Dent�ria, Porto, Portugal
�
�
Article history:
Received 10 October 2022
Accepted 28 February 2023
Available online 30 March 2023
�
Abstract
Objectives: Commercial photocurable polymers used in dental additive manufacturing still have mechanical limitations. The incorporation of graphene may provide interesting advantages in this field. This study aimed to evaluate in vitro the effect of adding graphene nanoparticles to a 3D-printed polymethylmethacrylate dental resin in terms of surface roughness, flexural properties, and hardness.
Methods: A 3D-printed dental resin (Dental Sand, Harz Lab) was loaded with four diferente graphene nanoplatelet (Graphenest) concentrations: 0.01wt%, 0.1wt%, 0.25wt%, and 0.5wt%. The neat resin was used as the control group. The surface roughness was measured with a contact profilometer using bar-shaped specimens (50x10x4mm). The flexural strength of specimens (80x10x4mm) from each group was calculated using the 3-point bending test in a Universal Test Machine. Hardness shore D was measured using a manual durometer on round-shaped specimens (12x6mm). Data were evaluated using the Kruskall-Wallis test followed by post-hoc Bonferroni corrected pairwise inter-group comparisons. Statistical significance was set at p<0.05.
Results: Graphene improved 3D-printed PMMA resin hardness with statistical significance at a concentration of 0.01wt% (p=0.043). Surface roughness increased with graphene concentrations above 0.01wt%, with statistically significant differences at 0.25wt% (p=0.006) and 0.5wt% (p=0.005) concentrations. Flexural properties worsened with increased graphene concentrations, and these differences were significant in the concentrations of 0.25wt% (p=0.028) and 0.5wt% (p=0.006).
Conclusions: The use of graphene as a mechanical reinforcement nanomaterial seems to be viable at low concentrations without prejudice to the surface roughness of a 3D-printed polymethylmethacrylate resin.
Keywords: Flexural strength, Graphene oxide, Hardness, Polymethylmethacrylate, Three-dimensional printing
�
Resumo
Objetivos: As resinas para impress�o 3D em Medicina Dent�ria apresentam ainda limita��es mec�nicas. A adi��o de grafeno pode colmatar esse problema. O objetivo deste trabalho foi avaliar in vitro o efeito do grafeno numa resina de polimetilmetacrilato para impress�o 3D ao n�vel da rugosidade de superf�cie, propriedades de flex�o e dureza.
M�todos: Uma resina para impress�o 3D foi aditivada com quatro concentra��es de grafeno: 0,01wt%, 0,1wt%, 0,25wt% e 0,5wt%. A resina pura foi usada como controlo. A rugosidade de superf�cie foi medida com um profil�metro de contacto em provetes retangulares (50x10x4mm). A resist�ncia � flex�o dos provetes (80x10x4mm) foi calculada usando o teste
de flex�o em 3 pontos numa m�quina de teste universal. A dureza shore D foi medida em provetes circulares (12x6mm) com um dur�metro manual. Os resultados foram avaliados utilizando o teste de Kruskal Wallis seguido do teste post-hoc de Bonferroni para compara��es entre grupos. Valores de p<0,05 foram considerados estatisticamente significativos.
Resultados: O grafeno demonstrou melhorar a dureza da resina de polimetilmetacrilato em baixas concentra��es, com significado estat�stico na concentra��o de 0,01wt% (p=0,043). A rugosidade de superf�cie apresentou valores superiores � resina normal para concentra��es de grafeno acima de 0,01wt%. Verificaram-se diferen�as estatisticamente significativas nas concentra��es de 0,25 (p=0,006) e 0,5wt% (p=0,005). As propriedades de flex�o pioraram com o aumento de grafeno, sendo essas diferen�as significativas nas concentra��es de 0,25 (p=0,028) e 0,5wt% (p=0,006).
Conclus�es: O uso do grafeno como refor�o mec�nico de uma resina de polimetilmetacrilato impress�o 3D parece vi�vel em baixas concentra��es, sem prejudicar a rugosidade de superf�cie.
Palavras-chave: Resist�ncia � flex�o, �xido de grafeno, Dureza, Polimetilmetacrilato, Impress�o 3D
�
Introduction
Polymers are widely used in dental prostheses, including complete and partial removable dentures, provisional prostheses, and implant-supported prostheses. Moreover, polymethyl methacrylate (PMMA) is still the most common material in dental prostheses fabrication.1 - 4
The use of CAD/CAM technologies in dentistry has been gaining increasing importance due to its ability to produce various shapes that conform to any biological site. Developments in computer technology and software applications are a relevant part of the groundswell of technological change that has led additive manufacturing technique � 3D printing � to where it is today.5 - 9 3D printers based on vat photopolymerization, namely stereolithography (SLA) and digital light projection (DLP), were the first commercially available and are still among the most used.10, 11
The emergence of these new technologies led to the development of new suitable materials.12 However, the compatible photosensitive acrylic resins limit the application of vat polymerization due to their high volume shrinkage, poor mechanical properties, and low thermal properties.13 - 16 Compared to traditional PMMA resin, 3D-printed PMMA resin demonstrated lower values of flexural strength, modulus of elasticity, and fracture toughness.17 - 22 Therefore, there is na increasing interest in improving commercially available 3D-printed resins by modifying and adapting their mechanical properties to emerging biomedical engineering applications.23 - 27 A promising way to modify and tailor 3D-printed resins� properties could be through the dispersion of nanomaterials in the resin.28, 29
In current dentistry, using a PMMA resin with good mechanical properties for prosthesis fabrication is increasingly important.30 - 32 Consequently, there is a search for a suitable nanofiller that can provide increased mechanical performance without compromising the remaining physical and biological properties.33 Some studies34,35 have demonstrated that surfasse roughness significantly influenced the extent of microbial adhesion to the denture base. Thus, changes in this importante clinical variable might significantly influence bacterial adhesion and retention.35 - 38
Recent developments in nanotechnology have enabled the use of graphene as a reinforcement phase in several polymers, including PMMA resins.39 This new strategy was developed to improve acrylic resins� mechanical and biological drawbacks.40
Graphene is a crystalline form of carbon isolated from graphite,41 characterized by excellent mechanical, thermal, and electric properties.42, 43 Despite the expected benefits of using graphene in dental applications, its mechanical behavior should be understood to anticipate clinical performance and risk of failure.44 The effects of graphene reinforcement on the properties of 3D-printed PMMA dental resin have not been investigated.
Therefore, this investigation aims to study the effect of graphene reinforcement on the surface roughness and mechanical properties of a commercially available 3D-printed PMMA dental resin. The null hypothesis is that adding graphene does not change PMMA resin�s surface roughness, hardness, and flexural strength.
Material and Methods
Graphene nanoplatelets (GNPs) (Graphenest Advanced Nanotechonoly �, Aveiro, Portugal) with a 3�10-nm thickness and 8�30 layers with 0.5-2-μm lateral dimensions were added to Dental Sans resin (HARZ Labs� Inc., Russia) � a photosensitive liquid mixture of methacrylate oligomers and monomers used for temporary crowns and bridges. The corresponding neat resin was used as the control group (G0). Four groups with different graphene concentrations were studied: 0.01wt% (G0.01), 0.1wt% (G0.1), 0.25wt% (G0.25), and 0.5wt% (G0.5).
GNPs were homogeneously mixed in the resin for 1 hour in total darkness in a high-power ultrasonic mixer to ensure their dispersion (375 w/L@40kHz). Then, GNPs� presence in the polymer resin at different concentrations was assessed through Raman spectroscopy. The samples� Raman spectra, with and without GNPs, were recorded in the 1400�2800-nm wavenumber range using a Horiba LabRAM HR Evolution confocal microscope (Horiba� Scientific, Longjumeau, France) equipped with a 532-nm (2.33 eV) laser.
All specimens were virtually designed in the CAD software Chitubox (CDB-Tech�, China) (Figure 1), and the corresponding CAD standard tessellation language (STL) files were sent to the 3D printer. Then, the specimens were 3D printed using a stereolithography printer with LCD technology (Phrozen� Mini 4K, Prozen, Taiwan) equipped with a 405-nm laser to cure the liquid polymer resin (Figures 2 and 3). The printing direction was 45�, and the layer resolution was 0.05 mm. The printed material had a density of 1.20 g/cm3 and a viscosity of 1.2 Pa.s. The addition of graphene did not change these polymer�s properties appreciably.
�
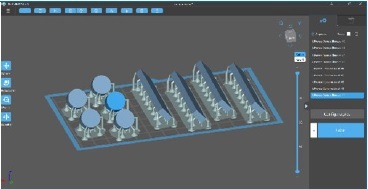
Figure 1. CAD design of specimens.
�
Figure 2. 3D printer.
�

Figure 3. Specimens after the printing process.
�
After printing, all specimens were cleaned using a 90% isopropyl alcohol bath in a post-processing machine (Creality3D� UW-02, Creality, China) for 5 minutes to remove unreacted resin according to the manufacturer�s indications. Then, the specimens were placed in an oven at 80�C for 30 minutes (POLEKO� Aparatura, Wodzisław Śląski, Poland) for post-print baking.
Post-polymerization was performed in a UV-light curing unit for 10 minutes (Creality3D� UW-02, Creality, China). Afterward, the support structures were removed using low-speed rotary instruments (5000 rpm).
Finally, the specimens were finished, polished, and measured using a digital caliper with a 0.01-mm resolution (ABSOLUTE� Digimatic Caliper Series 551, Mitutoyo Europe GmbH) to ensure conformity to the ISO 20795-1�s dimensional thresholds.
After measurements, all specimens were disinfected using 70% ethanol for 5 minutes,45 and were stored under 37�C water for 24 h according to ISO 20795-1.46
Flexural properties were studied in 15 bar-shaped specimens (80x10x4mm) according to ISO standard 178: Plastics - Determination of Flexural Properties.47 Three-point bending tests were performed on graphene-polymer resin specimens using a universal testing machine (Electropuls� E1000, Instron, USA) with a 10-kN load cell and a crosshead speed of 1mm/min. The distance adjusted to provide support to the specimens was 60 mm. The flexural strength of each type of graphene-polymer composite was obtained by averaging the test results of three separate specimens to reduce random errors in specimen preparation and experimental measurement.
The Shore D hardness of each resin group (n=5) was measured using a manual analog durometer (Sauter� HBD 100-0, Sauter GmbH, Wut�schingen, German) on round-shaped specimens (12x6mm) according to ASTM D2240.48 The specimen was placed under the indenter area with a 50-N load for 15 seconds of measurement. The values obtained were analyzed on a scale of 0-100 shores of hardness, with higher values indicating a harder material. Three measurements were performed at different locations on each specimen, and mean values were calculated.
The surface roughness profile was measured in 25 barshaped (50x10x4 mm) specimens, five of each group, using a contact profilometer (HommelWerke� LV � 50, Hommelwerke, Germany). The profilometer�s diamond tip had a 5-μm radius and ran the specimen�s surface, under constant load, following a straight measurement distance of 4.8 mm for 10 seconds. Three measurements were performed in each specimen. The average roughness was analyzed as Ra (μm): the arithmetic mean value of all heights (peaks and valleys) in a given roughness profile.
The statistical significance of the three properties analyzed was determined by the Kruskal-Wallis analysis of variance with a Bonferroni post-hoc test using the software Statistical Package for the Social Sciences (SPSS 25.0, Chicago, IL, USA). Statistical significance was set at p<0.05.
Results
Raman spectroscopy was performed to identify and evaluate the quality and structural properties of the graphene according to the intensity, frequency, and line width of Raman modes G, D, and 2D. Two main peaks characterize the Raman spectra of monolayer graphene: the primary in-plane vibrational mode, G (~ 1580 cm^-1), and 2D (~2690 cm^-1) a second overtone of a different out-of-plane vibration, D (~1350 cm^-1) (Figure 4). Raman spectroscopy results showed that GNPs consisted mainly of few-layer graphene and that photopolymerized resin was primarily PMMA. Raman spectra indicated the presence of graphene in every sample and no evidente change in the typical graphene caused by its introduction into the resin system (Figure 5).
�
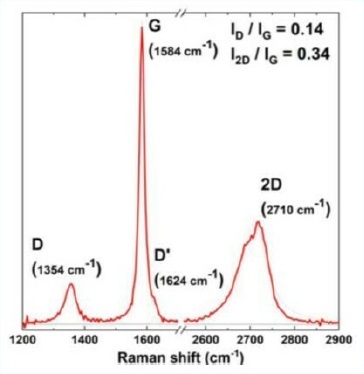
Figure 4. Raman spectra of pristine graphene powder.
�
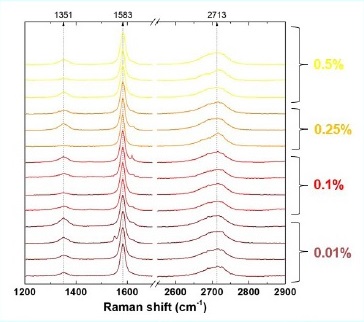
Figure 5. Raman spectra of graphene present at four concentrations in the reinforced resins.
�
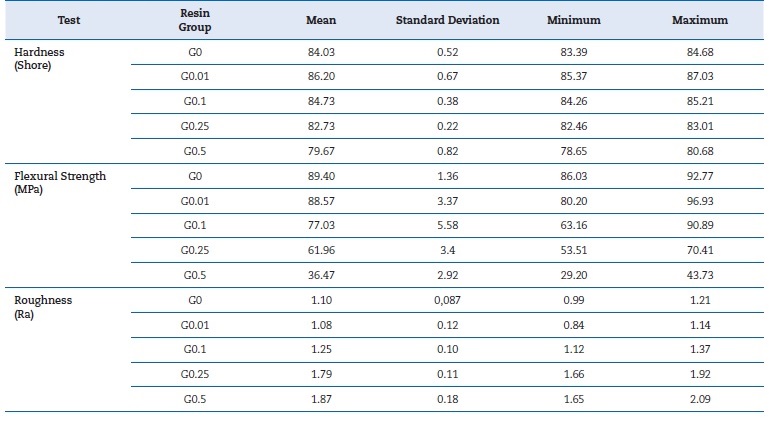
Table 1 shows the descriptive analysis results regarding hardness, flexural strength, and surface roughness per resin group. All graphene groups except the one with the lowest concentration influenced flexural strength negatively, with a statistically significant decrease in the 0.25wt% (p<0.028) and 0.5wt% (p<0.003) concentrations compared to the control (Figure 6). The two lowest concentrations of graphene (0.01wt% and 0.1wt%) increased the resin�s hardness, but only the lowest (0.01wt%) showed a statistically significant difference (p<0.043).
�
Table 1. Mean, standard deviation, minimum and maximum values of hardness, flexural strength, and surfasse roughness per resin group.
�
Higher concentrations (0.25wt% and 0.5wt%) had the opposite effect, with the 0.5wt% concentration causing a statistically significant decrease in hardness (p<0.022) (Figure 7). Surface roughness increased with the increase of graphene concentration, with statistically significant differences in the 0.25wt% (p<0.006) and 0.5wt% (p<0.005) concentrations (Figure 8).
�
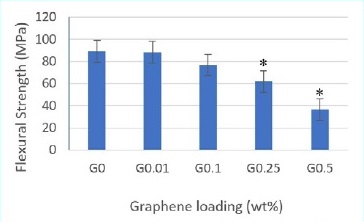
Figure 6. Flexural strength mean values by three-point bending test. Asterisks (*) indicate statistical significance compared to G0 (p<0.05).
�
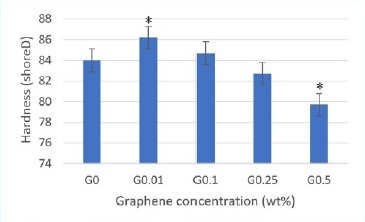
Figure 7. Hardness shore D mean values. Asterisks (*) indicate statistical significance compared to G0 (p<0.05).
�
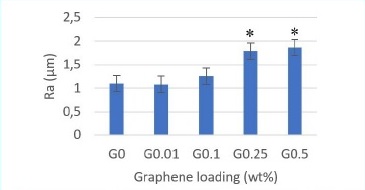
Figure 8. Mean values of surface roughness. Asterisks (*) indicate statistical significance compared to G0 (p<0.05)
�
Discussion
The mechanical properties of dental materials play a crucial role in their clinical performance and are strongly related to both processing and composition. Improving resistance by enhancing acrylic resins� mechanical properties is an important subject that has hardly been investigated.49, 50 Some studies,51 - 61 investigated graphene-reinforced PMMA dental resins, but very little research has focused on vat polymerization for resin�s reinforcement with graphene for biomedical applications.57
An acrylic prosthesis� flexural behavior is one of its most important mechanical properties. In the present investigation, incorporating graphene in concentrations higher than 0.1wt% affected flexural strength negatively. This finding agrees with two investigations that verified that graphene did not improve the resin�s flexural properties.52, 56 In turn, Lee et al.54 found that incorporating only 0.5wt% of graphene oxide (GO) enhanced flexural strength significantly, while higher GO concentrations (1wt% and 2wt%) showed a decrease in flexural strength values. These contradictory results may derive from the different methods used in these studies to add graphene to resin and to simulate the oral environment before the bending tests. Di Carlo et al.51 and Agarwalla et al.55 observed a significantly higher mechanical strength in the graphene-reinforced resin G-CAM, but the percentage of graphene was unknown, which may explain the different results. In a recente study, Punset et al.60 revealed that G-CAM�s graphene concentration was 0.027% by weight � a low concentration. These findings agree with the present study�s results, as a low graphene concentration (0.01wt%) provided a flexural strength similar to that of neat resin. Other studies have shown a greater improvement in polymers� mechanical properties with low graphene concentrations.61, 62 An et al.61 even demonstrated that flexural strength worsened at graphene concentrations greater than 0.1wt%.
Hardness indicates a material�s extent of resistance to plastic deformation.63, 64 Lee et al.56 evaluated this mechanical property in a conventional PMMA dental resin reinforced with graphene at 0.25wt%, 0.5wt%, 1wt%, and 2wt% concentrations and verified that adding graphene significantly increased the resin�s hardness. Agarwalla et al.55 and Punset et al.60 studied the influence of graphene reinforcement in the PMMA pre-polymerized dental resin G-CAM and found that hardness was similar to neat PMMA. In the present investigation, the resin�s hardness increased at graphene concentrations of 0.01wt% and 0.1wt% but decreased and was lower than the control�s in higher concentrations (0.25wt% and 0.5wt%). These different results may be explained by the diferente kinds of resin used in the three studies, which entail different processing techniques and, likely, a different influence of graphene.
Furthermore, there is a lack of knowledge about the influence of graphene on the UV polymerization reaction. One study reported reduced maximum curable thickness per scan when graphene was incorporated into photocurable resins.65
The addition of nanomaterials into the resin causes the photo-initiator and the nanomaterial to compete for light absorption.
This competition usually leads to a less effective UV polymerization process, which may explain the poor mechanical results obtained in the present investigation with graphene concentrations greater than 0.1wt%. Lopez de Armentia et al.57 revealed that incorporating 0.1wt% of graphene into the photocurable resin caused a notable negative effect on printability, potentially influencing the quality of the printed object.
Surface roughness is a factor of clinical relevance since it directly or indirectly affects microbial plaque�s retention in tissues in contact with the materials, increasing the risk of surface fatigue and decreasing their biocompatibility.66, 67 In the present investigation, graphene increased the resin�s surfasse roughness. This result agrees with other studies,55, 58 and may result from graphene�s struggle to disperse in a polymer matrix, which may cause agglomerates of increased graphene concentration.
This study�s null hypothesis was rejected because statistically significant differences were verified between the neat PMMA dental resin and the graphene-reinforced resins in the different properties studied: flexural strength, hardness, and surface roughness.
One limitation of this in vitro study could be that the mechanical tests were not performed in conditions similar to the oral cavity. It is important to understand the effect of graphene�s presence in resin in the long term while in function.
We aim to repeat these mechanical tests after thermocycling cycles in future studies. More studies are required to understand the fracture and deformation mechanisms better and consolidate these experimental observations.
Conclusions
Considering the limitations of this study, we conclude that low concentrations of graphene seem to improve the resin�s hardness without compromising its surface roughness and
flexural strength. Higher concentrations of graphene tend to worsen these properties. More studies are required to evaluate other conditions and different parameters.
�
References
1. Pratap B, Gupta R, Bhardwaj B, Nag M. Resin based restorative dental materials: Characteristics and future perspectives. Jpn Dent Sci Rev. 2019;55: 126�38.
2. Alp G, Johnston WM, Yilmaz B. Optical properties and surfasse roughness of prepolymerized poly (methyl methacrylate) denture base materials. J Prosthet Dent. 2019;121:347-52.
3. Gungor H, Gundogdu M, Duymus ZY. Investigation of the effect of different polishing techniques on the surfasse roughness of denture base and repair materials. J Prosthet Dent. 2014;112:1271-7.
4. Sahin O, Koroglu A, Dede D�, Yilmaz B. Effect of surfasse sealant agents on the surface roughness and color stability of denture base materials. J Prosthet Dent. 2016;116:610-16.
5. Sun Z. 3D printing in medicine: current applications and future directions. Quant Imaging Med Surg. 2018;8:1069-77.
6. Dawood A, Marti B, Sauret-Jackson V, Darwood A. 3D printing in dentistry. Br Dent J. 2015;219:521-9.
7. Pillai S, Upadhyay A, Khayambashi P, Farooq I, Sabri H, Tarar M, et al. Dental 3D-Printing: Transferring Art from the Laboratories to the Clinics. Polymers (Basel). 2021;13:157.
8. Dodziuk H. Applications of 3D printing in healthcare. Kardiochir Torakochirurgia Pol. 2016;13:283-93.
9. Concei��o, PR, Franco M, Alves N, Portugal J, Neves CB. Fit accuracy of removable partial denture metal frameworks produced by CAD-CAM - a clinical study. Rev Port Estomatol Med Dent Cir Maxilofac. 2021;62:194-200.
10. Borrello J, Nasser P, Iatridis JC, Costa K. 3D Printing a Mechanically-Tunable Acrylate Resin on a Commercial DLP-SLA Printer. Addit Manuf.2018;23:374�80.
11. Schweiger J, Edelhoff D, G�th JF. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J Clin Med. 2021;10:2010.
12. Hata K, Ikeda H, Nagamatsu Y, Masaki C, Hosokawa R, Shimizu H. Development of Dental Poly(methyl methacrylate)-Based Resin for Stereolithography Additive Manufacturing. Polymers (Basel). 2021;13:4435.
13. Manapat JZ, Chen QY, Ye PR, Advincula RC 3D Printing of polymer nanocomposites via stereolithography. Macromol Mater Eng. 2017;302:1600553.
14. Karalekas D, Aggelopoulos A. Study of shrinkage strains in a stereolithography cured acrylic photopolymer resin. J Mater Process Technol. 2003;136:146-50.
15. Fuh JYH, Lu L, Tan CC, Shen ZX, Chew S. Processing and characterising photo-sensitive polymer in the stereolithography process. J Mater Process Technol. 1999;89-90:211-7.
16. Dewaele M, Truffier-Boutry D, Leloup G, Devaux J. Volume contraction in photocured dental resins: the shrinkage-conversion relationship revisited. Dent Mat J. 2006;22:359-65.
17. Al-Dwairi ZN, Al Haj Ebrahim AA, Baba NZ. A comparison of the surface and mechanical properties of 3D printable denture-base resin material and conventional polymethylmethacrylate (PMMA). J Prosthodont. 2022;4:1-9.
18. Prpić V, Schauperl Z, Catic A, Dulcic N, Cimic S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J Prosthodont. 2020;29:524-8.
19. Perea-Lowery L, Gibreel M, Vallittu PK, Lassila LV. 3D-printed vs heat-polymerizing and autopolymerizing denture base acrylic resins. Materials (Basel). 2021;14:5781.
20. Gad MM, Fouda SM, Abualsaud R, Alshahrani FA, Al-Thobity AM, Khan SQ, et al. Strength and surface properties of a 3D-printed denture base polymer. J Prosthodont. 2022;31:412-8.
21. Neves C, Chasqueira F, Rebelo P, Fonseca M, Portugal J, Bettencourt A. Microhardness and flexural strength of two 3D-printed denture based resins. Rev Port Estomatol Med Dent Cir Maxilofac 2022;63:198-203.
22. Rijo I, Pedro D, Costa J, Bettencourt A, Portugal J, Neves CB. Chlorhexidine loading of acrylic reline resins � Microhardness and flexural strength after thermal aging. Ver Port Estomatol Med Dent Cir Maxilofac. 2018;59:154-61.
23. Ciancalepore C, Moroni F, Messori M, Bondioli F. Acrylate-Based Silver Nanocomposite by Simultaneous Polymerization Reduction Approach via 3D Stereolithography. Composites Communications. 2017;6:11�6.
24. Szaloki M, Gall J, Bukovinszki K, Borbely J, Hegedus C. Synthesis and Characterization of Cross-Linked Polymeric Nanoparticles and their Composites for Reinforcement of Photocurable Dental Resin. React Funct Polym. 2013;73:465-73.
25. dos Santos MN, Opelt CV, Lafratta FH, Lepienski C, Pezzin S, Coelho L. Thermal and Mechanical Properties of a Nanocomposite of a Photocurable Epoxy-Acrylate Resin and Multiwalled Carbon Nanotubes. Mater Sci Eng A. 2011;528(13-14):4318-24.
26. Zhang J, Huang D, Liu S, Dong X, Li Y, Zhang H et al.. Zirconia Toughened Hydroxyapatite Biocomposite Formed by a DLP 3D Printing Process for Potential Bone Tissue Engineering. Mater Sci Eng C. 2019;105:110054.
27. Markandan K, Lai CQ. Enhanced Mechanical Properties of 3D Printed Graphene-Polymer Composite Lattices at Very Low Graphene Concentrations. Compos Part A Appl Sci Manuf. 2020;129:105726.
28. Duan Y, Zhou Y, Tang Y, Li D. Nano-TiO2-modified photosensitive resin for RP. Rapid Prototyp J. 2011;17:247-52.
29. Szaloki M, Gall J, Bukovinszki K, Borbeli J, Hegedus C. Synthesis and characterization of cross-linked polymeric nanoparticles and their composites for reinforcement of photocurable dental resin. React Funct Polym. 2013;73:465�73.
30. Aguirre BC, Chen JH, Kontogiorgos ED, Murchison DF, Nagy WW. Flexural strength of denture base acrylic resins processed by conventional and CAD-CAM methods. J Prosthet Dent. 2020;123:641-6.
31. Diaz-Arnold AM, Vargas MA, Shaull KL, Laffoon JE, Qian F. Flexural and fatigue strengths of denture base resin. J Prosthet Dent. 2008;100:47-51.
32. Farina A, Cecchin D, Soares R, Botelho A, Takahashi J, Mazzetto M, et al. Evaluation of Vickers hardness of diferente types of acrylic denture base resins with and without glass fibre reinforcement. Gerodontology. 2012;29:e155-60.
33. Costa J, Bettencourt A, Madeira A, Nepomuceno L, Portugal J, Neves CB. Surface properties after chemical aging of chlorhexidine delivery systems based on acrylic resin. Ver Port Estomatol Med Dent Cir Maxilofac. 2019;60:155-62.
34. Pasmore M, Todd P, Pfiefer B, Rhodes M, Bowman CN. Effect of polymer surface properties on the reversibility of attachment of Pseudomonas aeruginosa in the early stages of biofilm development. Biofouling. 2002;18:65-71.
35. Terada A, Yuasa A, Kushimoto T, Tsuneda S, Katakai A, Tamada M. Bacterial adhesion to and viability on positively charged polymer surfaces. Microbiology (Reading). 2006;152:3575-83.
36. Bollen CM, Lambrechts P, Quirynen M. Comparison of surfasse roughness of oral hard materials to the threshold surfasse roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997;13:258-69.
37. Quirynen M, Marechal M, Busscher HJ, Weerkamp AH, Darius PL, van Steenberghe D. The influence of surface free energy and surface roughness on early plaque formation. An in vivo study in man. J Clin Periodontol. 1990;17:138-44.
38. Bettencourt AF, Costa J, Ribeiro IAC, Gon�alves L, Arias-Moliz MT, Dias JR, Franco M, Alves NM, Portugal J, Neves CB. Development of a chlorhexidine delivery system based on dental reline acrylic resins. Int J Pharm. 2023;631:122470.
39. Ghosh M, Shetty S. Effect of addition of graphene and carbon nanotubes on flexural strength of polymethylmethacrylate- a comparative in-vitro study. J Evolution Med Dent Sci. 2020;9:1494-9.
40. Xie H, Cao T, Rodr�guez-Lozano FJ, Luong-Van EK, Rosa V. Graphene for the development of the next-generation of biocomposites for dental and medical applications. Dent Mater. 2017;33:765-74.
41. Novoselov K, Geim A, Morozov S, Jiang D, Zhang Y, Dubonos S, et al. Electric field effect in atomically thin carbon films. Science. 2004;306(5696):666-9.
42. Huang X, Yin Z, Wu S, Qi X, He Q, Zhang Q, et al. Graphene-Based Materials: Synthesis, Characterization, Properties, and Applications. Small. 2011;7:1876-902.
43. Yan L, Zheng YB, Zhao F, Li S, Gao X, Xu B, et al. Chemistry and physics of a single atomic layer: strategies and challenges for functionalization of graphene and graphenebased materials. Chem Soc Rev. 2012;41:97-114.
44. Bitounis D, Ali-Boucetta H, Hong B, Min D, Kostarelos K. Prospects and challenges of graphene in biomedical applications. Adv Mater. 2013;25:2258�68.
45. Costa J, Matos A, Bettencourt A, Portugal J, Neves CB. Effect of ethanol solutions as post-polymerization treatment on the properties of acrylic reline resins. Rev Port Estomatol Med Dent Cir Maxilofac. 2016;57:215-22.
46. International Organization for Standardization. ISO 20795-1:2013. Dentistry base polymers. Part 1: Denture base polymers. Geneva. Available at: https://www.iso.org/standard/62277.html.
47. International Organization for Standardization. ISO 178:2019. Plastics - Determination of flexural properties.
48. Annual Book of ASTM Standard, �Standard Test Method for Plastics Properties Durometer Hardness�, D (2240-03), 2003:1-12.
49. Moldovan M, Prodan D, Sarosi C, Carpa R, Socaci C, Rosu M, et al.. Synthesis, morpho-structural properties and antibacterial effect of silicate-based composites containing graphene oxide/hydroxyapatite. Mater Chem Phys. 2018;217:48�53.
50. Xie H, Cao T, Rodriguez-Lozano F, Luong-Van E, Rosa V. Graphene for the development of the next-generation of bios for dental and medical applications. Dent Mater. 2017;33:765-74.
51. Di Carlo S, De Angelis F, Brauner E, Pranno N, Tassi G, Senatore M, et al.. Flexural strength and elastic modulus evaluation of structures made by conventional PMMA and PMMA reinforced with graphene. Eur Rev Med Pharmacol Sci. 2020;24:5201-8.
52. Gosh M, Shetty S. Effect of addition of graphene and carbon nanotubes on flexural strength of polymethylmethacrylate � a comparative in vitro study. J Evol Med Dent Sci. 2020;9:1494-9.
53. Alamgir M, Nayak G, Mallick A, Tiwari S, Mondal S, Gupta M. Processing of PMMA nanocomposites containing biocompatible GO and TiO2 nanoparticles. Materials and Manufacturing Process. 2018;33:1291-8.
54. Lee JH, Jo JK, Kim DA, Patel KD, Kim HW, Lee HH. Nanographene oxide incorporated into PMMA resin to prevent microbial adhesion. Dent Mater. 2018;34:e63-e72.
55. Agarwalla SV, Malhotra R, Rosa V. Translucency, hardness and strength parameters of PMMA resin containing graphene-like material for CAD/CAM restorations. J Mech Behav Biomed Mater. 2019;100:103388.
56. Leite PIF. The Application of Graphene in Removable Prosthesis [Dissertation]. Faculdade de Medicina Dent�ria do Porto, 2015.
57. de Armentia SL, Fern�ndez-Villamar�n S, Ballesteros Y, Del Real JC, Dunne N, Paz E. 3D Printing of a Graphene-Modified Photopolymer Using Stereolithography for Biomedical Applications: A Study of the Polymerization Reaction. Int J Bioprint. 2022;8:503.
58. Kausar A. Poly(methyl methacrylate) nanocomposite reinforced with graphene, graphene oxide, and graphite: a review. Polym Plast Technol Mater. 2019;58:821-42.
59. Shen M, Chang T, Hsieh T, Li Y, Chiang C, Yang H, Yip M. Mechanical properties and tensile fatigue of graphene nanoplatelets reinforced polymer nanocomposites. J Nanomater. 2013;2013:565401.
60. Punset M, Brizuela A, P�rez-Pevida E, Herrero-Climent M, Manero JM, Gil J. Mechanical Characterization of Dental Prostheses Manufactured with PMMA-Graphene Composites. Materials (Basel). 2022;15:5391.
61. An Y, Liu B, Yan X, Pei J, Liu J. The Experimental Study on Wear Resistance of the Denture Base Material Reinforced with Graphene Oxide. Mocaxue Xuebao/Tribology 2013;33:222�8.
62. Rafiee M, Rafiee J, Wang Z, Song H, Yu Z, Koratkar N. Enhanced mechanical properties of nanocomposites at low graphene content. ACS Nano 2009;3:3884-90.
63. Sakaguchi R, Ferracane J, Powers J. Craig�s Restorative Dental Materials. 14th ed. St. Louis: Elsevier, 2019.
64. Lee HH, Lee CJ, Asaoka K. Correlation in the mechanical properties of acrylic denture base resins. Dent Mater J. 2012;31:157-64.
65. Moriche R, Artigas J, Reigosa L, S�nchez M, Prolongo SG, Ure�a A. Modifications Induced in Photocuring of Bis-GMA/ TEGDMA by the Addition of Graphene Nanoplatelets for 3D Printable Electrically Conductive Nanocomposites. Composites Science and Technology. 2019;184:107876.
66. Gungor H, Gundogdu M, Yesil Duymus Z. Investigation of the effect of different polishing techniques on the surfasse roughness of denture base and repair materials. J Prosthet Dent. 2014;112:1271�7.
67. Al-Kheraif A. The effect of mechanical and chemical polishing techniques on the surface roughness of heatpolymerized and visible light-polymerized acrylic denture base resins. Saudi Dent J. 2014;26:56�62.
�
Helena Salgado
E-mail address: hsalgado@ucp.pt<
�
Acknowledgements
The authors acknowledge the support of Graphenest Advanced Nanotechnology in supplying graphene nanoplatelets and producing PMMA-graphene resins. They are also grateful to the Laboratory of Tribology-FEUP, namely, Prof. Dr. Carlos Fernandes, for the support in measuring surface roughness.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects.The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent.The authors declare that no patient data appear in this article.
�
CRediT authorship contribution statement
Helena Salgado: Project administration; Conceptualization; Methodology; Formal analysis; Data curation; Writing � original draft.
Joana Fialho: Data curation; Formal analysis.
Marco Marques: Methodology; Resources; Software.
M�rio Vaz: Conceptualization; Methodology; Resources; Writing � review and editing; Validation.
Maria Helena Figueiral: Conceptualization; Data curation; Supervision; Writing � review & editing; Validation.
Pedro Mesquita: Supervision; Validation; Writing-review & editing.
�
1646-2890/� 2023 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
