
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2022 | 63 (3) | 134-140
Original research
Influence of abutment and connection type on implant-abutment connection rigidity: an in vitro study
Rigidez da ligação implante-pilar com diferentes tipos de conexões e pilares: estudo in vitro
a Unidade de Investigação em Ciências Orais e Biomédicas (UICOB), Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b Departamento de Engenharia Mecânica, Faculdade de Ciências e Tecnologias, Universidade de Coimbra, Coimbra, Portugal
c Laboratório de Instrumentação, Engenharia Biomédica e Física da Radiação (LIBPhys), Portugal
Teresa Almeida Mendes - teresa.gmendes@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 63
Issue - 3
Original research
Pages - 134-140
Go to Volume
Article History
Received on 27/01/2022
Accepted on 13/09/2022
Available Online on 04/10/2022
Keywords
Original Research
�
Influence of abutment and connection type on implant-abutment connection rigidity: an in vitro study
Rigidez da liga��o implante-pilar com diferentes tipos de conex�es e pilares: estudo in vitro<
�
Teresa Almeida Mendes1,*0000-0001-6232-0251
Lu�s Miguel Vilhena20000-0001-9592-3120
Jaime Portugal10000-0001-5058-6554
Jo�o Caram�s1,30000-0002-5544-3744
Am�lcar Lopes Ramalho20000-0001-7004-2212
Lu�s Pires Lopes1,30000-0001-8633-827X
1 Unidade de Investiga��o em Ci�ncias Orais e Biom�dicas (UICOB), Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal.
2 Departamento de Engenharia Mec�nica, Faculdade de Ci�ncias e Tecnologias, Universidade de Coimbra, Coimbra, Portugal.
3 Laborat�rio de Instrumenta��o, Engenharia Biom�dica e F�sica da Radia��o (LIBPhys), Portugal.
�
�
Article history:
Received 27 January 2022
Accepted 13 September 2022
Available online 30 September 2022
�
Abstract
Objectives: To evaluate the effects of the abutment material and the connection type on the implant-abutment connection rigidity.
Methods: The study evaluated eighteen implants with three different types of connections: external-hexagon, tri-channel, and conical connection. Half of the implants were connected to titanium abutments, and the other half to zirconia abutments, forming six study groups (n=3). The implants were submitted to 1,200,000 load cycles with a force amplitude of 90 N. During load application, the implant-abutment connection rigidity was determined in each cycle. The values obtained were analyzed with the two-way ANOVA test according to the abutment and connection types.
Results: Rigidity tended to increase during loading cycles. The abutment material did not influence rigidity (p=0.883). The external-hexagon connection presented lower rigidity than the internal connections, with statistically significant differences (p=0.013).
Conclusions: The abutment material does not influence the implant-abutment connection�s rigidity. The external-hexagon connection proved to be less rigid and stable than the internal connections.
Keywords: Dental implant-abutment design, Dental implants, Titanium, Yttria-stabilized tetragonal zirconia
�
Resumo
Objetivos: Avaliar o efeito do tipo de pilar e do tipo de conex�o na rigidez da liga��o implante-pilar, quando o conjunto � submetido a cargas c�clicas.
M�todos: Foram avaliados 18 implantes com tr�s tipos diferentes de conex�es: hex�gono externo, tri-channel e conex�o c�nica. Metade dos implantes foram conectados a pilares de tit�nio e a outra metade a pilares de zirc�nia, formando 6 grupos experimentais (n=3). Os implantes foram submetidos a 1.200.000 ciclos de carga com uma amplitude de for�as de 90 N. Durante a aplica��o das cargas, foi calculada a rigidez da liga��o implante-pilar para cada ciclo. Os valores obtidos foram analisados com o teste ANOVA de duas vias de acordo com o tipo de pilar e de conex�o.
Resultados: Verificou-se uma tend�ncia para o aumento da rigidez ao longo dos ciclos de carga. O tipo de pilar n�o influenciou a rigidez (p=0,883). Quanto �s conex�es, o hex�gono externo apresentou valores de rigidez inferiores aos verificados nas conex�es internas, sendo a diferen�a estatisticamente significativa (p=0,013).
Conclus�es: N�o se verificaram altera��es na rigidez implante-pilar de acordo com o tipo de pilar. O hex�gono externo demonstrou ser uma conex�o menos r�gida e est�vel comparativamente �s conex�es internas.
Palavras-chave: Pilar sobre implante, Implantes dent�rios, Tit�nio, Zirc�nia tetragonal estabilizada com �trio
�
Introduction
The materials most commonly used to manufacture dental implants and the abutments that connect the implant to the prosthetic crown are titanium and different titanium alloys.
These are biocompatible materials with good mechanical properties and a low risk of corrosion.1 On the other hand, zirconia abutments, first introduced in 1997, have aesthetic properties superior to titanium and high mechanical strength.2, 3 However, zirconia is much harder than titanium, and zirconia abutments directly screwed to the implant are suspected of wearing the implant platform, leading to loss of geometry and causing instability at the implant-abutment connection.4
Implant-abutment connections can be classified as external or internal depending on the presence or absence of a geometric index extending above the implant�s coronal surface.5 The external-hexagon connection consists of a 0.7-mm high hexagon extending above the implant�s coronal surface.6
This connection, introduced by Br�nemark, has the advantage of providing long-term follow-up data and compatibility among multiple implant systems.5 However, its hexagon�s low height implies a reduced contact area between the abutment and the implant platform, causing high stresses to the screw that connects the abutment to the implant. Thus, this connection is associated with an increased incidence of screw loosening.5, 6
On the other hand, in internal connections, the indexing mechanisms extend into the implant, increasing the abutment-implant contact area and reducing the stresses applied to the prosthetic screws.5 Internal connections have a lower incidence of screw loosening, better joint strength,5, 7 and improve the implant�s ability to withstand axial loads compared to external-hexagon connections.8 Several types of internal connections are currently available on the market, with varying geometries, and the main types are internal hexagon, tri-channel, crossfit, hexagonal conical, and cone morse.5
The implant-abutment connection�s stability has been identified as a major factor in the long-term success of dental implants.4 Micromovements between the abutment and the implant create an unstable connection that may lead to biological and prosthetic complications.4 Low amplitude oscillatory movements can cause implant fretting wear, which may widen the microgap between the abutment and implant, increasing bacterial infiltration and bone loss.9, 10 The increased implant abutment instability also creates rotational freedom that may lead to a higher incidence of screw loosening.8
However, few studies evaluate micromovements between the implant and the abutment with different connections, and the abutment material�s effect has not been adequately reported in the dental literature. Therefore, the present research study aimed to evaluate the effects of the abutment material and the connection type on the implant-abutment connection�s displacement amplitude and rigidity when subjected to cyclic loads. The following null hypotheses were tested: 1) the abutment material (titanium or zirconia) does not affect the implant-abutment connection�s rigidity; 2) the connection type (external-hexagon, tri-channel, or conical connection) does not affect the implant-abutment connection�s rigidity.
Material and methods
The sample size n=3 was calculated based on a pilot study. A power analysis indicated statistical significance (α=0.05) at 80% power.11, 12 The study evaluated eighteen implants with three different connection geometries: external hexagon (Br�nemark MK III TiUnite RP Nobel Biocare, G�teborg, Sweden), tri-channel (Replace Tapered RP Nobel Biocare, G�teborg, Sweden), and conical connection (Nobel Active RP Nobel Biocare, G�teborg, Sweden). The implants were inserted in the center of epoxy resin blocks (DPC-Laminierharz LT 2, Duroplast- Chemie Vertriebs GmbH, Neustadt/Wied, Germany) according to the manufacturer�s recommended surgical protocols.
Half of the implants were connected to zirconia abutments (Zirkon Translucence, Zirkonzahn GmbH, Gais, Italy) and the other half to grade-5 titanium abutments (Titan5 Zirkonzahn GmbH, Gais, Italy), forming six study groups.
The abutments were designed in the software Zirkonzhan (Zirkonzhan Modelier, Gais, Italy) and produced with CADCAM techniques (Zirkonzahn M5, Gais, Italy). They had a 5-mm wide, 8-mm height, and 30� inclination of the incisal edge.13
This 30� slope was designed to create an accurate contact with the hemispherical brace of the testing machine.13 The abutments were directly screwed to the respective implants using grade-5 titanium screws recommended by the manufacturer, specific for titanium or zirconia abutments (Abutment screw, Zirkonzhan, Gais, Italy). A torque of 35 Ncm was applied with a manual torque wrench (Nobel Biocare, G�teborg, Sweden).
The specimens were submitted to 1,200,000 load cycles,2, 13 with a sinusoidal load varying between 100 N and 10 N (load amplitude of 90 N),2 at a frequency of 10 Hz in a fatigue testing machine (Instron ElectroPlus E10000). During all the tests, the specimens were submerged in artificial saliva (SAGF).14 According to the ISO 14801:2007 standard,13 cyclic loads were applied with an angulation of 30� to the implant�s long axis (Figure 1).
�
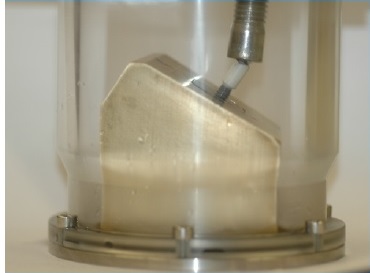
Figure 1. Testing machine with specimen support.
�
The fatigue tests were carried out with load control. During load application, the software that controls the mechanical fatigue testing machine graphically recorded, for each load cycle, the abutment-implant connection�s maximum and minimum displacement. The displacement amplitude was recorded as the difference between each cycle�s maximum and minimum displacement. The amplitude of the applied load was constant at 90 N.
For each load cycle, the rigidity was obtained using the following formula:15, 16 Rigidity =Force amplitude (N) Displacement amplitude (mm) In the analysis of rigidity evolution throughout the cycles, three different periods stand out during a given test (Figure 2). The first period corresponds to the first 100 cycles and is a phase of stabilization and accommodation of the abutment in contact with the load sphere; this period was discarded (Figure 2-A). The second period, between the 100th and 2000th cycles, corresponds to a stage of reduced rigidity variation (Figure 2-B). The third period, from the 2000th cycle to the end of each test, corresponds to a period of great rigidity variation. The second and third periods� average rigidity were calculated and designated as initial rigidity and final rigidity, respectively. The average total rigidity for each specimen was calculated based on the second and third periods� rigidity (Figures 2-B and 2-C).
�
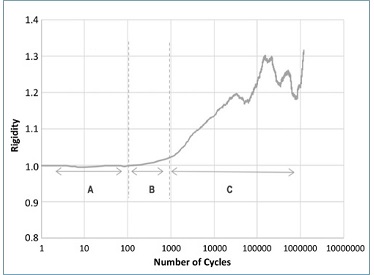
Figure 2. Exemplificative graph for the externalhexagon titanium specimen, showing rigidity evolution with the number of cycles during the mechanical test. Three different periods stand out: (A) Initial period of adaptation of the load control of the machine; (B) Period of reduced rigidity variation (Initial Rigidity); (C) Period of marked rigidity variation (Final Rigidity).
�
The dependent variable was the total rigidity (continuous variable, values expressed in N/mm), and the independente variables were the abutment material and connection type. Data were analyzed statistically using SPSS Statistics, version 28.0.1 (IBM SPSS Statistics, New York, United States).
After checking normality (Shapiro-Wilk tests; p>0.05) and the homogeneity of variances (Levene test; p>0.05), the 2-way ANOVA followed by Tukey�s post-hoc tests were used to detect the effect of main factors. A confidence level of α=0.05 was assumed.
Results
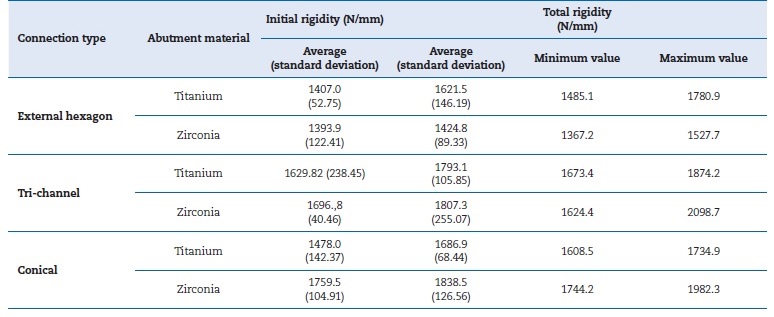
The average initial and total rigidity values of the various groups and the variation in rigidity (maximum and minimum) are shown in Table 1. In all groups, the average total rigidity was higher than the initial, representing an increase in rigidity throughout the test. The total rigidity values varied between a maximum of 2098.7 N/mm for the tri-channel connection with a zirconia abutment and a minimum of 1367.2 N/mm for the external-hexagon connection with a zirconia abutment.
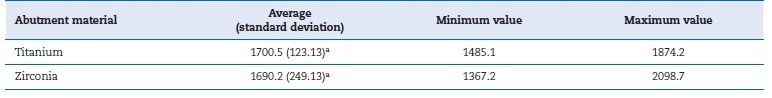
There were no statistically significant differences (p=0.883) in the abutment material�s effect on the rigidity of the implant- abutment connection (Table 2). Figure 3 represents the different abutment materials� mean total rigidity and respective standard deviation values.
�
Table 1. Mean and standard deviation of initial and total rigidity, n=3.
�
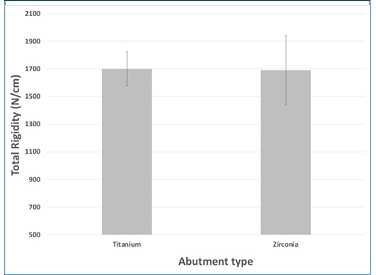
Figure 3. Influence of the abutment material on total rigidity (n=9; p=0.883).
�
Table 2. Measures of central tendency and dispersion of total rigidity, according to abutment material (N/mm), n=9. The average values have the same letter due to not showing statistically significant differences (p>0.05).
�
Conversely, the different groups showed statistically significant differences (p=0.013) in the connection type�s effect on the implant-abutment connection rigidity (Table 3). The two-way ANOVA test demonstrated no interaction between the two variables � type of connection and abutment material (p=0.156). The post-hoc tests revealed statistically significant differences between the total rigidity of the different connection types. Namely, there were differences between the external-hexagon and the tri-channel connections (p=0.016) and between the external-hexagon and the conical connections (p=0.036). There were no differences between the tri-channel and the conical connections (p=0.897). Figure 4 shows the values of the different connection types.
�
Table 3. Measures of central tendency and dispersion of total rigidity, according to connection type (N/mm), n=6. Connections with the same letter do not show statistically significant differences (p>0.05).

�
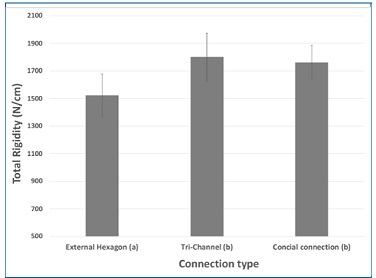
Figure 4. Influence of the connection type on the total rigidity (n=6). Connections with the same letter do not show statistically significant differences (p>0.05).
�
Discussion
In the present study, a mechanical testing machine measured the abutment displacement during cyclic loads to calculate the abutment-implant connection rigidity. The main conclusions of this work were that the abutment material did not influence the rigidity of the implant-abutment connection (the first null hypothesis cannot be rejected), but the connection type did (the second null hypothesis rejected).
The external-hexagon connection�s rigidity was lower than the tri-channel and conical internal connections, with statistically significant differences. These results can be related to the implant-abutment contact area, which differs according to the connection type. A connection with a larger contact area has more resistance to micromovements and higher joint stability and rigidity. Thus, a connection�s stress
concentration reduces as the internal area of the platform increases.17, 18 The contact area between implant and abutment is higher in internal connections than in the external- hexagon connection.19 In external connections, the axial loads occur directly over the screw.7 On the other hand, internal connections have higher stability, transfer forces more deeply, and tend to dissipate less stress on the screw than the external hexagon.7 The incidence of screw loosening is 5.4% with internal connections,20 while it varies between 6 to 48% with the external-hexagon connection.7
However, two clinical studies that evaluated clinical complications between implants with the external-hexagon and internal connections during 5 years in function did not detect statistically significant differences between the two types of connection.21, 22 Another clinical study evaluated two internal connections for 1 year after the placement of prosthetic rehabilitation and also found no differences between the two types of internal connections.23 Regarding the abutment material, contrary to the results obtained in the present study, zirconia abutments were reported to have superior rotational freedom than titanium abutments with external connection implants (Br�nemark, Nobel Biocare).24
The authors found no studies assessing the rigidity of different abutment-implant connections in the literature, but some studies measured the micromovements of the abutment-implant connection using various methodologies.
As in the present study, other authors argue that the type of connection conditions the micromovements between the abutments and the implants.25, 26 The tri-channel abutments seem to be the connection with the smallest magnitude of micromovements, which can be attributed to its geometry.
The tri-channel connection abutment25, 26 and Morse taper15 have lower displacements when compared to the external-hexagon connection. However, contrary to the presente study, some authors report that the conical connection (Nobel Active, Nobel Biocare) presented a higher displacement than the external-hexagon.25 This study results indicate a general tendency for an increase in rigidity with the progression of the test since the average total rigidity of all groups was higher after the application of cyclic loads, i.e., compared to the initial rigidity obtained in an initial phase of the tests.
During the cyclic loading, a zirconia abutment with a conical connection fractured. This specimen has since been replaced. The fracture occurred at the base of the abutment and may result from a smaller thickness of the zirconia in this area.27
Power analysis was made to calculate the sample size, and the ISO standard defines that data must be generated for a load cycle diagram, in which at least three specimens survive and none fail during the test.13 However, a larger sample would be convenient because small sample sizes and few specimens per group may influence the interactions between main factors.
Another limitation of the study is that only a few studies with heterogenous methodologies discussed this subject. Further studies with the same methodologies (number of cycles, frequency, artificial saliva) are needed. Moreover, ISO digital protocols should be created to standardize the comparing tools. A clinical trial with real oral conditions is also importante to deepen the knowledge of this phenomenon.
Conclusions
The present study showed no significant differences in the implant-abutment rigidity according to abutment material. However, the external-hexagon connection proved to be a less rigid and stable connection than the internal connections.
�
References
1. Hanawa T. Zirconia versus titanium in dentistry: A review. Dent Mater J. 2019;39:24-36.
2. Stimmelmayr M, Edelhoff D, G�th J, Erdelt K, Happe A, Beuer F. Wear at the titanium � titanium and the titanium � zirconia implant � abutment interface : A comparative in vitro study. Dent Mater. 2012;28:1215-20.
3. Naveau A, Rignon-Bret C, Wulfman C. Zirconia abutments in the anterior region: A systematic review of mechanical and esthetic outcomes. J Prosthet Dent. 2019;121:775-81.e1.
4. Nam RK, Lee SJ, Park EJ, Kwon HB, Yoon HI. Three-Dimensional Deformation and Wear of Internal Implant-Abutment Connection: A Comparative Biomechanical Study Using Titanium and Zirconia. Int J Oral Maxillofac Implants. 2018;33:1279-86.
5. Kofron MD, Carstens M, Fu C, Wen HB. In vitro assessment of connection strength and stability of internal implant abutment connections. Clin Biomech (Bristol, Avon). 2019;65:92-9.
6. Verdugo CL, N��ez GJ, Avila AA, San Mart�n CL. Microleakage of the prosthetic abutment/implant interface with internal and external connection: In vitro study. Clin Oral Implants Res. 2014;25:1070-83.
7. Pardal-Pel�ez B, Montero J. Preload loss of abutment screws after dynamic fatigue in single implant-supported restorations. A systematic review. J Clin Exp Dent. 2017;9:e1355-61.
8. B�douin Y, Lefran�ois E, Salomon JP, Auroy P. Abutment rotational freedom on five implant systems with diferente internal connections. J Prosthet Dent. 2021;S0022-3913(21)00266-3.
9. Yao KT, Kao HC, Cheng CK, Fang H-W, Huang CH, Hsu ML. Mechanical performance of conical implant-abutment connections under different cyclic loading conditions. J Mech Behav Biomed Mater. 2019;90:426-32.
10. Lauritano D, Moreo G, Lucchese A, Viganoni C, Limongelli L, Carinci F. The Impact of Implant�Abutment Connection on Clinical Outcomes and Microbial Colonization: A Narrative Review. Materials (Basel). 2020;13:1131.
11. Rosca B, Ramalho S, Sampaio-Fernandes JC, Portugal J. Reparability of two different CAD/CAM polymer materials using a light-cured composite and universal adhesives. Ver Port Estomatol Med Dent Cir Maxilofac. 2016;57:189-196.
12. Chasqueira AF, Arantes-Oliveira S, Portugal J. Bonding performance of simplified dental adhesives with three application protocols: an 18-month in vitro study. J Adhes Dent. 2020;22:255-64.
13. ISO 14801. International Standard for Dynamic fadigue test for endosseous dental implants. 2007.
14. Gal JY, Fovet Y, Adib-Yadzi M. About a synthetic saliva for in vitro studies. Talanta. 2001;53:1103-15.
15. Bicudo P, Reis J, Deus AM, Reis L, Vaz MF. Performance evaluation of dental implants: An experimental and numerical simulation study. Teoretical and Applied Fracture Mechanics. 2016;85:74-83.
16. Wang Y, Chen X, Zhang C, Feng W, Zhang P, Chen Y, et al. Studies on the performance of selective laser melting porous dental implant by finite element model simulation, fatigue testing and in vivo experiments. Proc Inst Mech Eng H. 2019;233:170-80.
17. Raoofi S, Khademi M, Amid R, Kadkhodazadeh M, Movahhedi MR. Comparison of the Effect of Three Abutment-implant Connections on Stress Distribution at the Internal Surface of Dental Implants: A Finite Element Analysis. J Dent Res Dent Clin Dent Prospects. 2013;7:132-9.
18. Takahashi JMFK, Dayrell AC, Consani RLX, N�bilo MAA, Henriques GEP, Mesquita MF. Stress Evaluation of Implantrev Abutment Connections Under Different Loading Conditions: A 3D Finite Element Study. J Oral Implantol. 2015;41:133-7.
19. Chun HJ, Shin HS, Han CH, Lee SH. Influence of implant abutment type on stress distribution in bone under various loading conditions using finite element analysis. Int J Oral Maxillofac Implants. 2006;21:195-202.
20. Lee KY, Shin KS, Jung JH, Cho HW, Kwon KH, Kim YL. Clinical study on screw loosening in dental implant prostheses: a 6-year retrospective study. J Korean Assoc Oral Maxillofac Surg. 2020;46:133-42.
21. Esposito M, Maghaireh H, Pistilli R, Grusovin MG, Lee ST, Trullenque-Eriksson A, et al. Dental implants with internal versus external connections: 5-year post-loading results from a pragmatic multicenter randomised controlled trial. Eur J Oral Implantol. 2016;1:129-41.
22. Vigolo P, Gracis S, Carboncini F, Mutinelli S, AIOP (Italian Academy of Prosthetic Dentistry) Clinical Research Group. Internal- vs External-Connection Single Implants: A Retrospective Study in an Italian Population Treated by Certified Prosthodontists. Int J Oral Maxillofac Implants. 2016;31:1385-96.
23. Cannata M, Grandi T, Samarani R, Svezia L, Grandi G. A comparison of two implants with conical vs internal hex connections: 1-year post-loading results from a multicentre, randomised controlled trial. Eur J Oral Implantol. 2017;10:161-8.
24. Alikhasi M, Monzavi A, Bassir SH, Naini RB, Khosronedjad N, Keshavarz S. A comparison of precision of fit, rotational freedom, and torque loss with copy-milled zirconia and prefabricated titanium abutments. Int J Oral Maxillofac Implants. 2013;28:996-1002.
25. Karl M, Taylor TD. Parameters Determining Micromotion at the Implant-Abutment Interface. Int J Oral Maxillofac Implants. 2014;29:1338-47.
26. Saidin S, Abdul Kadir MR, Sulaiman E, Abu Kasim NH. Effects of different implant-abutment connections on micromotion and stress distribution: Prediction of microgap formation. J Dent. 2012;40:467-74.
27. Ferrari A, Vichi A, Zarone F. Zirconia abutments and restorations: From laboratory to clinical investigations. Dent Mater. 2015;31:e63-76.
�
Teresa Almeida Mendes
E-mail address: teresa.gmendes@gmail.com
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
CRediT authorship contribution statement
TeresaAlmeida Mendes: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Visualization, Writing � original draft.
Lu�s Miguel Vilhena: Conceptualization, Data curation, Investigation, Methodology, Software, Supervision, Writing � review & editing.
Jaime Portugal: Formal analysis, Writing � review & editing.
Jo�o Caram�s: Conceptualization, Funding acquisition, Resources, Writing � review & editing.
Am�lcar Lopes Ramalho: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Writing- review & editing.
Lu�s Pires Lopes: Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Visualization, Writing � review & editing.
�
� 2022 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria.
Published by SPEMD. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0)
