
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2022 | 63 (3) | 159-166
Clinical case
Congenital granular cell tumor: an unusual case report
Tumor congénito de células granulares: um relato de caso incomum
a Post-graduate Program of Oral Pathology, Dentistry Department, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte, Brazil
Rani Iani Costa Gonçalo - ranigoncalo@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 63
Issue - 3
Clinical case
Pages - 159-166
Go to Volume
Article History
Received on 13/03/2022
Accepted on 10/08/2022
Available Online on 22/09/2022
Keywords
Clinical Case Report
�
Congenital granular cell tumor: an unusual case report
Tumor cong�nito de c�lulas granulares: um relato de caso incomum
�
Yailit Del Carmen Martinez Vargas1 0000-0001-5506-3111
Rani Iani Costa Gon�alo1 0000-0002-6762-135X
Danielle Machado Farias1 0000-0003-1829-0010
L�lia Maria Guedes Queiroz1 0000-0003-3380-0226
1 Post-graduate Program of Oral Pathology, Dentistry Department, Federal University of Rio Grande do Norte, Natal, Rio Grande do Norte, Brazil.
�
�
Article history:
Received 13 March 2022
Accepted 10 August 2022
Available online 22 September 2022
�
Abstract
Congenital granular cell tumor is an uncommon benign oral lesion of uncertain histogenesis that affects the alveolar ridge region of newborns. The present study aims to report an unusual congenital granular cell tumor case, emphasizing clinical, morphological, and immunohistochemical aspects. A 10-day-old newborn patient attended the stomatology service with a nodular pedunculated lesion of normal color located in the anterior region of the superior alveolar ridge. Thus, the diagnostic hypothesis was congenital epulis, and an excisional biopsy was performed. Histopathological analysis revealed
features consistent with the diagnosis of congenital granular cell tumor. In addition, we performed immunohistochemical staining for vimentin, Ki-67, and S100. The patient has been under follow-up with no clinical signs of recurrence. Due to its rarity, the analysis of congenital granular cell tumor�s clinicopathological characteristics enables an adequate diagnosis and treatment.
Keywords: Congenital epulis, Newborn, Oral pathology, Pediatrics
�
Resumo
O tumor cong�nito de c�lulas granulares � uma les�o oral benigna incomum de histog�nese incerta que afeta a regi�o de rebordo alveolar de rec�m-nascidos. O objetivo do presente estudo � relatar um caso incomum de tumor cong�nito de c�lulas granulares, com �nfase nos aspetos cl�nicos, morfol�gicos e imuno-histoqu�micos. Paciente rec�m-nascida, 10 dias de vida, compareceu ao servi�o de estomatologia apresentando les�o nodular, pedunculada e de colora��o semelhante � mucosa, em regi�o anterior do rebordo alveolar superior. Assim, a hip�tese diagn�stica foi de ep�lide cong�nita, sendo realizada bi�psia excisional. A an�lise histopatol�gica evidenciou caracter�sticas consistentes com o diagn�stico de tumor cong�nito de c�lulas granulares. Associado a isso, a colora��o imuno-histoqu�mica foi realizada para vimentina, Ki-67 e S100. A paciente est� em acompanhamento, sem sinais cl�nicos de recorr�ncia. Portanto, devido � raridade dessa les�o, a an�lise das suas caracter�sticas clinicopatol�gicas permite a obten��o de um diagn�stico e tratamento adequados.
Palavras-chave: Ep�lide cong�nita, Rec�m-nascido, �Patologia oral, Pediatria
�
Introduction
Congenital granular cell tumor (CGCT) is an uncommon benign lesion that affects fetuses and neonates. It shows a predilection for females, and the anterior alveolar mucosa of the maxilla is the most affected intraoral site.1, 2 As for its histogenesis, hypotheses include odontogenic, neural, histiocytic, pericytic, fibroblastic, muscular, and even undifferentiated mesenchymal cells. However, the CGCT�s histogenesis remains unknown, and there is no consensus in the literature.1, 3, 4 Clinically, CGCT presents as a single circumscribed growth with sessile or pedunculated implantation, color ranging from pink to reddish, and size ranging from a few millimeters to about 10 centimeters in diameter.2 Multiple lesions involving the maxilla and mandible have also been described in 10% of cases.4 5 - 7 Histopathological images reveal rounded voluminous cells with abundant eosinophilic granular cytoplasm and slightly basophilic oval nuclei. CGCT�s microscopic appearance is very similar to granular cell tumors, and the differential diagnosis between the two is based on etiological, clinical, and immunohistochemical aspects.1, 3, 6, 8
Surgical excision is recommended immediately upon detection of the lesion, and spontaneous regression is rare. Large lesions can cause feeding difficulties and airway obstruction in the neonate.5, 6, 9 This study reports a case of CGCT and discusses clinical and histopathological characteristics, as well as differential diagnoses from other lesions, while emphasizing a multidisciplinary approach.
Case report
A 10-day-old Black female newborn was presented at a Stomatology Service with a nodular lesion in the oral cavity. Intraoral physical examination revealed a pedunculated exophytic nodular lesion of firm consistency and coloring similar to the mucosa, located in the anterior region of the left upper alveolar ridge and measuring approximately 3.0 x 2.0 cm in diameter (Figure 1). This mass was causing breastfeeding problems but no airway obstruction. The infant�s mother did not mention any adverse perinatal event, and the lesion was detected only at birth.
Considering a diagnostic hypothesis of congenital epulis, pediatric and anesthetic evaluations were performed to plan the surgical excision of the lesion, which occurred under general anesthesia with orotracheal intubation, as usually recommended in such cases.1, 3, 10 The lesion was completely excised using electrocautery, bleeding was minimal, and the infant recovered with no complications, achieving normal breastfeeding.
Histopathological examination revealed a benign, well-circumscribed lesion characterized by a proliferation of polygonal cells amid a sparse stroma (Figure 2). The cells exhibited rounded morphology and abundant eosinophilic granular cytoplasm.
Some of the rounded-to-oval-shaped basophilic nuclei appeared as expelled toward the cell�s periphery. The dense fibrous connective tissue stroma was sparse, with a mild infiltrate of mononuclear inflammatory cells and blood vessels. The epithelium lining exhibited atrophy of its epithelial ridges at its greatest extent, with an area of focal ulceration (Figures 3, 4, and 5). In order to better characterize the lesion under study, immunohistochemical staining for vimentin (Figure 6), Ki-67 (Figure ), and S100 (Figure 8) was performed.
The clinical, histopathological, and immunohistochemical aspects led to a diagnosis of CGCT. The patient has been under follow-up for 3 years, with no clinical signs of recurrence. The child�s parents signed a free informed consent form explaining and authorizing data usage for academic reasons. The institution�s Research Ethics Committee approved this study.
�

Figure 1. Clinical aspect. Pedunculated nodular lesion on the anterior upper alveolar ridge of a newborn.
�
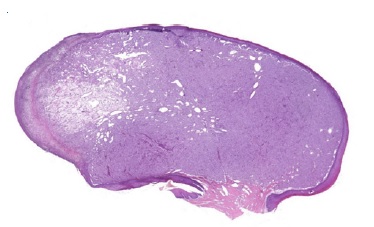
Figure 2. Histopathological features of CGCT. Well-circumscribed lesion characterized by the proliferation of polygonal cells amid a sparse stroma (H&E; 40x magnification).
�
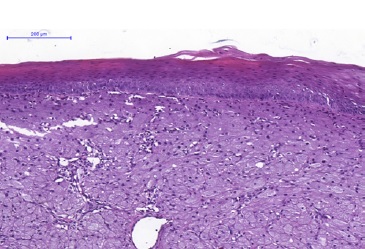
Figure 3. Histopathological features of CGCT. The lesion is lined by a parakeratinized stratified squamous epithelium exhibiting atrophy. There are lesion cells in the lamina propria (H&E; 100x magnification).
�
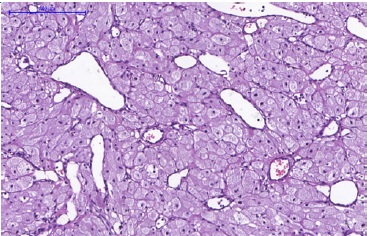
Figure 4. Histopathological features of CGCT. Blood vessels of varied shapes and sizes amid the granular cells (H&E; 400x magnification).
�
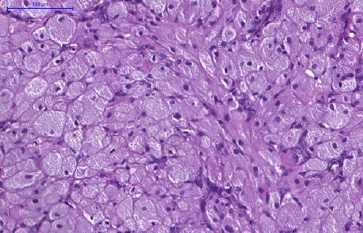
Figure 5. Histopathological features of CGCT.
In detail, the cells show a rounded morphology and an abundant and eosinophilic cytoplasm with granules. The basophilic nuclei, with a rounded-to-oval shape, are positioned at the cell periphery (H&E; 400x magnification).
�
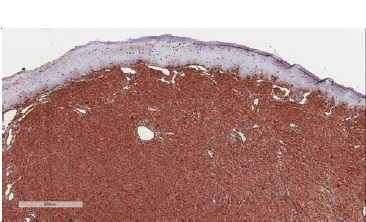
Figure 6. Immunohistochemical features of CGCT. Diffuse immunoexpression for vimentin (400x magnification).
�
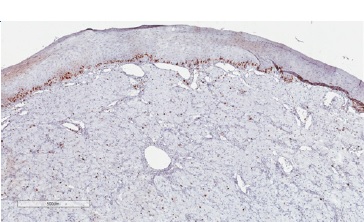
Figure 7. Immunohistochemical features of CGCT. Low proliferative index through analysis of Ki-67 immunoexpression (400x magnification).
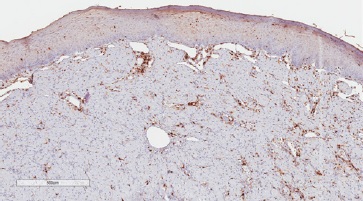
Figure 8. Immunohistochemical features of CGCT Granular cells exhibit immune-negativity for S100 (400x magnification).
�
Discussion and conclusions
CGCT was originally described by Neumann, who called it �congenital epulide.�11 Since then, few cases have been reported in the literature. In the last 5 years, only 22 studies2, 7, 10, 12 - 30 reporting CGCT occurrence were published (Table 1). The Greek-derived term �epulid� means �swollen gums� and is nonspecifically used in dentistry for hyperplastic lesions in the gingival tissue. The use of more specific terminology to name CGCT has been suggested, including �congenital granular cell lesion,� �newborn gingival granular cell tumor,� �newborn congenital epulis,� �congenital granular cell myoblastoma,� and �granular cell fibroblastoma.� However, due to the occurrence of extra-gingival cases, the term �congenital granular cell tumor� is likely most appropriate.9, 31
�
Table 1. Summary of clinical cases reported in the literature in the last 5 years.
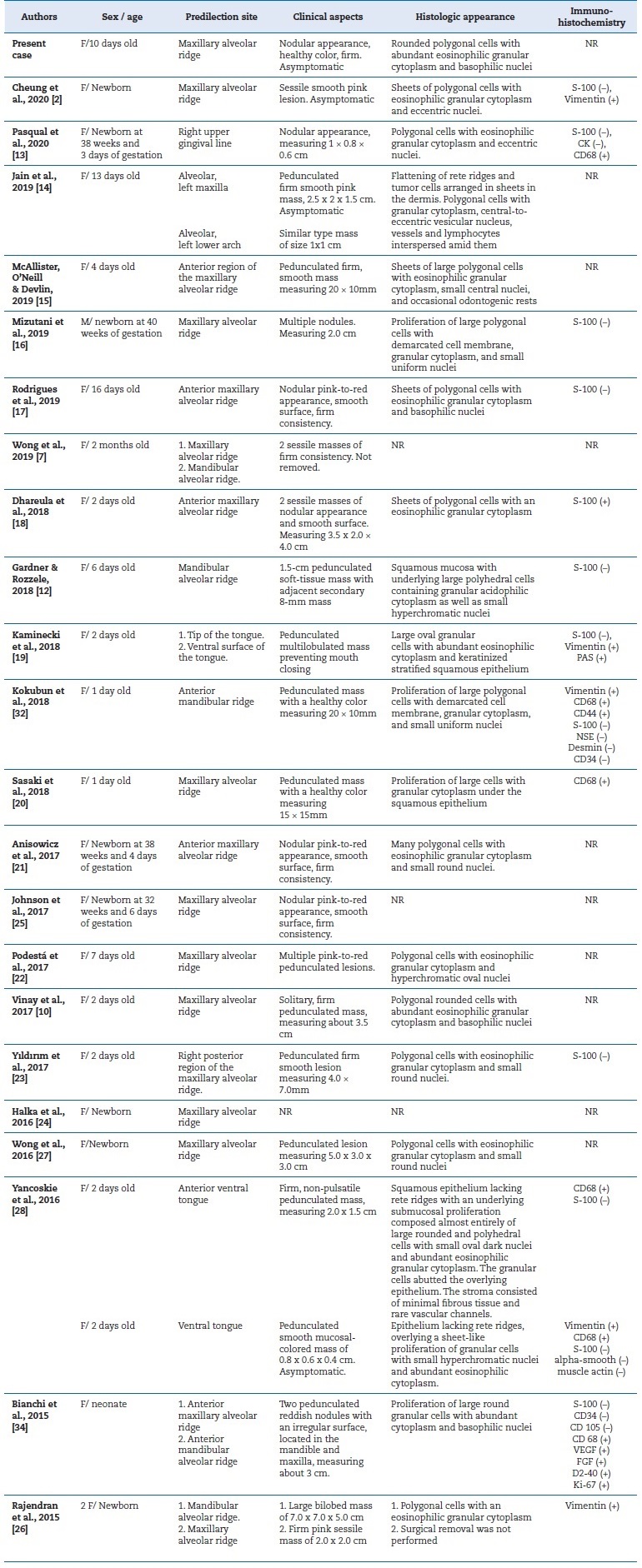
F � female; M � male; SMA � smooth-muscle actin; CK � cytokeratin; NSE � neuron-specific enolase; NR � not reported
�
CGCT is most frequently located in the anterior maxillary alveolar ridge and has demonstrated a marked predilection for female neonates compared to males at a ratio of 8:1. Clinically, CGCT presents as solitary lesions that are rarely multiple, are similar in color to the mucosa (or reddish), of firm consistency, with a smooth and non-ulcerated surface, and with sessile or pedunculated implantation. Typically, the CGCT is 1 to 2 cm in diameter, despite some reports of lesions larger than 9 cm.1 - 3, 5, 31 The present case report has clinical characteristics consistent with the findings shown in the literature.
Although its histogenesis is not well established, some authors believe that CGCT is a reactive entity.1, 3 Others believe that this lesion�s cellular phenotype is related to pericytic or myopericytic cells due to the marked vascularization typically observed in its stroma, with increased pericytic proliferation around small venules.5 Furthermore, due to its intrauterine origin and female predominance, the development of CGCT has been suggested as closely associated with maternal hormones.1, 3, 31 Despite a possible endogenous hormone influence, this hypothesis becomes untenable when considering the absence of estrogen or progesterone receptors in the lesion cells. Thus, the reason for the female gender preference is still uncertain.5, 8, 32
Due to CGCT�s rarity, healthcare professionals sometimes cannot clinically recognize it, leading to misdiagnoses. It is thus extremely important to perform an adequate anamnesis that, together with microscopic aspects, can facilitate diagnosis.
Upon histopathological examination, CGCT is very similar to granular cell tumors: both lesions exhibit tumor growth composed of polygonal eosinophilic cells containing cytoplasmic granules.3, 33 However, while CGCT demonstrates atrophy of the epithelium lining, the granular cell tumor has a characteristic pseudoepitheliomatous hyperplasia in its epithelial lining. Although both lesions have a predilection for females, their location differs: CGCT exclusively affects the alveolar ridge of newborns, while granular cell tumors can affect many sites in the body, despite being more common in the tongue, and are most common between the third and sixth decades of life.1, 3
In differential diagnosis, other lesions that present granular cells should be considered, such as granular cell melanoma, certain fibro-histiocytic neoplasms, smooth muscle tumors, and soft-tissue alveolar sarcoma. Immunohistochemical techniques can be used as a complementary tool to characterize the lesion better and discard other histologically similar lesions. Previous studies have evaluated the immunoexpression of proteins such as S100, smooth muscle actin (SMA), desmin, calponin, neuro-specific enolase (NSE), CD68, vimentin, cytokeratins (CKs), CD34, CD31, and Ki-67.5 In the present study, we observed lesion cells� immunopositivity for vimentin, negativity for S100, and a low cell proliferation index in Ki-67 analysis. These findings reinforced CGCT�s non-neoplastic nature and suggested a mesenchymal origin.
CGCT immunohistochemical profile analysis increases diagnostic accuracy and enables clinical management and treatment.
In contrast to granular cell tumors, which present granular cells immunoreactive for vimentin and S100, CGCT�s lesion cells present strong and diffuse immunostaining for vimentin, negativity for S100, and weak, focal immunostaining for Ki-67.1 - 3, 29 Immunoreactivity for S100 and NSE in the granular cell tumor suggests a Schwann-cell origin. On the other hand, CGCT is usually negative for S100 and positive for vimentin, suggesting a mesenchymal origin. However, CGCT positivity for NSE has been reported, indicating a possible neural origin.1, 2
Although uncommon, spontaneous remission is possible because CGCT�s growth tends to cease after birth, as in cases of small lesions that do not interfere with breathing or feeding.34 Yet, most studies recommend surgical excision of the lesion under local or general anesthesia.1, 3, 10 There are no reports of recurrence after surgical CGCT excision, even when there are tissue remnants of the lesion.1, 3 In addition to surgical excision, techniques using electrocautery and carbon dioxide laser, or even gingivoperiosteoplasty, can be used for subsequent primary alveolar reconstruction, promoting proper alignment and normal dental development.30
The present study reviews CGCT�s histopathological and immunohistochemical characteristics, comparing them with data reported in the literature and emphasizing the differential diagnosis from other oral lesions. Due to CGCT�s rarity, studies that analyze its clinicopathological and immunohistochemical characteristics can provide greater knowledge, enabling better diagnosis and clinical management.
�
References
1. Zhang B, Tan X, Zhang K, Ly Y, Chen J, Zhang F. A study of cell proliferation using immunohistological staining: a case report of congenital granular cell epulis. Int J Pediatr Otorhinolaryngol. 2016;88:58-62.
2. Cheung JM, Putra J. Congenital granular cell epulis: classic presentation and its differential diagnosis. Head Neck Pathol. 2020;14:208�11.
3. Liang Y, Yang YS, Zhang Y. Multiple congenital granular cell epulis in a female newborn: a case report. J Med Case Rep. 2014;8:413.
4. Sahu S, Maurya R, Rao Y, Agarwal A. Multiple congenital epulis in newborn � a rare presentation. J Oral Maxillofac Pathol. 2009;13:78-80.
5. Childers ELB, Fanburg-Smith JC. Congenital epulis of the newborn: 10 new cases of a rare oral tumor. Ann Diagn Pathol. 2011;15:157-61.
6. Kumar RM, Bavle R, Umashankar D, Sharma R. Congenital epulis of the newborn. J Oral Maxillofac Pathol. 2015;19:407.
7. Wong BJW, Cheung WS, Campbell KM. Congenital epulidesspontaneous regression. J Pediatr. 2019;205:287-287.e1.8. Vered M, Dobriyan A, Buchner A. Congenital granular cell epulis presents an immunohistochemical profile that distinguishes it from the granular cell tumor of the adult. Virchows Arch. 2009;454:303-10.
9. Silva GCC, Vieira TC, Vieira JC, et al. Congenital granular cell tumor (congenital epulis): a lesion of multidisciplinar interest. Med Oral Patol Oral Cir Bucal. 2007;12:428-30. PMID: 17909507.
10. Vinay KN, Anjulo, LA, Nitin P, Neha KV, Dhara D. Neumann�s Tumor: A Case Report. Ethiop J Health Sci. 2017;27:189- 92.
11. Neumann E. Ein fall von kongenitaler epulis. Arch Heilkd. 1871;12:189-90.
12. Gardner P, Rozzelle A. Congenital Granular Cell Tumor: Case Report and Review. Case Rep Pediatr. 2018;1:1-3.
13. Pasqual HM, Maldaner A, Macagnan MC, Link RA, Correa NB, Borges RS, et al. Granular cell in female neonate: a case report. J Bras Pato Med Lab. 2020;56:1-3.
14. Jain N, Sinha P, Singh L. Large Congenital Epulis in a Newborn: Diagnosis and Management. Ear Nose Throat J. 2020;99:NP79-81.
15. McAllister P, O�Neill T, Devlin M. Congenital Epulis: A Rare Case of Feeding Obstruction in a neonate. Br J Oral Maxillofac Surg. 2019;57:484:6.
16. Mizutani K, Mukai M, Nagatsuka H, Yamada S. Whitish-Yellow Tumor on its Characteristic Cut Surface: A Case Report of Congenital Granular Cell Epulis. Clin Pathol. 2019;12:2632010X19831257.
17. Rodrigues KS, Barros CCS, Rocha OKMS, Silva LAB, Paies MB, Miguel MCC. Congenital granular cells epulis: cade report and differential diagnosis. J Bras Pato Med Lab. 2019;55:281-8.
18. Dhareula A, Jaiswal M, Goyal A, Gauba K. Congenital granular cell tumor of the newborn - Spontaneous regression or early surgical intervention. J Indian Soc Pedod Prev Dent. 2018;36:319-23.
19. Kaminecki I, Xu W, Abbas SH, Kale M. Newborn with a rare congenital granular cell lesion of the tongue. BMJ Case Rep. 2018;11:226777.
20. Sasaki R, Okamoto T, Watanabe Y. Congenital Granular Cell Epulis. Plast Reconstr Surg Glob Open. 2018;6:1989.
21. Anisowicz, SK, Tolisano AM, Golden JB.Visual diagnosis: newborn with a large oral mass. Pediatr Ver. 2017;38:10-2.
22. El�as Podest� EM., Astucuri, CJ, Guti�rrez GM, �pulis del reci�n nacido. Rev Pediatr Aten Primaria. 2017;19:275-8.
23. Yıldırım C, Zerener T, Şen�imen M, Akgun OM, Altug H�, �i�ek AF. Congenital gingival granular cell tumor: A Case Report. J Dent (Shiraz). 2017;18:70-2.
24. Halka J, Chaiyasate K. Congenital Epulis. Eplasty. 2016;16:ic8.
25. Johnson K, Shainker S, Estroff J, Ralston SJ. Prenatal diagnosis of congenital epulis: implications for delivery. J Ultrasound Med. 2017;36:449-51.
26. Rajendran G, Pay A, Roehr CC. Two variations of congenital epulis. Arch Dis Child Fetal Neonatal Ed. 2016;101:F432.
27. Wong DKC, Ramli R, Muhaizan WM, Primuharsa Putra SHA. Congenital epulis: A rare benign tumour. Med J Malaysia. 2016;71:300-1.
28. Yancoskie AE. Congenital granular cell lesion of the tongue: a report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:14-8.
29. Kokubun K, Matsuzaka K, Akashi Y, Sumi M, Nakajima K, Murakami S, Narita M, Shibahara T, Inoue T. Congenital Epulis: A Case and Review of the Literature. Bull Tokyo Dent Coll. 2018;59:127-32.
30. Bianchi PR, Araujo VC, Ribeiro JWB, Passador-Santos F, Araujo NS,Soares AB. Multiple congenital granular cell epulis: case report and immunohistochemical profile with emphasis on vascularization. Case Rep Dent. 2015;2015:878192.
31. Conrad, Rachel; Perez, Mia CN. Congenital granular cell epulis. Arch Pathol Lab Med. 2014;138:128-31.
32. Leocata P, Bifaretti G, Saltarelli S, Corbacelli A, Ventura L. Congenital (granular cell) epulis of the newborn: A case report with immunohistochemical study on the histogenesis. Ann Saudi Med. 1999;19:527‐9.
33. van der Waal I. Congenital granular cell epulis. In: Barnes L, Eveson JW, Reichart P, Sidransky D editors. World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press, 2005. p.198.
34. Tiwari C, Nagdev M, Saoji R, Nama N, Joshi S. Large congenital epulis: a neonatal tumour with striking appearance, but simple management. Fetal Pediatr Pathol. 2022; 41:351-3.
�
Rani Iani Costa Gon�alo
Correio eletr�nico: ranigoncalo@gmail.com
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Acknowledgments
This study was financed in part by the Coordena��o de Aperfei�oamento de Pessoal de N�vel Superior - Brasil (CAPES) � Finance Code 001.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
CRediT authorship contribution statement
Yailit Del Carmen Martinez Vargas: Conceptualization, Data curation, Project administration, Visualization, Writing � original draft, Writing � review & editing;
Rani Iani Costa Gon�alo: Conceptualization, Data curation, Methodology, Visualization, Writing � original draft, Writing � review & editing;
Danielle Machado Farias: Data curation, Validation, Visualization, Writing � review& editing; L�lia
Maria Guedes Queiroz: Formal analysis, Investigation, Project administration, Supervision, Visualization, Writing � review & editing.
�
1646-2890/� 2022 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0).
