
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (4) | 229-236
Original research
Oral health-related knowledge and practices among a cohort of pregnant Portuguese women
Conhecimentos e práticas relacionadas à saúde bucal em uma coorte de gestantes portuguesas
a University of Coimbra, Faculty of Medicine, Dentistry Department, Institute of Paediatric Dentistry and Preventive Dentistry (Coimbra, Portugal)
b University of Coimbra, Faculty of Medicine, Center for Innovation and Research in Oral Sciences (Coimbra, Portugal)
Margarida Esteves - margarida.esteves022@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 4
Original research
Pages - 229-236
Go to Volume
Article History
Received on 20/11/2020
Accepted on 18/11/2021
Available Online on 24/12/2021
Keywords
Original Research
�
Oral health-related knowledge and practices among a cohort of pregnant Portuguese women
Conhecimentos e pr�ticas relacionadas � sa�de bucal em uma coorte de gestantes portuguesas
�
Margarida Esteves1,* 0000-0001-8522-983X
Joana Leonor Pereira1 0000-0002-4669-8999
Carolina Gomes1
B�rbara Cunha1 0000-0001-9660-1393
Ana Messias1,2 0000-0003-4019-9379
Ana L. Costa1,2 0000-0002-4102-1719
1 Dentistry Department, Institute of Paediatric Dentistry and Preventive Dentistry, Faculty of Medicine, University of Coimbra, Coimbra, Portugal
2 Center for Innovation and Research in Oral Sciences, Faculty of Medicine, University of Coimbra, Coimbra, Portugal.
�
�
Article history:
Received 20 October 2020
Accepted 18 November 2021
Available online 23 December 2021
�
Abstract
Objectives: To assess the level of knowledge and attitudes regarding prenatal and infant oral health in a sample of pregnant women from Coimbra, Portugal.
Methods: A self-applied questionnaire was administered to randomly selected pregnant women who attended prenatal check-ups at two public health institutions in Coimbra. Collected data included sociodemographic information, oral health knowledge and practices in pregnancy, and knowledge on oral health in children. All ethical requirements were met. Statistical analysis was conducted using descriptive and inferential methods. Variables were tested for independence using a chi-square test with a 95% confidence interval.
Results: A total of 120 women enrolled in the study. Although 68.9% of participants brushed their teeth twice daily, 36.4% reported not using floss, with a statistically significant association with age (p=0.004). Half of the respondents had not attended a dental appointment before pregnancy, and 59.2% believed pregnancy could be harmful to oral health. Findings showed limited knowledge of the possible consequences of gingivitis and periodontitis to the course of pregnancy and the importance of diet in oral health. Moreover, a low level of understanding was noted regarding the existence and prevention of early childhood caries.
Conclusions: Oral health-related knowledge and practices of surveyed women were in general deficient. Considering pregnancy is a period of particular interest for acquiring knowledge and good oral health practices, which are decisive for both the expectant mother na� the child, our results highlight an urgent need to implement prenatal oral health care programs in this study population.
Keywords: Dental caries, Health knowledge, Attitudes, Practice infant oral health, Pediatric dentistry, Periodontitis, Pregnancy, Prenatal care, Preventive dentistry.
�
Resumo
Objetivos: Avaliar os conhecimentos e atitudes relativos � sa�de oral na gravidez e na inf�ncia de uma amostra de gr�vidas de Coimbra, Portugal.
M�todos: Um question�rio auto-aplic�vel foi administrado a uma amostra aleat�ria de gr�vidas em seguimento pr�-natal em duas institui��es de sa�de p�blicas de Coimbra. Colheram-se dados sociodemogr�ficos e referentes aos conhecimentos e pr�ticas de sa�de oral na gravidez e relativos ao beb�. Todos os requisitos �ticos foram cumpridos. Procedeu-se a an�lise estat�stica descritiva e inferencial dos resultados. Verificou-se a independ�ncia das vari�veis atrav�s do teste de qui-quadrado para um intervalo de confian�a de 95%.
Resultados: A amostra incluiu 120 gr�vidas. Apesar de 68.9% das participantes ter revelado realizar escovagem bi-di�ria, 36.4% n�o usava fio dent�rio, verificando-se uma associa��o estatisticamente significativa deste h�bito com a idade (p=0.004). Metade das inquiridas n�o visitou o m�dico dentista antes da gravidez e 59.2% considerava que a gravidez era potencialmente danosa para a sa�de oral. Foram evidenciadas algumas lacunas no conhecimento relativamente �s poss�veis consequ�ncias de gengivite ou periodontite no desfecho da gravidez e acerca da import�ncia da dieta para a sa�de oral. Destacou-se tamb�m falta de informa��o no que respeita � c�rie precoce de inf�ncia e � sua preven��o.
Conclus�es: Em geral, as gr�vidas apresentaram conhecimentos e comportamentos de sa�de oral insuficientes. Atendendo a que a gravidez constitui uma fase de particular interesse para a aquisi��o de conhecimentos e modifica��es comportamentais decisivos para a gestante e beb�, os presentes resultados suportam a necessidade de implementar programas de sa�de oral pr�-natal nesta popula��o.
Palavras-chave: C�rie dent�ria, Conhecimentos, �Atitudes e pr�ticas de sa�de oral, Beb�, Sa�de oral, Odontopediatria, Periodontite, Gravidez, Cuidados pr�-natais, Medicina dent�ria preventiva.
�
Introduction
During pregnancy, a woman experiences oral and systemic changes, including behavioral, organic, and physiological alterations at various levels (e.g., endocrine, cardiovascular, respiratory, immunological, and neurological).1 - 3 Some of these changes can lead to a greater susceptibility to specific oral pathologies, both in terms of soft and hard tissues.1, 4 - 6 However, inadequate attention to oral health during pregnancy is commonly reported.
Poor attention to oral health often leaves pregnant women susceptible to oral problems, such as pain, and increased levels of anxiety largely related to adverse pregnancy outcomes. 2, 7 - 9
Moreover, cumulative evidence has associated periodontal diseases in pregnant women with adverse pregnancy outcomes, including preeclampsia, gestational diabetes, preterm birth, and low birth weight.10, 13 Research has further shown that the mother�s oral condition and behaviors significantly influence the offspring�s oral health outcomes, particularly the risk of experiencing early childhood caries (ECC).10 15 - 16
Considering the inherent oral implications of pregnancy and the potential systemic consequences, timely monitoring and early intervention are extremely important. Therefore, monitoring oral health in pregnant women should be an integral part of the approach to their general healthcare.4, 5, 7, 17 - 19
During the prenatal period, pregnant women show greater interest and receptivity in acquiring information and changing their health habits and practices.4, 5 Oral health education covering the prevention of oral diseases and demonstrating correct practices can then be provided. In addition, periodic consultations should be encouraged, as they bring importante benefits for both pregnant women and their children.4, 16, 18, 20, 21
Previous studies have found evidence of knowledge gaps and misconceptions among expectant mothers concerning: oral hygiene habits, the incidence of various oral pathologies, dental treatment, and poor oral health and its impact on the course of pregnancy and ECC.17, 18, 21 - 27 Multiple barriers to accessing oral healthcare during pregnancy have also been identified in several countries.8, 9 To our knowledge, available data among pregnant women in Portugal is limited, as the few published
studies involved small sample sizes and did not fully record the participants� knowledge of the impact of maternal oral health and behavior on children�s oral health. 28, 29 Accordingly, the present study aims to assess the effect of maternal knowledge and practices on prenatal and infant oral health, with a survey of pregnant women followed in two Portuguese public health institutions.
Material and methods
This cross-sectional survey was performed using a convenience sample of pregnant women attending pre-scheduled consultations for routine prenatal follow-up at a public maternity practice and a family health facility in Coimbra, Central Portugal. A total of 120 pregnant women were eligible to enroll in the study: 82 from the public maternity system, 19 from the family health facility, and 19 from individual contacts of the researchers. All women agreed to participate in this study. Data collection occurred over two consecutive months on randomly selected days.
The research fully complied with the ethical requirements of the 1964 Helsinki declaration and its later amendments. Required authorizations were obtained from both institutions prior to commencing the study. After giving written informed consent, each participant was asked to complete a self-reported questionnaire. Exclusion criteria included non-Portuguese speakers and unwillingness to participate.
The questionnaire, based on previously published surveys,22, 23, 25 consisted of 29 closed-answer questions covering sociodemographic information, oral health knowledge and practices in pregnancy, and the pregnant woman�s knowledge of oral health in children.
The results of the questionnaires were entered into Microsoft Excel� 2011 for subsequent statistical treatment using IBM SPSS Statistics21. A descriptive analysis was performed, and the independence of the variables was checked with the chisquare test (χ2) under a 95% confidence interval (p<0.05).
Results
The sociodemographic profile of the sample is shown in Table 1. Approximately half of the respondents (52.5%) were aged between 31 and 35 years old, 71.7% had attended higher education, 64.0% were married, and 71.7% lived in urban areas (Table 1). This was the first pregnancy of most women, and 52.5% were in the last trimester of pregnancy (Table 1).
�
Table 1. Sociodemographic characterization of the sample.
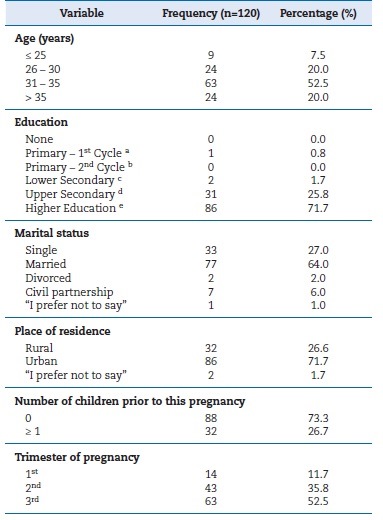
a Primary - 1st Cycle (up to 4 years of schooling)
b Primary - 2nd Cycle (up to 6 years of schooling)
c Lower Secondary (up to 9 years of schooling)
d Upper Secondary (up to 12 years of schooling)
e Higher Education (university level)
�
Concerning attitudes and behaviors of pregnant women regarding their oral health, 68.9% reported brushing twice a day, and 36.4% said they did not use dental floss as an additional measure (Table 2). As a group, pregnant women below 25 years stood out due to their low use of dental floss, with a statistically significant association (p=0.004; χ2=14.329) between using dental floss and age (Table 2).
�
Table 2. Attitudes and practices of the pregnant woman regarding oral health.
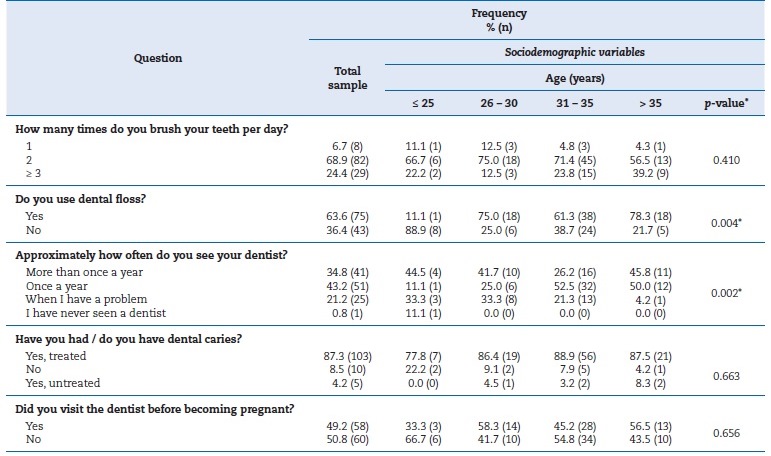
* Chi‑square test (χ2) under a 95% confidence interval (p<0.05)
�
When asked about the frequency of dental appointments and prior history of dental caries, 43.2% of respondents confirmed they regularly attended annual consultations, and most (87.3%) said they had previously had caries lesions treated (Table 2). About 60.8% of the respondents rated their current oral health status as �Good�, while 31.7% rated it as �Acceptable� and 7.5% as �Excellent�. However, only 49.2% of the pregnant women had undergone dental appointments before their current pregnancy (Table 2).
Regarding the oral health-related knowledge of pregnant women, most participants (83.3%) responded positively when asked about the possibility/need to undergo dental treatment during pregnancy (Table 3). Nonetheless, over half of the respondentes (59.2%) agreed that pregnancy could be harmful to their oral health, with a statistically significant association to their age groups (p=0.010; χ2=17.165) and level of education (p=0.037; χ2=15.965) (Table 3). When asked, �Do you think that caries is a communicable disease?�, 69.2% of women gave a negative response and 20.8% did not have an opinion (Table 3). Similarly, 58.3% stated they were unaware that gingivitis or periodontitis could contribute to premature birth and low birth weight (Table 3).
�
Table 3. Knowledge of the pregnant woman regarding oral health.<
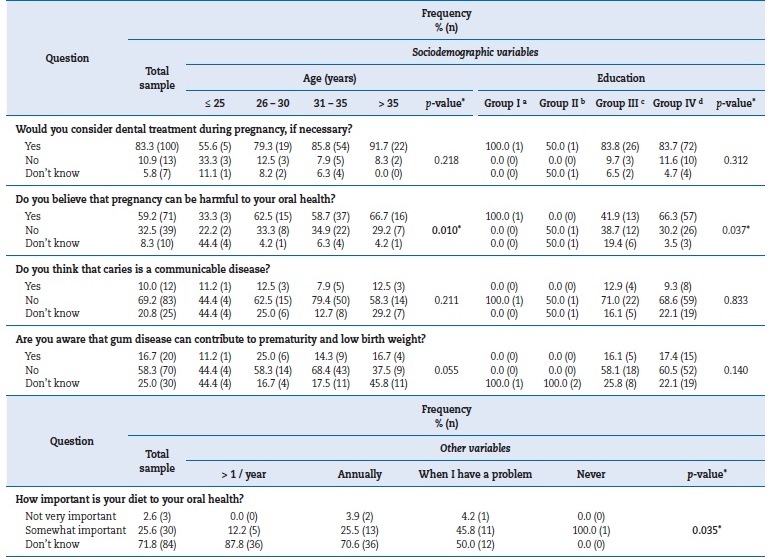
* Chi‑square test (χ2) under a 95% confidence interval (p<0.05)
a Group I: Primary - 1st Cycle (up to 4 years of schooling)
b Group II: Lower Secondary (up to 9 years of schooling)
c Group III: Upper Secondary (up to 12 years of schooling)
d Group IV: Higher Education (university level)
Most pregnant women showed a lack of knowledge of the importance of diet in oral health, with 71.8% stating they did not know the importance of diet to their oral health. A statistically significant association was found between the response to this question and the frequency of regular dental appointments (p=0.035; χ2=14.328) (Table 3).
Regarding ECC, 43.3% of participants reported they were unaware of the existence of this disease. A statistically significant association was found between this variable and both the level of education (p=0.034; χ2=14.283) and the environment where they lived (rural/urban) (p=0.015; χ2=8.501); the latter association was also found when considering only women in first pregnancies (p=0.027; χ2=7.340) (Table 4). When asked about the relationship between caries and nocturnal breastfeeding, 37.5% of respondents stated they did not know whether they were related and 46.7% thought they were unrelated (Table 4).
�
Table 4. Knowledge of the pregnant woman regarding the child�s oral health.
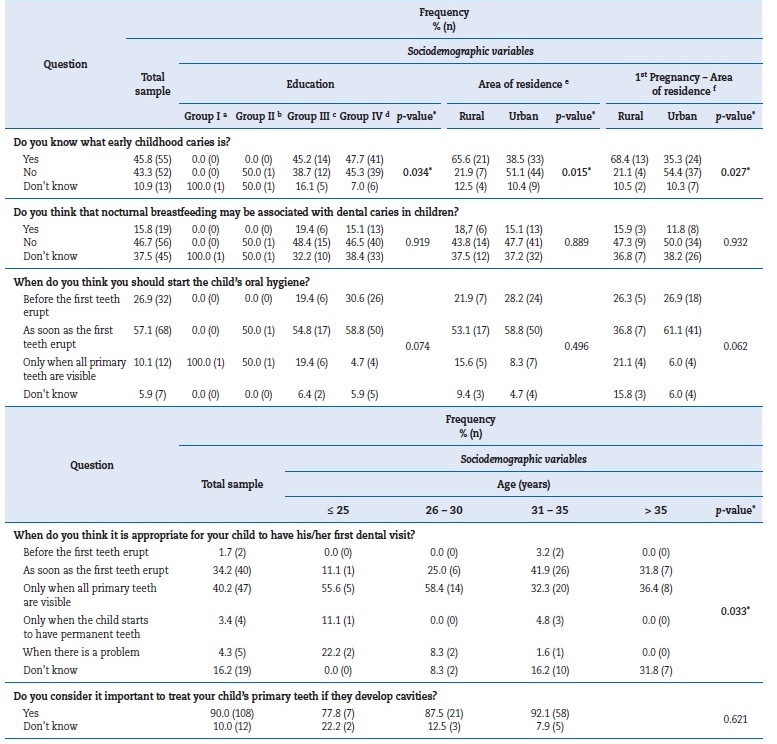
* Chi‑square test (χ2) under a 95% confidence interval (p<0.05)
a Group I: Primary - 1st Cycle (up to 4 years of schooling)
b Group II: Lower Secondary (up to 9 years of schooling)
c Group III: Upper Secondary (up to 12 years of schooling)
d Group IV: Higher Education (university level)
e n = 118. Two participants did not answer this question.
f n = 88
The majority of participants (84.0%) considered that the appropriate time to start oral hygiene is before or as soon as the first teeth erupt (Table 4). However, only 35.9% of expectant mothers considered the first dental appointment should occur before or as soon as the child�s first teeth erupt. Some participants stated the child�s first dental visit should occur only when all primary teeth are visible (40.2%), when there is a problem (4.3%), or when the child has permanent teeth (3.4%) (Table 4). A statistically significant association was found between this variable and age (p=0.033; χ2=27.287). Most respondents (90.0%) recognized the importance of treating injuries to primary teeth (Table 4).
Discussion
The present study aimed to assess the effect of maternal knowledge and practices on prenatal and infant oral health, with a survey of pregnant women followed in two Portuguese public health institutions.
From the results, most pregnant women reported toothbrushing twice daily. Previous studies have reported a correlation between this practice and higher levels of education,7, 23, 25, 30 and indeed, most of this study�s sample reported having attended higher education (71.7%). However, 36.4% of participants said they did not floss, which is consistent with findings from a previous report among expectant women in Portugal.29 Most notably for this study, those under 25 years old were more likely not to use floss, thus highlighting the importance of hygienic instruction and motivation.
Although only a minority reported never having gone to a dental consultation, half the respondents had not visited the dentist before becoming pregnant. The latter finding is, unfortunately, in line with previously reported practices.8, 9, 29 This negligence happens despite the known established effect of prenatal oral health care on preventing adverse birth outcomes and ECC onset.11, 16 Nonetheless, most participants stated they would undergo dental treatment during pregnancy if needed. While these results may reveal that the women surveyed were aware that dental treatment during pregnancy was safe, another possible explanation is the misconception, supported by over half of the participants, that pregnancy can be potentially harmful to their oral health. This result is consistente with previous findings from another cohort followed in the same public maternity practice, where the persistence of myths about the effects of pregnancy on oral health was also reported, particularly an increased tendency for dental demineralization and tooth loss.28
Additional knowledge gaps were identified, as more than half of the pregnant women were unaware that gingivitis or periodontitis could contribute to premature birth and low birth weight, corroborating the findings of previous international surveys.17, 31 Insufficient knowledge regarding the importance of diet in oral health was found among most respondents, despite dietary factors being fundamental to the etiology of multiple oral pathologies, both for pregnant women and children.21, 32, 33
Lamentably, it was evident that a high proportion of the cohort was not familiar with ECC. Similar to earlier reports, most participants in this study also said that caries was not communicable or did not know whether it was. This finding possibly reveals an unawareness that early acquisition of Mutans Streptococc is a key risk factor for developing ECC. 14 - 16, 29, 34, 35 The fact that mother-to-child (or caregiver-to-child) transmission constitutes the major pathway for Mutans Streptococci initial acquisition underlines the importance of education and prenatal oral health care in reducing maternal carriage of Mutans Streptococci and limiting saliva-sharing activities, as highlighted by recent studies.14 - 16, 33
A substantial number of pregnant women stated that nocturnal breastfeeding was not associated with the etiology of ECC. In fact, although multiple studies have explored the potential impact of prolonged and ad libitum breastfeeding on ECC�s development, recent evidence from a systematic review suggests that breastfeeding does not increase ECC risk.21, 36
Regarding perinatal oral health care, most pregnant women recognized the importance of treating primary teeth and stated their intention to establish toothbrushing habits before or as soon as the first teeth erupted, a finding in line with those of Ferreira et al.29 Nonetheless, while one-third of the sample intended that their child first visited the dentist as soon as teeth erupted, a large proportion of participants reported an intention to visit the dentist only when all of the child�s primary teeth were present. Another concerning finding is that a non-negligible share of participants stated they did not know when the first dental appointment should occur.
Such lack of knowledge reduces the likelihood of establishing a dental home during the child�s first year of life, a crucial recommendation for establishing oral health preventive and/or curative strategies.4, 33, 37, 38
This research presented some limitations. Firstly, there are known possible drawbacks of questionnaire-based studies: nonresponses, misconceptions, and socially desirable answers.
Another limitation is related to the nature of the cohort, particularly the asymmetric distribution of sociodemographic characteristics. Despite recognizing that the present sample cannot be considered representative of all pregnant women in Portugal, to the best of our knowledge, this study involved a considerably larger sample than the few published surveys among Portuguese cohorts.28, 29
Even though our results generally reflect those found in the international literature,7 17 19 21 - 27 30 39 such a comprehensive characterization of oral health-related knowledge and the practices of expectant mothers has not been reported for Portuguese cohorts. This work enabled the identification of importante gaps and illustrated the urgent need for prenatal education and promotion of oral health in Portugal.
Conclusions
Most pregnant women taking part in this study believed pregnancy could be harmful to their oral condition, and a significant proportion did not seek prenatal oral health care. Surveyed women also lacked knowledge of the potential impact of their periodontal status on gestation and were unaware of the existence of ECC and the need for its prevention, particularly regarding concepts such as vertical transmission and the establishment of a dental home. This study population showed a clear demand for the implementation of educational programs aimed at increasing awareness and understanding on these matters.
�
References
1. Barak S, Oettinger-Barak O, Oettinger M, Machtei EE, Peled M, Ohel G. Common oral manifestations during pregnancy: A review. Obstet Gynecol Surv. 2003;58:624-8.
2. Figueiredo CSA, Rosalem CGC, Cantanhede ALC, Thomaz �BAF, Cruz MCFN. Systemic alterations and their oral manifestations in pregnant women. J Obstet Gynaecol Res. 2017;43:16-22.
3. Oliveira JFM, Gon�alves PE. Verdades e mitos sobre o atendimento odontol�gico da paciente gestante. Rev Port Estomatol Med Dent Cir Maxilofac. 2009;50:165-71.
4. Steinberg BJ, Hilton I, Iida H, Samelson R. Oral Health and Dental Care During Pregnancy. Dent Clin North Am. 2013;57:195-210.
5. American College of Obstetricians and Gynecologists Women�s Health Care Physicians; Committee on Health Care for Underserved Women. Committee Opinion No. 569: oral health care during pregnancy and through the lifespan. Obstet Gynecol. 2013;122:417-22.
6. Frias-Bulhosa J. Sa�de Oral e Gravidez. Rev Port Estomatol Med Dent Cir Maxilofac. 1998;39:233-42.
7. Hom JM, Lee JY, Divaris K, Baker AD, Vann WF. Oral health literacy and knowledge among patients who are pregnant for the first time. J Am Dent Assoc. 2012;143:972-80.
8. Naseem M, Khurshid Z, Khan HA, Niazi F, Zohaib S, Zafar MS. Oral health challenges in pregnant women: Recommendations for dental care professionals. Saudi J Dent Res. 2016;7:138-46.
9. Rocha JS, Arima LY, Werneck RI, Moys�s SJ, Baldani MH. Determinants of Dental Care Attendance during Pregnancy: A Systematic Review. Caries Res. 2018;52:139-52.
10. Vamos CA, Thompson EL, Avendano M, Daley EM, Quinonez RB, Boggess K. Oral health promotion interventions during pregnancy: A systematic review. Community Dent Oral Epidemiol. 2015;43:385-96.
11. Iheozor-Ejiofor Z, Middleton P, Esposito M, Glenny AM. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst Rev. 2017;6:CD005297.
12. Manrique-Corredor EJ, Orozco-Beltran D, Lopez-Pineda A, Quesada JA, Gil-Guillen VF, Carratala-Munuera C. Maternal periodontitis and preterm birth: Systematic review and meta-analysis. Community Dent Oral Epidemiol . 2019;47:243-51.
13. Bi WG, Emami E, Luo ZC, Santamaria C, Wei SQ. Effect of periodontal treatment in pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Matern Neonatal Med. 2019 Oct 21;1-10. Epub ahead of print.
14. Chaffee BW, Gansky SA, Weintraub JA, Featherstone JDB, Ramos-Gomez FJ. Maternal oral bacterial levels predict early childhood caries development. J Dent Res. 2014;93:238-44.
15. Bastos VAS, Freitas-Fernandes LB, Fidalgo TKS, Martins C, Mattos CT, Souza IPR, et al. Mother-to-child transmission of Streptococcus mutans: A systematic review and metaanalysis. J Dent. 2015;43:181-91.
16. Xiao J, Alkhers N, Kopycka-Kedzierawski DT, Billings RJ, Wu TT, Castillo DA, et al. Prenatal Oral Health Care and Early Childhood Caries Prevention: A Systematic Review and Meta-Analysis. Caries Res . 2019;53:411-21.
17. Boggess KA, Urlaub DM, Moos MK, Polinkovsky M, El-Khorazaty J, Lorenz C. Knowledge and beliefs regarding oral health among pregnant women. J Am Dent Assoc . 2011;142:1275-82.
18. Lin DL, Harrison R, Aleksejuniene J. Can a prenatal dental public health program make a difference? J Can Dent Assoc. 2011;77:b32.
19. Mart�nez-Beneyto Y, Vera-Delgado M, P�rez L, Maurandi A. Self-reported oral health and hygiene habits, dental decay, and periodontal condition among pregnant European women. Int J Gynecol Obstet. 2011;114:18-22.
20. Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent Oral Epidemiol . 2008;36:335-46.
21. ElKarmi R, Aljafari A, Eldali H, Hosey MT. Do expectante mothers know how early childhood caries can be prevented? A cross-sectional study. Eur Arch Paediatr Dent. 2019;20:595-601.
22. Villa A, Abati S, Pileri P, Calabrese S, Capobianco G, Strohmenger L, et al. Oral health and oral diseases in pregnancy: A multicentre survey of Italian postpartum women. Aust Dent J. 2013;58:224-9.
23. Abiola A, Olayinka A, Mathilda B, Ogunbiyi O, Modupe S, Olubunmi O. A survey of the oral health knowledge and practices of pregnant women in a Nigerian teaching hospital. Afr J Reprod Health. 2011;15:14-9.
24. Detman LA, Cottrell BH, Denis-Luque MF. Exploring Dental Care Misconceptions and Barriers in Pregnancy. Birth. 2010;37:318-24.
25. Avula H, Mishra A, Arora N, Avula J. KAP assessment of oral health and adverse pregnancy outcomes among pregnant women in Hyderabad, India. Oral Health Prev Dent. 2013;11:261-70.
26. Pentapati KC, Acharya S, Bhat M, Rao SVK, Singh S. Knowledge of dental decay and associated factors among pregnant women: A study from rural india. Oral Health Prev Dent . 2013;11:161-8.
27. Rothnie JJ, Walsh CA, Wang MJ-J, Morgaine KC, Drummond BK. An exploratory study of pregnant women�s knowledge of child oral health care in New Zealand. N Z Dent J. 2012;108:129-33.
28. Antunes A, Rosete V, Fagulha J. Sa�de Oral na Gr�vida. Acta Med Port. 2001;14:385-93.
29. Ferreira A, Oliveira C, Silva L, Santiago M, Veiga N. The Importance of Oral Health during Pregnancy and Among the Newborn. Matern Pediatr Nutr J. 2018;4:2017-8.
30. Llena C, Nakdali T, Sanz JL, Forner L. Oral Health Knowledge and Related Factors among Pregnant Women Attending to a Primary Care Center in Spain. Int J Environ Res Public Health. 2019;16:5049.
31. Daalderop LA, Wieland B, Tomsin K, Reyes L, Kramer BW, Vanterpool SF, et al. Periodontal disease and pregnancy outcomes: Overview of systematic reviews. JDR Clin Trans Res. 2018;3:10-27.
32. Murphey C, Fowles E. Dental health, acidogenic meal, and snack patterns among low-income women during early pregnancy: A pilot study. J Midwifery Womens Health. 2010;55:587-92.
33. Finlayson TL, Gupta A, Ramos-Gomez FJ. Prenatal Maternal Factors, Intergenerational Transmission of Disease, and Child Oral Health Outcomes. Dent Clin North Am . 2017;61:483-518.
34. Ramos GMS, Castro LB, Rocha CT, Neves BG. Pregnant women�s knowledge of baby�s oral health in a basic health unit, Fortaleza, Brazil. Brazilian Res Pediatr Dent Integr Clin. 2014;14:239-48.
35. Rigo L, Dalazen J, Garbin RR. Impact of dental orientation given to mothers during pregnancy on oral health of their children. Einstein (Sao Paulo). 2016;14:219-25.
36. Moynihan P, Tanner LM, Holmes RD, Hillier-Brown F, Mashayekhi A, Kelly SAM, et al. Systematic Review of Evidence Pertaining to Factors That Modify Risk of Early Childhood Caries. JDR Clin Trans Res . 2019;4:202-16.
37. American Academy of Pediatric Dentistry. Policy on the dental home. Pediatr Dent.2018;40:29-30.
38. American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): Classifications, consequences, and preventive strategies. Pediatr Dent . 2017;39:59-61.
39. Hashim R. Self-reported oral health, oral hygiene habits and dental service utilization among pregnant women in United Arab Emirates. Int J Dent Hyg. 2012;10:142-6.
�
Margarida Esteves
E-mail address: margarida.esteves022@gmail.com
�
Acknowledgments
The authors would like to thank Dr. Ondina Jardim, Graduate Hospital Assistant at the Coimbra Hospital and University Centre practicing at Daniel de Matos Maternity, for her support and assistance with data collection, as well as all pregnant women who accepted to participate in this study and Prof. Julian Tice for the text translation and final revision.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
1646-2890/� 2021 Sociedade Portuguesa de Estomatologia e Medicina Dent�ria. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
