
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2021 | 62 (1) | 9-15
Original research
Influence of implant design, length, diameter, and anatomic region on implant stability: a randomized clinical trial
Influência do comprimento, diâmetro e desenho do implante e da região anatómica na estabilidade implantar: ensaio clínico randomizado
a Specialization in Implantology, Faculdade de Medicina Dentária da Universidade de Lisboa, Lisbon, Portugal
b Department of Oral Surgery and Implant Dentistry, Faculdade de Medicina Dentária da Universidade de Lisboa, Lisbon, Portugal
c Department of Biostatistics, Faculdade de Medicina Dentária da Universidade de Lisboa, Lisbon, Portugal
d Implantology Institute, Lisbon, Portugal
e Center for Innovative Care and Health Technology (ciTechcare), Polytechnic of Leiria, Leiria, Portugal
André Moreira - andregonmoreira@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 62
Issue - 1
Original research
Pages - 9-15
Go to Volume
Article History
Received on 22/04/2020
Accepted on 29/11/2020
Available Online on 04/01/2021
Keywords
Original Research
�
Influence of implant design, length, diameter, and anatomic region on implant stability: a randomized clinical trial
Influ�ncia do comprimento, di�metro e desenho do implante e da regi�o anat�mica na estabilidade implantar: ensaio cl�nico randomizado
�
Andr� Moreirab,d,*, Jos� Rosaa, Filipe Freitasb,d, Helena Franciscob,d, Henrique Lu�sc,e, Jo�o Caram�sb,d
a Specialization in Implantology, Faculdade de Medicina Dent�ria da Universidade de Lisboa, Lisbon, Portugal
b Department of Oral Surgery and Implant Dentistry, Faculdade de Medicina Dent�ria da Universidade de Lisboa, Lisbon, Portugal
c Department of Biostatistics, Faculdade de Medicina Dent�ria da Universidade de Lisboa, Lisbon, Portugal
d Implantology Institute, Lisbon, Portugal
e Center for Innovative Care and Health Technology (ciTechcare), Polytechnic of Leiria, Leiria, Portugal�
�
Article history:
Received 22 April 2020
Accepted 29 November 2020
Available online 4 January 2021
�
AbstractObjectives: To evaluate the influence of implant geometry and anatomical region on implant stability.
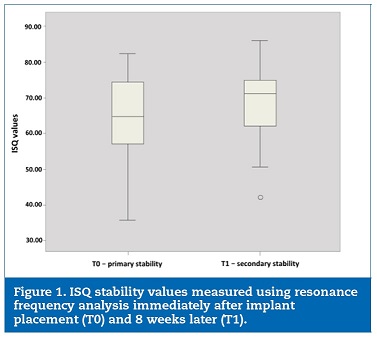
Methods: A randomized controlled clinical trial was conducted on 45 patients, in whom a total of 79 implants were placed: 40 MIS C1 Implants and 39 MIS Seven Implants. The implant stability quotient was measured using resonance frequency analysis immediately after implant placement and 8 weeks later with an Osstell Mentor device.
Results: 76 implants were analyzed. The implant stability quotient was statistically significantly higher for secondary stability than primary stability (68.7�}8,6 vs. 65.2�}10.3, respectively, p=0.023). Considering primary stability, no statistical differences were found between the implant lengths 8.0 mm, 10.0 mm, 11.0 mm, and 11.5 mm (67.9�}7.6, 63.9�}10, 57.2�}11.1, and 66.4�}11.3, respectively, p=0.312). The same was observed for secondary stability (68.4�}9.4, 67.9�}9.3, 74.7�}1.5, and 69.2�}7.9, respectively, p=0.504). Also, there were no statistically significant differences between the implant diameters 3.75 mm and 4.20 mm concerning primary stability (64.3�}8.7 and 66.1�}11.7 respectively, p=0.445) or secondary stability (68.8�}8.2 and 68.7�}9.1 respectively, p=0.930). Regarding implant design, a statistically significant difference was found only for secondary stability, favoring MIS Seven implants (p=0.048). The intraoral location was statistically significant for both primary and secondary stability, as these were higher on the anterior maxilla than the posterior maxilla and mandible (p<0.05).
Conclusions: The diameter and length of the implants studied did not influence their stability. Implant design may influence secondary stability, whereas intraoral location has a relevant effect on primary and secondary stability.
Keywords: Implant design,Implant diameter,Implant length, Implant stability,Osseointegration,� Resonance frequency analysis
�
ResumoObjetivos: Avaliar a influencia da geometria dos implantes e regi�o anat�mica na estabilidade implantar.
M�todos: Foi realizado um ensaio clinico controlado aleatorizado em 45 pacientes, onde foram colocados 79 implantes: 40 implantes MIS C1 e 39 implantes MIS Seven. O coeficiente de estabilidade do implante foi medido atrav�s da analise de frequ�ncia de resson�ncia (RFA) imediatamente apos a coloca��o do implante e 8 semanas depois, com Osstell Mentor.
Resultados: Foram analisados 76 implantes. O coeficiente de estabilidade do implante registado para estabilidade secundaria foi significativamente maior que o verificado para a estabilidade primaria (68,7�}8,6 e 65,2�}10,3, p=0,023). Considerando a estabilidade primaria, n�o foi encontrada diferen�a estatisticamente significativa entre os comprimentos de 8,0 mm, 10,0 mm, 11,0 mm e 11,5 mm (67,9�}7,6, 63,9�}10, 57,2�}11,1 e 66,4�}11,3, p=0,312). O mesmo foi verificado para a estabilidade secundaria (68,4�}9,4, 67,9�}9,3, 74,7�}1,5 e 69,2�}7,9, p=0,504). N�o se observou diferen�a estatisticamente significativa entre os di�metros dos implantes de 3,75 e 4,20 mm e estabilidade primaria (64,3�}8,7 e 66,1�}11,7, p=0,445) ou estabilidade secundaria (68,8�}8,2 e 68,7�}9,1, p=0,930). Foi encontrada diferen�a estatisticamente significativa para a estabilidade secundaria, favorecendo o implante MIS Seven (p=0,048). A localiza��o intraoral foi estatisticamente significativa para a estabilidade primaria e secundaria, sendo maior na maxila anterior em rela��o a maxila e mand�bula posteriores (p<0,05).
Conclus�es: O di�metro e o comprimento dos implantes estudados n�o influenciaram sua estabilidade. O tipo do implante parece influenciar a estabilidade secundaria, enquanto a regi�o anat�mica aparenta ter um efeito relevante na estabilidade prim�ria e secundaria.
Palavras-chave: Desenho do implante,Di�metro do implante,Comprimento do implante,Estabilidade do implante,Osseointegra��o,Analise de frequ�ncia de resson�ncia
Introduction
The use of dental implants is a widespread treatment option for the replacement of missing teeth.1 This treatment�s predictability is directly related to osseointegration, which has been defined as the direct structural and functional connection between bone and the surface of a dental implant.2 Some of the most relevant factors for the osseointegration of dental implants are achieving and maintaining implant stability.2 Insufficient implant stability has been cited as the greatest potential risk factor for implant loss.3, 4
The implant stability can be measured in two different stages: primary and secondary stability.5 Primary stability is the initial biometric stability obtained immediately after implant insertion that results from the mechanical attachment within the bone and seems to be affected by bone quality and quantity, surgical technique, and implant geometry.3 Secondary stability offers biological stability through bone regeneration and remodeling and seems to be highly affected by primary stability.6
The objective measurement of implant stability is important to evaluate the clinical outcome of dental implant treatments throughout implant healing and loading. There are several methods to assess implant stability that can be grouped as invasive and non‑invasive.3 The invasive methods include histologic and histomorphologic analysis, tensional test, push‑and pull‑out test, and removal torque analysis3, 7 The non‑invasive methods for assessing implant stability include radiographic analysis with imaging techniques, cutting torque resistance, insertion torque measurement, reverse torque, modal analysis, percussion test, pulsed oscillation waveform, resonance frequency analysis, and magnetic technology.3
Developed by Meredith et al. in 1996, the resonance frequency analysis (RFA) is a reliable and easily predictable non‑invasive objective method for quantifying primary and secondary implant stability.8, 9 It measures implant stability as a reaction to oscillations exerted onto the implant/bone interface, providing a unit of measurement known as the implant stability quotient (ISQ), expressed in a range from 0 to 100.5
According to several studies, RFA is a highly effective non‑invasive method to determine dental implants� stability during the healing and follow‑up treatment stages.10 ‑ 12 Previous research reported that ISQ levels for successfully osseointegrated implants fluctuate between 57 and 82, whereas implants with ISQ values lower than 50 have a high risk of failure.13
Published results on the relationship between implant stability, design, length, and diameter are controversial. Previous research has shown that lower stability was obtained with longer implant lengths.(14) Other investigations obtained different results, concluding that implant length has no significant effect on implant stability.15 However, those authors concluded that ISQ values increased with increased implant diameter, and tapered implants showed higher ISQ values than parallel implants. Given the diversity of the current results, it is important to carry out a clinical trial that simultaneously studies the different factors that appear to influence implant stability.
Therefore, this randomized controlled clinical trial aims to evaluate the influence of implant length, diameter, design, and anatomic region on ISQ values during osseointegration. The research hypothesis was that ISQ values are affected by jaw region, implant diameter, implant length, and implant design.
Material and Methods
A prospective, randomized, parallel‑group, controlled clinical trial was carried out at the Implant Dentistry Postgraduate Program of the Faculty of Dental Medicine of the University of Lisbon (FMDUL), Lisbon, Portugal. Inclusion criteria were adults with good general health, non‑smokers, with at least one tooth missing for more than 6 months and sufficient bone height/width for implant placement without the need for bone augmentation. Exclusion criteria included patients with uncontrolled systemic diseases, history of head/neck irradiation, immune system severe deficiencies, smokers, and patients treated with oral/intravenous bisphosphonates.
Using G*Power (version 3.1.9.4, Heinrich‑Heine‑University, Germany), a minimum sample size of 70 implants was calculated as required to detect comparisons between the two groups, considering a statistical power of 80% and estimated dropouts. The eligible patients were randomly allocated into two different groups by simple randomization (using GraphPad Software, QuickCalcs � website http://www.graphpad.com) according to implant design: Group A � C1 implants (MIS Implants Technologies Ltd) and Group B � Seven implants (MIS Implants Technologies Ltd). The study was approved by the Ethics Committee of the FMDUL, Lisbon, Portugal. All procedures followed the standards of the Helsinki Declaration of 1975, as revised in 2000.
All patients were fully informed of the nature of the study and signed an informed consent form. A total of 79 implants were placed: 40 MIS C1 implants and 39 MIS Seven implants (MIS Implants Technologies Ltd). All implants had the same surface: sandblasted and acid‑etched surface. C1 implants feature a 12‑degree conical connection that ensures a secure fit between abutment and implant. The C1 implant has a dual thread design (range 1.5 mm) over the entire implant body. The apical region of C1 implant features two cutting blades establishing the self‑tapping properties.
Seven implants� apical region features an internal hexagon connection and a dual thread design (range 2 mm), sharper at the apex and gradually lessening toward the neck. Both implants have conical root‑shaped geometry and micro‑rings at the neck.
All surgeries were performed by postgraduate students of the Implantology Postgraduate Program, FMDUL, Lisbon, Portugal, under the supervision of surgery instructors. Imaging techniques (panoramic and intraoral radiographs, dental computerized tomographs) were applied for all patients for proper pre‑surgical planning.
Immediately before surgery, the mouth was rinsed with a 0.12% chlorhexidine solution (Eludril, Laboratoires Pierre Fabre, France) for 1 minute. The surgical procedures were done under local anesthesia (articaine containing 1:100000 epinephrine � Artinibsa, Inibsa), using loco‑regional or infiltrative anesthesia techniques, according to the anatomical region. A midcrestal incision was made, and a full‑thickness flap was obtained.
The implants were placed according to the manufacturer�s instructions. A one‑stage surgical protocol with non‑immediate loading was planned for this study. For definition purposes, implants placed in the �anterior� region were meant to replace central and lateral incisors and canines, whereas those in the �posterior� region were placed to replace premolars and molars. Implants were surgically positioned with the implant shoulder at the level of the alveolar bone crest. Primary closure of the wound was made using 3‑0 polyglactin 910 single sutures (Vicryl Rapide, Ethicon). Post‑operative antibiotic (amoxicillin, 1 g, 12/12 hours for 8 days) and analgesic (paracetamol, 1 g, 8/8 hours for 2 days) were prescribed. All patients were instructed to follow a soft cold diet for the first 24 hours and mouthwash with chlorhexidine 0.2% for a week.
RFA was employed to measure implant stability. RFA measurements were taken immediately after implant placement (T0) and 8 weeks later (T1), using the Osstell Mentor device (Ostell Integration Diagnostics, Goteborg, Sweden). For each implant, ISQ values were measured from the three orientations (buccal, lingual, and occlusal), according to the method described by Rokn.15 The mean of all measurements was regarded as the final ISQ of the implant. A single operator made all measurements and recordings.
Data were analyzed using IBM SPSS Statistics version 25.0 (IBM Corp., Armonk, NY, USA). The t‑test or Mann‑Whitney U test and ANOVA or Kruskal‑Wallis tests were used according to groups of variables, normality of the distribution, and homogeneity of variance. The t‑test was used for groups of two qualitative variables with normal distribution, and the Mann‑Whitney U test was applied if they had a non‑normal distribution.
ANOVA was used for groups of three or more variables if the distribution was normal and variance was homogeneous; if not, Kruskal‑Wallis was applied. The level of significance was set at p <0.05. Multiple comparisons were made to identify significant differences between groups. The quantitative variables analyzed were mean primary stability and mean secondary stability.
Results
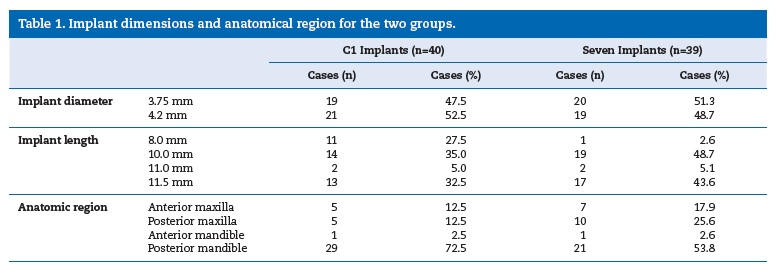
A total of 45 patients (28 women and 17 men) with an average age of 46 years were included and received 79 implants. No dropouts were registered. The number of implants inserted was 47 (59.5%) in women and 32 (40.5%) in men. The implants� length was 8.0 mm, 10.0 mm, 11.0 mm, and 11.5 mm, and
their diameter was 3.75 mm and 4.20 mm. Of the 79 implants studied, 3 MIS Seven implants were excluded due to osseointegration failure, reaching an overall implant survival rate of 96.2%. The anatomical region for implantation, implant types, and implant dimensions are listed in Table 1.
�
�
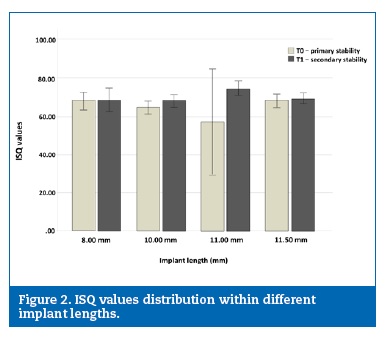
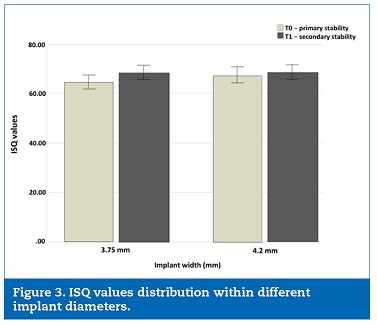
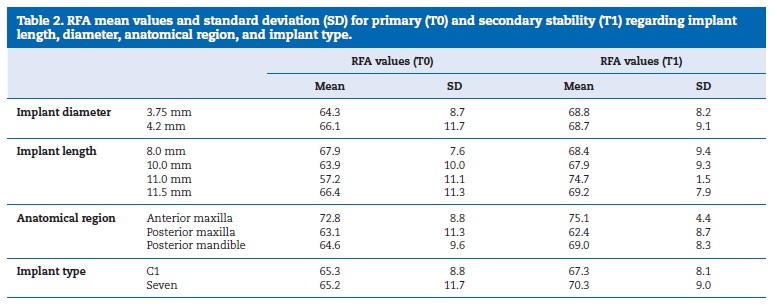
Mean ISQ values were 65.2�}10.3 at implant placement and increased statistically significantly after 8 weeks (p=0.023), with a mean of 68.7�}8.6 (Figure 1). Descriptive statistics of ISQ values distribution regarding implant length and diameter are reported in Figures 2 and 3, respectively. When considering the overall primary stability (T0) and implant length (8.0 mm, 10.0 mm, 11.0 mm, and 11.5 mm), no statistically significant relationship was observed between length and ISQ values (67.9�}7.6, 63.9�}10, 57.2�}11.1, and 66.4�}11.3, p=0.312). Also, no relationship was found between the implant width (3.75 mm and 4.2 mm) and the ISQ values (64.3�}8.7 and 66.1�}11.7, p=0.445). Regarding implant types, no statistically significant differences were found in the mean primary stability between the two designs of implants studied (65.3�}8.8 for MIS C1 implant and 65.2�}11.8 for MIS Seven implant, p=0.962).
Analysis of the experimental data also revealed that secondary stability was not affected by implant length or width.
�
�
�
�
No significant differences were observed when comparing the ISQ values for secondary stability between different implant lengths (p=0.504). Similarly, there was no correlation between the implants� diameter and the ISQ values for secondary stability (p=0.930). However, different results were obtained when considering the implant design. The secondary stability ISQ values measured for the MIS Seven implant type were significantly higher than those measured for MIS C1 implants (p=0.048). ISQ values measured for primary and secondary stability related to implant length, diameter, and implant design are listed in Table 2.
�
�
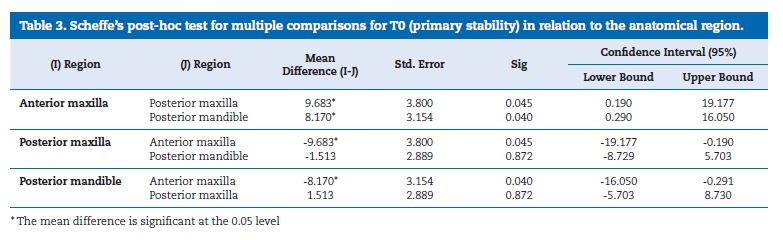
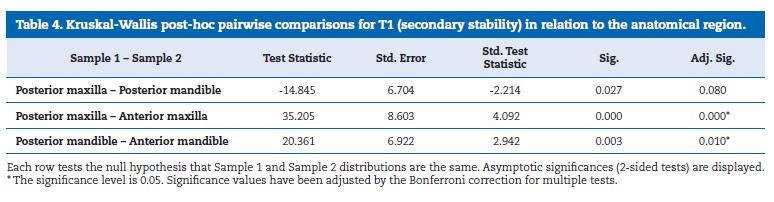
In respect to the anatomical region, implants were distributed in the anterior maxilla (15.2%), posterior maxilla (19.1%), anterior mandible (2.6%), and posterior mandible (63.1%). According to the data obtained, there was a statistical difference between anatomical regions of implantation and primary and secondary stability (p<0.05). However, no conclusions could be drawn when making multiple comparisons due to insufficient data from the anterior mandible; thus, these data were not considered. The ISQ values for both primary stability and secondary stability at the T0 and T1 measurements were significantly higher in the anterior maxilla than in posterior regions of the maxilla and mandible (p=0.045 and p=0.040, respectively).
The significance of differences between anatomical regions is reported in Tables 3 and 4.
�
�
�
Discussion
This study aimed to determine how the implant design, length, diameter, and anatomical region affect the primary and secondary stability measured by RFA. Our findings suggest that the length and diameter of the implants studied did not influence their stability. Moreover, implant design may influence secondary stability, whereas intraoral location has a relevant effect on primary and secondary stability.
The effect of implant length on primary stability and implant�s long‑term prognosis has been a controversial issue.
Some studies showed that short implants failed more often than longer implants, while others reported that implant length did not significantly influence implant survival rates.(16) Moreover, some studies suggested that increasing implant length plays an important role in decreasing bone stress and increasing implant stability in poor quality bone areas.17 Likewise, some authors reported that implant diameter influenced ISQ values,18 whereas others reported no differences.19, 20
In the present clinical study, the primary and secondary stability were evaluated in two types of implant designs (MIS C1 implants and MIS Seven implants) at implant placement and after a healing period. This study concluded that the implants� length was not significant for primary or secondary stability. These conclusions are in agreement with previous research that found no correlation between implant length and stability.21 Regarding implant diameter, the results also showed no statistical difference on ISQ values between the different diameters for both primary and secondary stability.
These data agree with prior studies that found no correlation between implant diameter and implant stability.22
The perception that longer and larger implants have greater stability may not be accurate. Implant design and the surrounding bone may have a more significant effect on implant stability. The implant body design and the thread geometry are significant for improving the mechanical implant stability.23
Within the limitations of this study, the implant design appears to play a role in implant stability measured after a healing period.
In respect to the bone region, the present study observed that implants placed in the anterior region had more primary stability than implants placed in the posterior regions of the maxilla or mandible. The secondary stability was also poorer in the posterior areas of the jaws. The reason for this may be related to low bone density, which causes decreased implant stability. The poorer implant stability in the posterior area might explain the lower implant success rates reported in the posterior maxilla than in the other regions. 24 In the present study, the three implants that failed were placed in posterior regions of the jaws. The posterior maxilla�s reduced bone density and the challenges of mandibular posterior blood supply may explain these failures.
These results agree with those of a previous investigation that found that implants placed in the anterior region had lower failure rates than implants placed in the jaws� posterior region.25 In a more recent study, no differences were found in ISQs regarding bone types, except between D2 and D3, according to Misch�s classification.26 Some authors stated that, in cases of low bone quality, an optimum increase in implant length and diameter should be taken into account to achieve higher primary stability.27
Limited data is available concerning the influence of implant design on implant stability. A randomized clinical trial found a small initial advantage of conical implants with wide pitch compared to semiconical implants and narrow pitch.28
However, after 90 days, both implant designs showed similar stability. In the present study, the implant design significantly influenced the ISQ values on secondary rather than primary stability.
Besides the implant geometry, length, or diameter, other parameters have to be considered regarding implant stability and success of dental implants, namely the bone quality, the surgical technique, or the insertion torque. The results of the present study sho\uld be confirmed with a larger number of implants, in bone substrates of different densities and with different implant designs.
More long‑term controlled clinical trials are needed to confirm the outcomes of the present study, with more patients and fixtures inserted and longer follow‑ups, to formulate clear guidelines for implant stability and the success of dental implants.
Conclusions
Within the limitations of this study, it can be concluded that, rather than the diameter or length of implants, the anatomical region of implantation has a relevant effect on both primary and secondary stability of dental implants.
�
Acknowledgements
The authors would like to thank Andre Chen, Antonio Carvalho and Joao Canta, who participated in this investigation.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest.The authors have no conflicts of interest to declare.
�
References
1. Marković A, Calvo‑Guirado JL, Lazić Z, Gomez‑Moreno G, Ćalasan D, Guardia J, Čolic S, Aguilar‑ Salvatierra A, Gačić B, Delgado‑Ruiz R, Janjić B, Mi�ić T. Evaluation of primary stability of self‑tapping and non‑self‑tapping dental implants. A 12‑week clinical study. Clin Implant Dent Relat Res. 2013;15:341‑9.
2. Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants: a review of the literature. Int J Prosthodont. 1998;11:408‑20.
3. Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016;16:124‑30.
4. Friberg B, Jemt T, Lekholm U. Early failures in 4,641 consecutively placed Branemark dental implants: a study from stage 1 surgery to the connection of completed prostheses. Int J Oral Maxillofac Implants. 1991;6:142‑6.
5. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998;11:491‑501.
6. Cochran D, Schenk R, Lussi A, Higginbottom F, Buser D. Bone response to unloaded and loaded titanium implants with a sandblasted and acid‑etched surface: a histometric study in the canine mandible. J Biomed Mater Res. 1998;40:1‑11.
7. Guler A, Sumer M, Duran I, Sandikci E, Telcioglu N. Resonance frequency analysis of 208 Straumann dental implants during the healing period. J Oral Implantol. 2013;39:161‑7.
8. Meredith N, Alleyne D, Cawley P. Quantitative determination of the stability of the implant‑tissue interface using resonance frequency analysis. Clin Oral Implants Res. 1996;7:261‑7.
9. O�Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000;2:85‑92.
10. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008;47:51‑66.
11. Friberg B, Sennerby L, Meredith N, Lekholm U. A comparison between cutting torque and resonance frequency measurements of maxillary implants. A 20‑month clinical study. Int J Oral Maxillofac Surg. 1999;28:297‑303.
12. Gahona O, Granic X, Antunez C, Domancic S, Diaz‑Narvaez V, Utsman R. Insertion torque and resonance frequency analysis (ISQ) as predictor methods of implant osseointegration. J Osseointegr 2018;10:103‑7.
13. Huang H, Lee S, Yeh C, Lin C. Resonance frequency assessment of dental implant stability with various bone qualities: a numerical approach. Clin Oral Implants Res. 2002;13:65‑74.
14. Ostman P, Hellman M, Wendelhag I, Sennerby L. Resonance frequency analysis measurements of implants at placement surgery. Int J Prosthodont. 2006;19:77‑83.
15. Rokn A, Ghahroudi A, Mesgarzadeh A, Miremadi A, Yaghoobi S. Evaluation of Stability Changes in Tapered and Parallel Wall Implants: A Human Clinical Trial. J Dent. 2011;8:186-200.
16. Kotsovilis S, Fourmousis I, Karoussis IK, Bamia C. A systematic review and meta‑analysis on the effect of implant length on the survival of rough‑ surface dental implants. J Periodontol. 2009;80:1700‑18.
17. Kong L, Sun Y, Hu K, Li D, Hou R, Yang J et al. Bivariate evaluation of cylinder implant diameter and length: a three‑dimensional finite element analysis. J Prosthodont. 2008;17:286‑93.
18. Park K, Kwon J, Kim S, Heo S, Koak J, Lee J et al. The relationship between implant stability quotient values and implant insertion variables: a clinical study. J Oral Rehab. 2012;39:151‑9.
19. Han J, Lulic M, Lang N. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: II. Implant surface modifications and implant diameter. Clin Oral Implants Res. 2010;21:605�11.
20. Aragoneses J, Suarez A, Brugal V, Gomez M. Frequency Values and Their Relationship With the Diameter of Dental Implants. Prospective Study of 559 Implants. Implant Dent. 2019;28:279‑88.
21. Balleri P, Cozzolino A, Ghelli L, Momicchioli G, Varriale A. Stability measurements of osseointegrated implants using Osstell in partially edentulous jaws after 1 year of loading: a pilot study. Clin Implant Dent Relat Res. 2002;4:128-32.
22. Shiffler K, Lee D, Rowan M, Aghaloo T, Pi‑Anfruns J, Moy P. Effect of length, diameter, intraoral location on implant stability. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122:193‑8.
23. OSullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000;2:85-92.
24. Tolstunov L. Implant zones of the jaws: implant location and related success rate. J Oral Implantol. 2007;33:211‑20.
25. Sesma N, Pannuti C, Cardaropoli G. Retrospective clinical study of 988 dual acid‑ etched implants placed in grafted and native bone for single‑ tooth replacement. Int J Oral Maxillofac Implants 2012;27:1243‑8.
26. Makary C, Menhall A, Zammarie C, Lombardi T, Lee S, Stacchi C, Park K. Primary Stability Optimization by Using Fixtures with Different Thread Depth According To Bone Density: A Clinical Prospective Study on Early Loaded Implants. Materials. 2019;12:2398.
27. Barikani H, Rashtak S, Akbari S, Badri S, Daneshparvar N, Rokn A. The effect of implant length and diameter on the primary stability in different bone types. J Dent. 2013;10:449‑55.
28. Gehrke S, da Silva U, Del Fabbro M. Does Implant Design Affect Implant Primary Stability? A Resonance Frequency Analysis‑Based Randomized Split‑Mouth Clinical Trial. J Oral Implantol. 2015; 41: 281‑6.
�
Andre Moreira
E-mail address: andregonmoreira@gmail.com
