
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2020 | 61 (1) | 2-9
Original research
The influence of pre-surgical orthodontic treatment on the dento-skeletal profile of Class III patients
A influência do tratamento ortodôntico pré-cirúrgico no perfil dento-esquelético de indivíduos com Classe III
a Faculdade de Medicina Dentária, Universidade de Lisboa, Portugal
Natascha Fernandes - natascha_sf@yahoo.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 61
Issue - 1
Original research
Pages - 2-9
Go to Volume
Article History
Received on 16/12/2019
Accepted on 24/03/2020
Available Online on 02/07/2020
Keywords
Original research
�
The influence of pre-surgical orthodontic treatment on the dento-skeletal profile of Class III patients
A influ�ncia do tratamento ortod�ntico pr�-cir�rgico no perfil dento-esquel�tico de indiv�duos com Classe III
�
Natascha Fernandes*, Joana Godinho, Luis Jardim
Faculdade de Medicina Dent�ria, Universidade de Lisboa, Portugal
�
�
http://doi.org/10.24873/j.rpemd.2020.07.696
�
Abstract
Objectives: This cephalometric study intended to evaluate pre-surgical changes in cephalometric variables on the lower third of the face produced by the orthodontic treatment, in patients with severe Class III malocclusions.
Methods: The sample included 40 adults, divided into three groups: no-extractions (N), extractions for orthodontic reasons (E), and previous extractions for non-orthodontic reasons (E-NO). Student t-tests were used to evaluate the influence of orthodontic treatment on the cephalometric variables. An ANOVA was used for group comparisons before treatment and to compare the changes produced by the orthodontic treatment in the three groups. The significance level was established at 5%.
Results: In Group E, significant (p<0.05) retraction andretroclination of the upper incisors were observed. The lower incisors proclined in all the three groups and protracted in Groups N and E-NO. The upper incisor remained proclined in Group N, and the lower incisor retroclined in Group E-NO. There was a clockwise rotation of the mandible, with an increase in total and inferior facial heights, in both the extraction groups. The upper molars advanced in all groups.
Conclusions: 1) The SNA angle decreased due to point A retraction in Group E. 2) Mandibular clockwise rotation led to increased total and inferior facial heights, in both the extraction groups. 3) Extractions facilitated incisor decompensation in Group E. 4) After treatment, the lower incisors remainedretroclined in Group E-NO, due to an exaggerated initialretroclination.
Keywords: Class III malocclusion, Cephalometrics, Pre-surgical orthodontic treatment
�
Resumo
Objetivos: Este estudocefalom�trico pretendeu avaliar as altera��es produzidas pelo tratamento ortod�ntico pr�-cir�rgico sobre as vari�veis cefalom�tricas dento-esquel�ticas do ter�o inferior da face, em pacientes com maloclus�es severas de Classe III.
M�todos: A amostra, constitu�da por 40 adultos, foi dividida em tr�s grupos: sem extrac��es (N); extra��es por raz�es ortod�nticas (E); dentes previamente extra�dos por raz�es n�o ortod�nticas (E-NO). A influ�ncia do tratamento ortod�ntico sobre as medi��es, bem como as diferen�as iniciais entre grupos, foram determinadas utilizando testes t de Student. Para efetuar a compara��o entre os tr�s grupos, foi utilizada uma an�lise ANOVA. O n�vel de signific�ncia estat�stica foi estabelecido em 5%.
Resultados: No Grupo E, os incisivos superiores foram significativamente (p<0,05) retra�dos eretro-inclinados. Verificou-se uma proinclina��o do incisivo inferior nos tr�s grupos e ainda um avan�o nos grupos N e E-NO. O incisivo superior permaneceu proinclinado no Grupo N e o incisivo inferior continuou retro-inclinado no Grupo E-NO. Foi observada uma rota��o hor�ria da mand�bula, com aumento da altura facial total e inferior, nos grupos E e E-NO. O molar superior mesializou nos tr�s grupos.
Conclus�es: 1) O �ngulo SNA diminuiu no Grupo E � custa daretra��o do ponto A. 2) Observou-se uma rota��o hor�ria da mand�bula com aumento da altura facial total e inferior nos grupos comextra��es. 3) As extra��es permitiram uma maior descompensa��o dos incisivos no Grupo E. 4) No Grupo E-NO, os incisivos inferiores continuaram retro-inclinados depois do tratamento, uma vez que a retro-inclina��o inicial era excessiva.
Palavras-chave: M� oclus�o de Classe III, Cefalometria, Tratamentoortod�ntico pr�-cir�rgico
�
Introduction
A large percentage of individuals seeking a combined orthodontic/orthognathic surgery intervention have skeletal Class III malocclusions. 1 This sagittal discrepancy is characterized by maxillary deficiency, mandibular excess or a combination of both.1, 2 Changes in vertical facial growth can further contribute to the complexity of these cases.3 - 7
There are several treatment options for Class III malocclusions.
Dentofacial orthopedic appliances8 - 10 and devices for protraction with bone anchorage11, 12 can improve the growth pattern in children with a genetic predisposition for this problem.
Purely orthodontic dentoalveolar compensation can be attempted to camouflage the skeletal discrepancy in adults when an aesthetically acceptable profile accompanies a mild-to-moderate skeletal Class III malocclusion.13 - 16
Excessive retroclination of the lower incisors during camouflage treatments can lead to an exaggeratedbuccal prominence of their roots and gingival recession.14 In such cases, a combined surgical orthodontic treatment, rather than camouflage, would be the correct approach.14 Additional guidelines for surgical orthodontic treatment in adult patients are ANB and lower incisor-mandibular plane angles smaller than -4o and 83o, respectively.17 Other important factors that distinguish surgical from non-surgical patients are the ratio between maxillary and mandibular length, the gonial angle, the sella-nasion distance and the Wits appraisal.16 - 19
The main objectives of orthognathic surgery are the development of a functional and stable occlusion and an improvement in facial aesthetics.15, 20 - 25 In this type of treatment, a pre-surgical orthodontics phase is usually followed by the surgical correction of the skeletal discrepancy. Then, a post-surgical orthodontic period is required to finish and detail the occlusion.26
Dento-alveolar compensations in the form of upper incisor proclination and lower incisorretroclination help to maintain function and camouflage an existing Class III skeletal discrepancy.4, 15, 27, 28 In patients with larger anteroposterior discrepancies and increased mandibular posterior rotation, the compensatory lower incisor retroclination is increased.13, 28
Additionally, in hyperdivergent patients, the lower incisors erupt in a way that maintains the overbite, and the alveolar bone becomes longer and thinner in the labio-lingual direction.
These features may increase the risk of periodontal problems in the anteroinferior region.27, 29, 30 Pre-surgical orthodontics eliminates these compensations by creating or increasing a reverse overjet, which allows a surgical mandibular setback and/or maxillary advancement. As a result, the direction of the incisor movement is opposite to that required by a non-surgical, compensatory treatment plan. Therefore, comparing to the baseline, the patient�s malocclusion and profile are generally worse immediately before surgery, and this can only be avoided if an early surgical approach is used.15, 31, 32
Depending on the magnitude of the initial sagittal discrepancy and the degree of incisor compensation observed, an orthodontic treatment plan is established. This treatment may require the extraction of upper first premolars, alone or in combination with the lower second premolars.
The aim of this retrospectivecephalometric study was to evaluate the changes produced by pre-surgical orthodontic treatment on dental and skeletal measurements of the lower third of the face, in patients with skeletal Class III malocclusions requiring orthognathic surgery, using different extraction protocols. The null hypothesis tested was that, after the pre-surgical orthodontic phase, no differences would be found in cephalometric measurements between the extractions (for orthodontic and non-orthodontic reasons) and the no-extractions groups.
Material and methods
The sample for this study consisted of adult orthodontic patients with skeletal Class III malocclusions requiring orthognathic surgery. The inclusion criteria were European origin, no previous orthodontic or orthopedic treatments, good quality cephalometric x-rays, and treatment performed by the same specialist in orthodontics. After approval by the Ethics Committee of the School of Dentistry of the University of Lisbon, a sample of 18 males and 22 females was gathered, with informed consent. Individuals with congenital anomalies and severe facial asymmetries were excluded from the study.
The original sample was divided into three groups: Group N, including no extractions (n =13); Group E, including upper first premolars extracted for orthodontic treatment purposes (n =12); and Group E-NO, including previous extractions for non-orthodontic reasons (n =15).
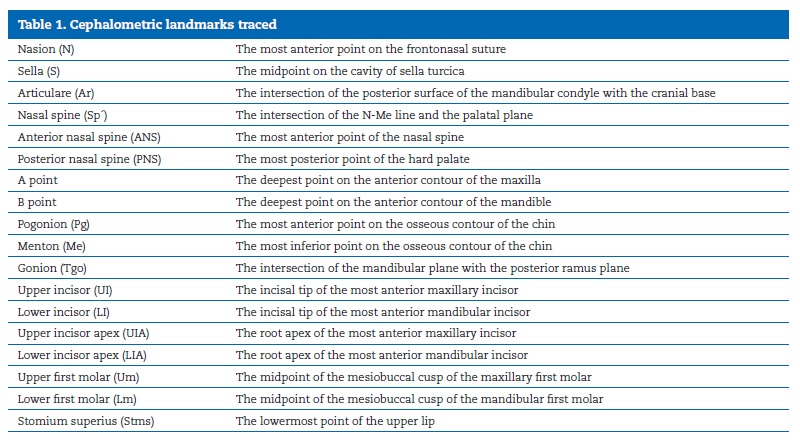
Lateral cephalograms were taken before (T1) and after (T2) the pre-surgical orthodontic treatment phase with the aid of a cephalostat and with the Frankfurt horizontal plane parallel to the floor. The Adobe Photoshop CS5 (Adobe Inc.� San Jos�, California) program was used to superimpose the T2 cephalogra on the T1 one, according to the structural method of Bj�rk. The horizontal reference plane (x) was constructed 7� above the sella-nasion line, with the vertex at nasion.33 A line perpendicular to the horizontal plane at nasion was used as the vertical reference plane (y). All linear cephalometric variables were measured either parallel or perpendicular to the x plane, using the cephalometric program Nemoceph (Nemotec �, Madrid, Spain). The cephalometric landmarks used are described in Table 1. The palatal plane (ANS-PNS), the mandibular plane (Tgo-Me), the long axis of the upper incisor UI1 (UIUIA) and the long axis of the lower incisor LI1 (LI-LIA) were also traced in the analysis.
�
�
Cephalometric measurements were chosen to represent skeletal and dental variables, which could be changed by the pre-surgical orthodontic treatment. For skeletal changes, the SNA angle, total facial height (TFH, N-Me distance), inferior facial height (IFH, Sp�-Me distance), maxillary prominence (point A to y distance), mandibular prominence (point B to y distance), chin prominence (Pg to y plane) and the MP-x angle (Tgo-Me to x plane) were calculated. For dental changes, the following measurements were evaluated: upper incisor exposure (UI-Stms distance),overjet, overbite, UI-y distance, LI-y distance, UI-PP distance, LI-MP distance, UI1-x angle, LI1-x angle, UI1-PP angle, LI1-MP angle, Um-y distance, Lm-y distance, Um-PP distance, and Lm-MP distance.
One researcher traced all the radiographs and was blinded for patients� identity, to avoid bias. Ten randomly chosen cases were re-traced within a month interval, by the same investigator.
Method error was evaluated with paired t-tests and the Dahlberg�s equation: √Σd2/2n, where d is the difference between the calculated values between the first and the second tracings.34
Statistical analysis was done with SPSS� version 20.0 for Macintosh (IBM Company, Armonk, NY, USA). Descriptive statistics (mean and standard deviation) were calculated at T1 and T2 for each cephalometric variable. The Shapiro-Wilk test was performed to evaluate normality in the sample distribution.
A t-test for independent samples was used to determine the influence of the orthodontic treatment on the cephalometric variables within each group. Differences between the groups before treatment and differences in the changes produced by the orthodontic treatment in the three groups were evaluated using an ANOVA analysis. Post-hoc testing was done with the Bonferroni method. The level of statistical significance was fixed at 5%.
For the method error, the paired t-test revealed no significant differences between the first and the second measurements (p>0.05). No systematic deviations were found, and the values obtained from the Dahlberg equation were generally small (<1�/1mm). Therefore, there were no significant random errors.
Results
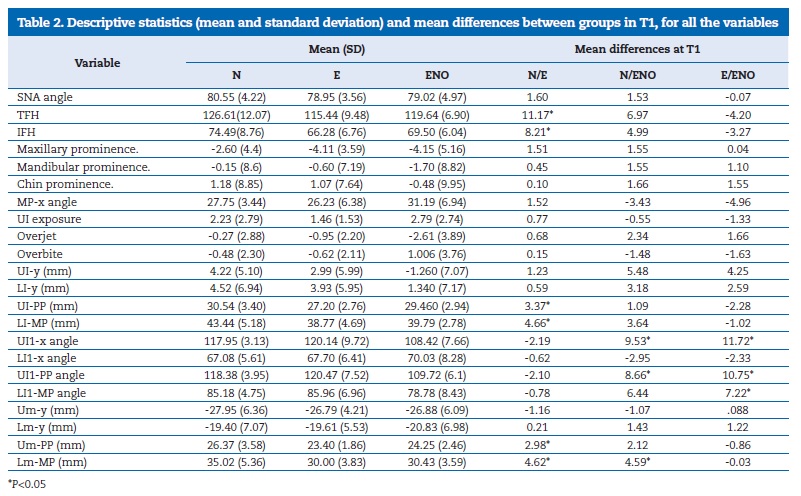
According to the results of the Shapiro-Wilk test, all variables in the study showed normal distribution. The descriptive statistics (mean and standard deviation) before the orthodontic treatment (T1) are presented in Table 2.
�
�
The differences between Groups N, E and E-NO before the pre-surgical orthodontic treatment (T1) are exposed in Table 2. In comparison with Group N, Group E was characterized by a decrease in TFH and IFH. The distances UI-PP, Um-PP, LI-MP and Lm-MP were also reduced. The distance Lm-MP was smaller in Group E-NO than in Group N. Upper incisor inclination in relation to both the palatal plane and the horizontal plane was reduced in Group E-NO in comparison with the other two groups. The lower incisorretroclination was significantly (p<0.05) greater in Group E-NO than in Group E.
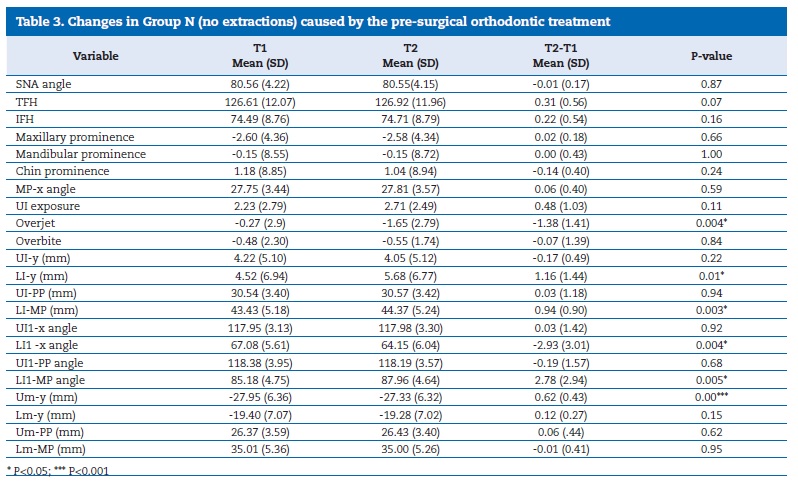
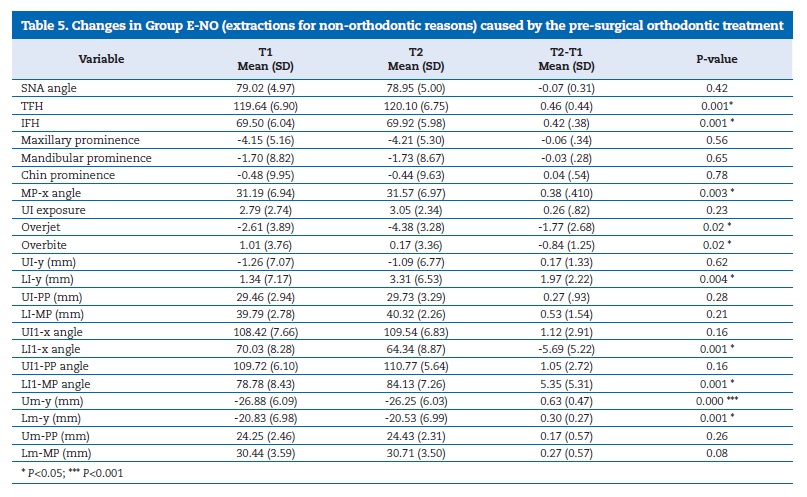
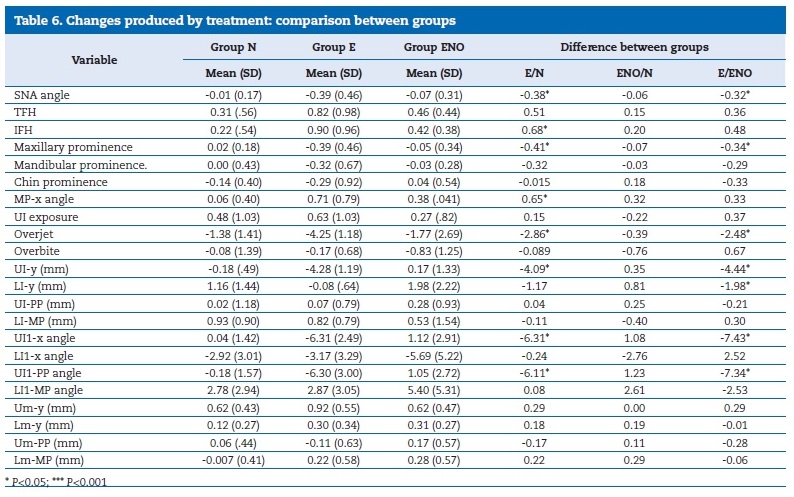
Changes produced by the orthodontic treatment are presented in Table 3 for Group N, Table IV for Group E and Table V for Group E-NO. In Group N, the overjet became more negative due to lower incisor proclination and protraction, and the distance between this incisor and the mandibular plane increased. The upper molars moved forward in Group N.
�
�
�
�
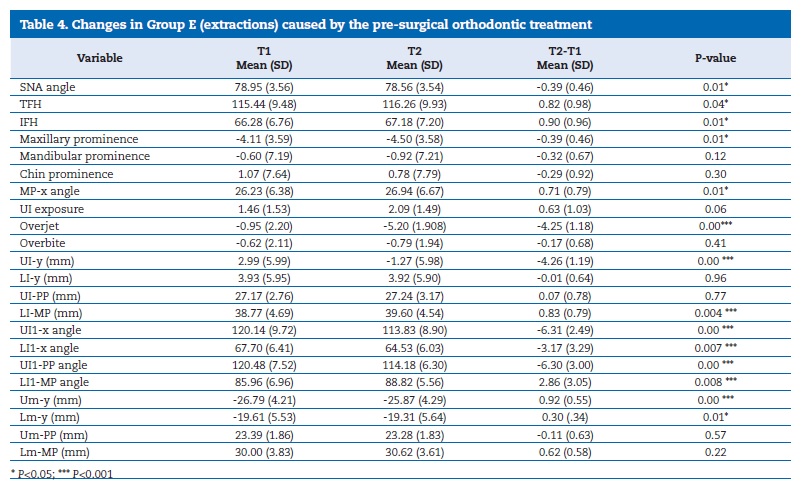
In Group E, the SNA angle decreased, and point A retraction was observed. Posterior mandibular rotation caused an increase in TFH and IFH and in the MP-x angle (Table 4). Theoverjet became more negative due to the elimination of dental compensations: the upper incisors were retracted and retroclined, and the lower incisors were proclined and extruded.
Both upper and lower molars moved forward in Group E. An increase in TFH and IFH and the MP-x angle were observed in Group E-NO (Table 5). The overjet became more negative and the overbite decreased with lower incisorsproclination and protraction, and both upper and lower molars mesialized in Group E-NO.
The comparisons between groups during the pre-surgical orthodontic treatment are presented in Table 6. There was a larger decrease in the SNA angle and a greater retraction of point A in Group E when compared to Group N. Mandibular posterior rotation was also greater in Group E with a higher increase in the IFH and the MP-x angle.Overjet became more negative in Group E than in Group N, due to a greater retraction and retroclination of the upper incisors.
�
�
When comparing Group E to Group E-NO, a significant (p<0.05) decrease in the SNA angle and a larger retraction of point A were observed in the first. Overjet also became more negative, primarily due to a larger retraction and retroclination of the upper incisors. In Group E�NO, greater lower incisor advancement was observed in relation to the vertical plane.
There were no significant (p>0.05) differences in the changes observed between Groups N and E-NO (Table 6).
Discussion
Pre-surgical orthodontic treatment involves leveling and aligning of the dental arches, transverse coordination, closure of extraction spaces, and elimination of dental compensations.26 Although the orthodontic treatment might involve extractions, some Class III surgical patients already have missing teeth for non-orthodontic reasons. Since this could influence the cephalometric variables measured in the present study, the patients were divided into three groups (N, E and E-NO).
Before treatment, the magnitude of the sagittal discrepancy was similar in all groups. The increased upper incisorproclination initially observed in Group E may have contributed to the decision to extract teeth in these cases. In Group E-NO, the normal upper incisor inclination could be explained by the previous absence of posterior teeth. This arch length collapse could also have been responsible for the greater retroclination observed in the lower incisors of this group. However, some degree of lower incisorretroclination was present in all groups before treatment.
During the pre-surgical orthodontic treatment, all three groups exhibited anchorage loss with mesialization of the upper first molars. In Groups E and E-NO, lower molar advancement also occurred, possibly due to closure of the extraction spaces. Although Group E initially demonstrated greater upper incisor proclination, the treatment caused significant upper incisor retraction and retroclination only in this group, resulting in an overjet more negative than in the other two groups.
Alveolar bone resorption on the labial aspect of the retracted incisors caused a significant point A retraction and a reduction in the SNA angle.
According to other authors, orthodontic treatment planning without extractions in the upper arch may limit upper incisor retraction and may be responsible for the persisting post-treatment incisor proclination.15, 35 This situation was verified in Group N in the present study, where the upper incisors remained proclined. In Group E-NO, these teeth maintained a normal inclination even before surgery. Generally, satisfactory results depend on an adequate correction of upper incisor proclination as successful decompensation permits greater surgical movement.35, 36
The lower incisors proclined in all groups and advanced in Groups N and E-NO. The success in lower incisordecompensation was verified by other authors.36 However, the greater initial lower incisor retroclination in Group E-NO, caused by the absence of several posterior teeth, limited the amount of proclination achieved orthodontically and, thus these teeth were still excessively retroclined post-treatment comparing to the norm. 38 This association between unsuccessful lower incisor decompensation and extractions in the lower arch has been previously documented.35 Persisting lower incisor retroclination can limit correction and lead to reduced ANB and excessive SNB angles even after treatment.35
Although decompensation has been described to be less successful in hyperdivergent and severe anteroposterior discrepancies,37 the groups were similar initially. Factors that contribute to insufficient lower incisor decompensation include lower arch extractions, severe initial lower incisorretroclination, lack of patient cooperation in the use of Class II elastics, and insufficient alveolar bone thickness to permit incisor advancement.35
One of the limitations of this investigation was the small sample size in each group since the 40 patients were subdivided into three groups. Also, Group E-NO was heterogeneous and included patients that had three or more missing teeth anterior to the upper and lower first molars.
Future studies on the long-term impact of removing dental compensations on surgical cases with and without extractions are needed. Finally, the effects of pre-surgical incisor decompensation on the soft tissues, which, although temporary, can have a strong impact on facial aesthetics, should be investigated.
Conclusions
1) In Group E, there was a decrease in the SNA angle due to retraction of point A.
2) Mandibular clockwise rotation in Groups E and E-NO led to an increase in total and inferior facial heights.
3) Upper incisors were significantly retracted andretroclined only in Group E, where extractions facilitated incisor decompensation.
4) The lower incisor was proclined in all three groups and protracted in Groups N and E-NO. Due to the large degree of initial retroclination, the lower incisors remained retroclined in Group E-NO after treatment.
5) The upper first molar advanced in all the three groups.
�
References
1. Proffit WR, Philips C,Dann C. Who seeks surgical orthodontic treatment?Int J Adult Orthog Surg. 1990;5:153-60.
2. Staudt CB,Kiliaridis S. Different skeletal types underlying Class III malocclusion in a random population. Am J Orthod Dentofac Orthop. 2009;136:715-21.
3. Bell WH, White RP, Proffit WR. Surgical correction of dentofacial deformities, Volume I. Philadelphia: WB Saunders; 1980.
4. Jacobson A, Evans WG, Preston CB,Sadowsky PL. Mandibular prognathism. Am J Orthod. 1974;66:140-71.
5. Nojima K, Nagai H, Nishii Y, Sakamoto T, Yamaguchi H. Morphological evaluations in skeletal Class III malocclusion requiring maxillofacial surgery using orthognatic surgical analysis. Bull. Tokyo Dent Coll. 2002;43:163-71.
6. Proffit WR, White RP, Sarver DM. Contemporary treatment of dentofacial deformity. St Louis: Mosby;2003.
7. Sanborn RT. Differences between the facial skeletal patterns of Class III malocclusion and normal occlusion. Angle Orthod. 1955;25:208-22.
8. Arman A,Toygar TU, Abuhijleh E. Profile changes associated with different orthopedic treatment approaches in Class III malocclusions. Angle Orthod. 2004;74:733-40.
9. Franchi L,Bacetti T, Tollaro I. Predictive variables for the outcome of early functional treatment of Class III malocclusion. Am J Orthod Dentofac Orthop. 1997;112:80-6.
10. Kilic N,Catal G, Kiki A, Oktay H. Soft tissue profile changes following maxillary protraction in Class III subjects.Eur J Orthod. 2010;32:419-24.
11. Bacceti T, DeClerck HJ, Cevidanes LH,Franchi L. Morphometric analysis of treatment effects ofboneanchored maxillary protraction in growing Class III patients. Eur JOrthod. 2011;33:121-5.
12. Cevidanes L,Baccetti T, Franchi L, McNamara A, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus face mask with rapid maxillary expansion. Angle Orthod. 2010;80:799-806.
13. Ishikawa H, Nakamura S, Iwasaki H, Kitazawa S,Tsukada H, Chu S. Dentoalveolar compensation in negative overjet cases. Angle Orthod. 2000;70:145-8.
14. Sperry TP, Speidel TM, Isaacson RJ, Worms FW. The role of dental compensations in the orthodontic treatment of mandibular prognatism. Angle Orthod. 1977;47:293-9.
15. Troy B, Shanker S, Fields HW, Vig K, Johnston W. Comparison of incisor inclination in patients with Class III malocclusion treated withorthognathic surgery or orthodontic camouflage. Am J Orthod Dentofac Orthop. 2009;135:146.e1-9.
16. Tseng YC, Pan CY, Chou ST, Liao CY, Lai ST, Chen CM et al. Treatment of adult Class III malocclusions with orthodontic therapy or orthognathic surgery: Receiver operating characteristic analysis. Am J OrthodDentofac Orthop. 2011;139:485-93.
17. Kerr WJS, Miller S,Dawber JE. Class III malocclusion: surgery or orthodontics? Br J Orthod. 1992;19:21-4.
18. Murakami C, Hiyama S,Ohyama K. Craniofacial morphology of skeletal Class III patients before treatment and growthrelated changes during treatment with a maxillary protraction appliance: a comparison of orthodontic and surgical cases. World J Orthod. 2005;6:51-60.
19. Stellzig-Eisenhauer A, Lux CJ, Schuster G. Treatment decision in adult patients with Class III malocclusion: orthodontic therapy or orthognathic surgery? Am J OrthodDentofac Orthop. 2002;122:27-37.
20. Chew MT, Sandham A, Wong HB. Outcome of orthognathic surgery in Chinese patients.A subjective and objective evaluation. Angle Orthod. 2007;77:845-50.
21. Bell R, Kiyak HA,Joondeph DR, McNeill RW, Wallen TR. Perceptions of facial profile and their incluence on the decision to undergo orthognathic surgery. Am J Orthod. 1985;88:323-32.
22. Jacobson A. Psychological aspects ofdentofacial esthetics and orthognathic surgery. AngleOrthod. 1984;4:18-35.
23. Kiyak H, West R,Hohl T, McNeil R. The psychological impact oforthognathic surgery: a 9 month follow up. Am J Orthod. 1982;81:404-12.
24. Laufer D, Glick D,Gutman D, Sharon A. Patient motivation and response to surgical correction of prognathism. Oral surg, Oral Med, OralPathol. 1976;41:309-13.
25. Rivera SM, Hatch JP, Dolce C, Bays RA, VanSickels JE, Rugh JD. Patients own reasons and patient-perceived recommendations for orthognathic surgery. Am J OrthodDentofacial Orthop. 2000;118:134-40.
26. Edler RJ. Problems in the orthodontic management of orthognathic cases. Eur J Orthod. 1990;12:420-37.
27. Ahn HW,Baek SH. Skeletal anteroposterior discrepancy and vertical type effects on lower incisor preoperativedecompensation and postoperative compensation in skeletal Class III patients. Angle Orthod. 2011;81:64-74.
28. Lin J, Gu Y. Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition. AngleOrthod. 2003;73:401-10.
29. Chung CJ, Jung S, Baik HS. Morphological characteristics of the symphyseal region in adult skeletal Class IIIcrossbite and openbite malocclusions. Angle Orthod. 2008;78:38-43.
30. Handelman CS. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:5-109.
31. Worms FW, Isaacson RJ, Spiedel TM. Surgical orthodontic treatment planning: profile analysis and mandibular surgery. Angle Orthod. 1976;46:1-25.
32. Huang CS1, Hsu SS, Chen YR. Systematic review of the surgery-first approach in orthognathic surgery. Biomed J. 2014;37:184-90.
33. Legan HL,Burstone CJ. Soft tissuecephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38:744-51.
34. Houston W. The analysis of errors in orthodontic measurements. Am JOrthod. 1983;83:382-90.
35. Johnston C, Burden D, Kennedy D, Harradine N, Stevenson M. Class III surgical-orthodontic treatment: a cephalometric study. Am J OrthodDentofac Orthop. 2006;130:300-9.
36.Capelozza Filho L, Martins A, Mazzotini R, Da Silva Filho OG. Effects of dental decompensation on the surgical treatment of mandibular prognathism. Int J AdultOrthodon Orthognath Surg. 1996;11:165-80.
37. Phonpraserth A, Cunningham SJ, Hunt NP. Soft tissue changes associated with incisordecompensation prior to orthognathic surgery. Int J Adult Orthod Orthognath Surg. 1999;14:199-206.
38. Tweed CH. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am J Orthod Oral Surg. 1946;32:175-230.
�
Natascha Fernandes
E-mail address: natascha_sf@yahoo.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 16 December 2019
Accepted 24 March 2020
Available online 2 July 2020
