
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2019 | 60 (4) | 175-188
Clinical innovation
A comprehensive classification to full arch implant rehabilitation
Uma classificação abrangente para reabilitação total sobre implantes
a Oral Surgery and Implant Department, Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b LIBPhys-FCT UID/FIS/04559/2013, Lisboa
c International Director New York University College of Dentistry Linhart Continuing Dental Education Program, New York,USA
d Implantology Institute, Lisbon, Portugal
João Caramês - caramesj@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 4
Clinical innovation
Pages - 175-188
Go to Volume
Article History
Received on 11/10/2019
Accepted on 08/11/2019
Available Online on 19/12/2019
Keywords
Clinical innovation
�
A comprehensive classification to full arch implant Rehabilitation
Uma classifica��o abrangente para reabilita��o total sobre implantes
�
Jo�o Caram�s*
Oral Surgery and Implant Department, Faculdade de Medicina Dentaria, Universidade de Lisboa, Lisbon, Portugal
LIBPhys-FCT UID/FIS/04559/2013, Lisboa
International Director New York University College of Dentistry Linhart Continuing Dental Education Program, New York, USA
Implantology Institute, Lisbon, Portugal
�
�
http://doi.org/10.24873/j.rpemd.2019.12.687
�
Abstract
Objectives: This article proposes a classification system for full-arch implant rehabilitation options, taking into account the patient's individual bone resorption pattern.
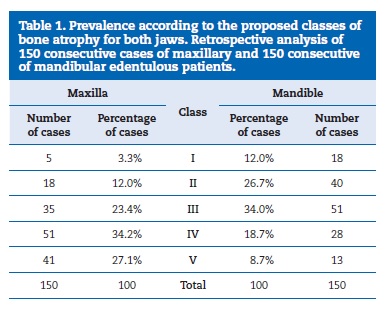
Methods: Five levels of jaw atrophy were established according to the available therapeutic bone height and width in the anterior and posterior jaw, based on the evaluation of 150 consecutive edentulous maxillae and 150 consecutive edentulous mandibles by cone-beam computed tomography.
Classification proposal: Fixed full-arch and removable rehabilitation schemes were proposed for each level. Implant number, location, position, design and the need for regenerative procedures were defined according to clinical information and available evidence-based rationale
Conclusions: The illustrated rehabilitation scheme aims to aid clinicians during treatment
planning and to underline a pyramidal complexity hierarchy of the different classes, from simple to complex. Besides being helpful for treatment planning, this classification also optimizes communication between clinicians and patients.
Keywords: Classification, Clinical assessment, Diagnosis, Full-arch rehabilitation, Patient-centered outcomes
�
Resumo
Objetivos: Este artigo prop�e um sistema de classifica��o das op��es de reabilita��o total sobre implantes, tendo em conta o padr�o de reabsor��o osseo individual do doente.
M�todos: Roman;mso-bidi-font-family: CaeciliaLTStd-Roman'>Atrav�s da analise e avalia��o radiogr�fica (Cone Beam Computed Tomography) de 150 maxilas e 150 mandibulas edentulas de forma consecutiva, foram descritos cinco n�veis de atrofia dos maxilares de acordo com a disponibilidade �ssea a n�vel de altura e largura nas regi�es anteriores e posteriores. Proposta de classifica��o: Foram propostos esquemas de reabilita��o fixa e de reabilita��o remov�vel para cada n�vel. De acordo com a informa��o clinica e a evidencia cient�fica dispon�vel foram definidos os seguintes par�metros: numero, localiza��o, posi��o e desenho dos implantes e a necessidade de procedimentos regenerativos.
Conclus�es: Roman;mso-bidi-font-family: CaeciliaLTStd-Roman'>Os esquemas de reabilita��o ilustrados tem como prop�sito auxiliar os cl�nicos durante o planeamento baseando-se numa pir�mide hier�rquica das diferentes classes, do mais simples ao mais complexo. Al�m da sua utilidade, esta classifica��o tamb�m visa otimizar a comunica��o entre cl�nicos e pacientes.
Palavras-chave: Classifica��o,Avalia��o clinica,Diagnostico,Reabilita��o total,Resultados centrados no paciente
�
Introduction
Complete edentulism is still a global health problem. Available data collected worldwide report a wide variation of the prevalence of edentulism, equating up to 70% in population groups aged 60 years old or over.1 Some epidemiological studies highlight a decrease in prevalence in developed countries due to preventive oral health measures.2 However, the increase in life expectancy seems to balance this tendency and promote the need for treatment.3
An implant-supported full-arch rehabilitation, either fixed or removable, represents a highly predictable treatment for edentulous patients to recover masticatory function, aesthetics and psychological well-being.4, 5 Patient-related outcome measures evaluated through oral health-related quality of life (OHRQol) parameters, patient satisfaction and patient preference, serve to confirm these prosthodontic needs.6, 7 Several prospective studies8 - 12 and, recently, randomized clinical trials13, 14 and systematic reviews, 15 after evaluation at the implant and prosthesis levels, have described high survival and success rates associated with these types of rehabilitations either in immediate, early or conventional loading protocols.
From the clinician�s perspective and according to the SAC Classification proposed by ITI, surgical and prosthodontic considerations for a fixed full-arch rehabilitation fall within Advanced and Complex procedures.16 Several factors determine these levels of difficulty. A variable bone resorption pattern associated with different levels of atrophy, the proximity to anatomical landmarks or patient risk factors require accurate planning and a highly skilled surgeon.17 Several classical anatomical classifications have been proposed to help diagnose resorption patterns in edentulous jaws.17 - 19 Although those classifications express the type and profile of the alveolar ridge in different levels of atrophy, they do not suggest any prosthodontic rehatbilitation options for each level.
Some classification systems have been proposed to guide clinicians and provide a basis for diagnostic and treatment procedures for full-arch implant rehabilitations and simplify communication between patients, colleagues and technicians.20, 21
However, there is still a need for a classification system that simultaneously takes into consideration the jaw anatomy and resorption pattern, the implant placement site, the surgical technique and the prosthodontic rehabilitation scheme.22, 23
The classification system proposed in this manuscript considers the patient�s clinical information as the cornerstone of the therapeutic decision-making process. Medical factors, expectations, biomechanics and prosthodontic design should be the primary starting point from which this process begins. This unique information is crucial for adjusting and optimizing the implant-prosthodontic scheme decision. The classification system proposed follows this principle and is the result of twenty-four years of clinical experience in full-arch implant surgery and prosthodontics by the author. This period was characterized by more than 3500 edentulous arches rehabilitated at the author�s clinical center. To complement this specialist proposal and provide clinicians with predictable clinical options for each category from Maxilla and Mandible Class I to Class V, this tool for aiding decisions also integrates the best available evidence to support the prosthodontic options suggested for each class.
Classification Proposal
A complete anamnesis should collect and emphasize patient-related factors. General systemic health, soft-tissue conditions, type of the opposing jaw, oral hygiene, parafunctional habits (bruxism and clenching), patient expectations and financial situation represent some of the deciding factors that justify the therapeutic options proposed for each class.
Based on a prosthodontic-driven implant placement approach, a properly designed prosthesis should always be obtained prior to the surgical appointment. The aesthetic analysis should be ruled by facial, dentolabial and tooth-related factors.24
Aspects such as vertical occlusal dimension assessment, appropriate upper lip support, smile line and phonetics should be integrated into a mutually protected occlusion in fixed full-arch prostheses or a bilateral balanced occlusion in overdentures.
The current tendency toward minimally invasive surgical procedures, thus decreasing patient morbidity, has been taken into account, since graftless full-arch implant rehabilitation is proposed in each class whenever possible.7 In cases of severe bone resorption, compromised lip support or local bone defects, horizontal or vertical bone augmentation are proposed to provide a more predictable treatment option.25
Similarly, and aiming for higher patient satisfaction, an immediate loading protocol should be applied in Carames Classification (CC) classes where an implant primary stability > 30 N.cm should be obtained.5, 26, 27 In compromised patients, particularly in the maxilla, with one or more risk factors such as smoking, diabetes, bruxism, periodontal disease or severe bone atrophy, a conventional loading protocol is preferred.28
Preoperative cross-sectional image acquisition of the edentulous arch anatomy and implant site should be obtained using a cone-beam computed tomography (CBCT) scan. This prerequisite is in accordance with the EAO guidelines for the use of diagnostic imaging in Implant Dentistry and the 5threcommendation of the American Academy of Oral and Maxillofacial Radiology�s position statement on selection criteria for the use of radiology in Implant Dentistry.29, 30
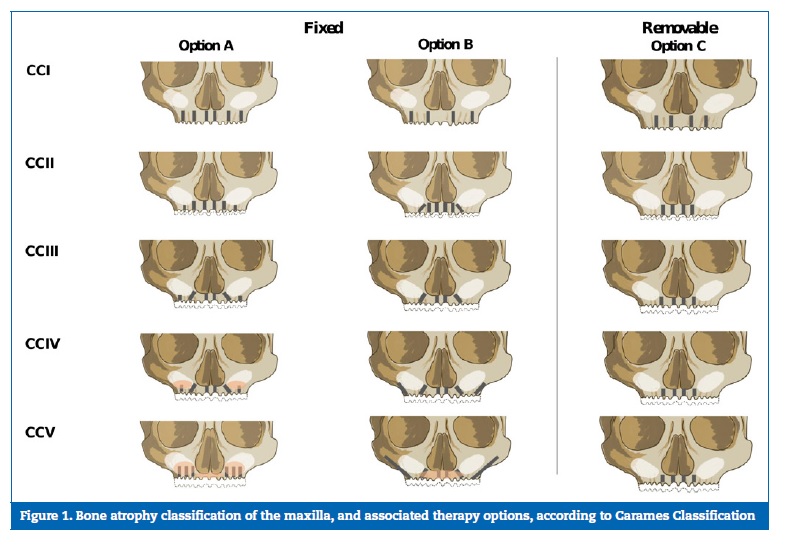
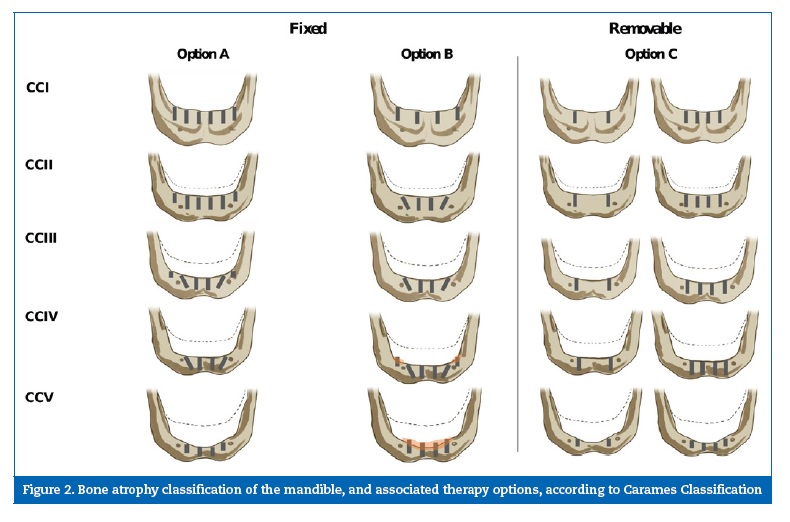
The five classes (CCI-CCV) proposed for each edentulous jaw express the different levels of bone atrophy and therapeutic bone height and width most usually found among edentulous patients. Two fixed (Options A and B) and one removable (Option C) full-arch schemes, taking into consideration implant number, distribution, position and eventual grafting procedures, are proposed for each Maxilla (Figure 1) and Mandible (Figure 2) CC Class. The three rehabilitation options proposed are merely indicative and equally valid. Deciding factors complement the possible reasons for the treatment choice within each CC Class.
�
�
�
Either four, six or eight implants are proposed for fixed full-arch rehabilitation and a minimum of two and a maximum of four implants are considered for removable full-arch rehabilitation. Odd numbers of implants are avoided and only used in compromised clinical situations. The illustrated schemes are based on a symmetric and homogenous resorption pattern of the maxilla and mandible. In cases where an asymmetric resorption pattern is observed, left and right sides should be classified independently.
Anatomical classification measurements
The planning guidelines of this system consider a standard 4.1-mm diameter implant, but, in compromised cases, smaller or wider diameter implants can be used. In order to avoid facial bone resorption and soft-tissue recession, implant positioning should ensure, whenever possible, a critical buccal plate width equivalent to 2 mm.31, 32 Thus, the minimum width when placing a standard implant is 6 mm or more.
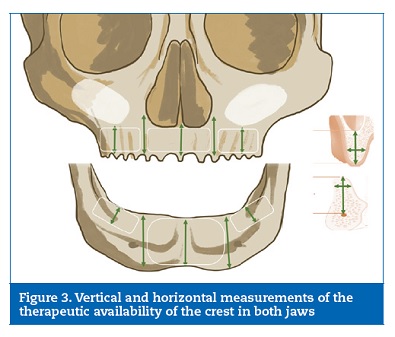
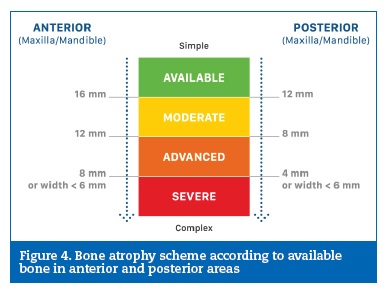
Atrophic ridges frequently have a narrow and knife-edge shape. For treatment planning, the therapeutic availability of the crest is vertically and horizontally measured in millimeters (mm) by a built-in digital ruler in the CBCT software (Figure 3). The vertical measurement only considers the most coronal part of the crest with a >6-mm width. Depending on the vertical and horizontal level of atrophy, we can consider that the crest either has available bone or moderate, advanced or severe bone resorption (Figure 4).
�
�
�
In the maxillae, the measurements are made in five positions: in the anterior region, at the midline and at the point of confluence between the anterior wall of the sinus and the nasal cavity on each side. The height is measured from the >6-mm width crestal level to the inferior border of the nasal cavity or the point of confluence between the anterior wall of the sinus and the nasal cavity. In the posterior region, the first molar position is considered. The height is measured from the > 6-mm width level of the alveolar ridge to the inferior wall of the maxillary sinus.
In the mandible, the measurements are also made in five positions: in the anterior region, at the midline and on each side of the mandible at 4 mm anterior to the position of the mental foramen. The height is measured from the >6-mm width crestal level to the inferior border of the mandible. In the posterior region, the first molar position is considered. The posterior therapeutic bone height is measured as the distance from the >6-mm width bone crest level to a 2-mm safe distance to the mandibular canal.
The therapeutic height and width values suggested for each CC class are based on experience and the result of a consecutive preoperative CBCT analysis of 150 edentulous maxillae and 150 edentulous mandibles performed by the author (Table 1).
�
�
Carames Classification (CC) classes description, therapeutic options and deciding factors
Maxilla CC I
Anterior � Available bone (height >16 mm; width >6 mm)
Posterior � Available bone (height >12 mm; width >6 mm)
In the anterior region of the maxillae, the height measured from the >6-mm width crestal level to the inferior border of the nasal cavity is >16 mm. In the posterior region, the height from the alveolar ridge to the inferior wall of the maxillary sinus is at least 12 mm.
THERAPEUTIC OPTIONS
The available bone in the anterior and posterior regions allows for the placement of axial or straight implants.
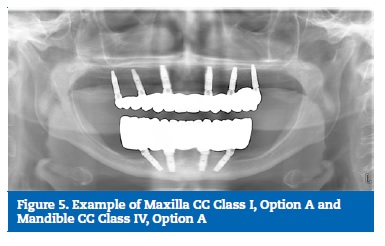
Option A � Placement of six straight equidistant implants. The four anterior implants are placed between the anterior walls of the maxillary sinuses. Their entry points are the lateral incisors and first premolars positions. The two posterior implants are placed in the first molar position. In case of opposing natural dentition with a functional second molar, the posterior implants should be placed in a way that enables function, preferably without a cantilever. A fixed cross-arch prosthesis without a distal cantilever is proposed (Figure 5).
�
�
Option B � Placement of four equidistant straight implants. The two anterior implants should be placed at the canine position and the two posterior implants at the first molar position. A fixed cross-arch prosthesis without a distal cantilever is proposed.
Option C � Placement of a full-arch removable prosthesis. An overdenture supported by four non-splinted implants is placed in the anterior region of the maxilla in the lateral incisor and first premolar positions.
DECIDING FACTOR
The main deciding factor for choosing Option A or B is the arch size. Short edentulous arches and, therefore, a small surgical space available between first molar positions suggest Option B. Based on the author�s clinical experience, this option is less prevalent. However, in cases weighting other biomechanical factors such as the presence of natural teeth in the opposing arch or parafunctional habits, Option A should be selected.
Option C (CCI, CCII and CCIII) is specifically indicated in patients with any cognitive or physical impairment. An edentulous older adult who needs daily assistance or has some degree of dependence could be a candidate for this therapeutic option, as it offers a favorable condition and maintenance of oral hygiene. Medical or economic factors and reduced patient compliance, which require minimally invasive surgical interventions and the lowest possible number of rehabilitation appointments, can also justify this option.2
Maxilla CCII
Anterior � available bone: height >16 mm; width >6 mm
Posterior � moderate resorption: height >8 mm and <12 mm; width >6 mm
In the anterior region, the height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the nasal cavity is >16 mm. In the posterior region, moderate posterior bone resorption is found. The bone height measured from the alveolar ridge with a >6-mm crestal width to the inferior wall of the maxillary sinus is >8 mm and <12 mm.
THERAPEUTIC OPTIONS
Due to moderate posterior bone resorption and a slight prominence of the maxillary sinus anterior wall, either a straight or a distally tilted implant could be considered in the fixed fullarch rehabilitation schemes.
Option A � Placement of six straight equidistant implants. Four implants are placed in the area limited by the anterior wall of the sinus, in the lateral incisor and first premolar positions. Two shorter implants are placed in the posterior region
in the first molar position.
Option B � Placement of four straight implants in the region limited by the anterior wall of the maxillary sinus, in the lateral incisor and first premolar positions. The posterior implants with the same length are tilted at a 17�- angle following the slope of the anterior wall maxillary sinus. The implant�s entry point is the first molar position with its apex in the second premolar position.
Option C � Similar to the Option C of the CCI Class.
DECIDING FACTOR
The main deciding factor for choosing Option A or B is the arch extension size, the maxillary sinus geometry and particularly poor bone quality. To avoid cantilever extensions, the posterior implant is placed in the molar position and, as this location has moderate resorption (height >8 mm and <12 mm; width >6 mm), a tilted implant can be placed to reach bone of better quality, instead of placing a shorter implant in a compromised bone.33, 34 In larger edentulous arches with a more pneumatized maxillary sinus and compromised posterior bone quality, Option B would be preferable.
In Option B, there is an increased A/P spread distance and, thus, a reduction in the cantilever length extension in cases where the natural opposing arch extends to the second molar position.
Maxilla CCIII
Anterior � moderate resorption: (height >12 mm and <16 mm; width >6 mm)
Posterior � advanced resorption: (height >4 mm and <8 mm; width >6 mm)
Moderate bone resorption is observed in the anterior region. The bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the nasal cavity is >12 mm and <16 mm. The posterior region is characterized by advanced bone resorption. The bone height measured from the alveolar ridge with a >6-mm crestal width to the inferior wall of the maxillary sinus is >4 mm and <8 mm.
THERAPEUTIC OPTIONS
The inter-antral distance and the available bone height are less favorable in this type of maxillae. The residual posterior bone height determines two types of fixed full-arch rehabilitation schemes.
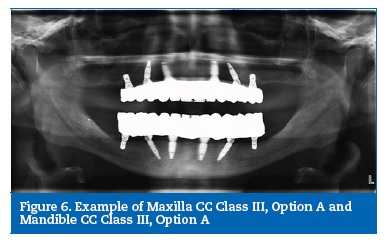
Option A � Placement of six implants in the maxilla. Two straight implants are placed in the lateral incisors position, two distally tilted implants in the premolar position and two short implants (> 4 mm and < 8 mm) in the posterior region in the molar position, allowing second molar occlusion without cantilevers (Figure 6).
�
�
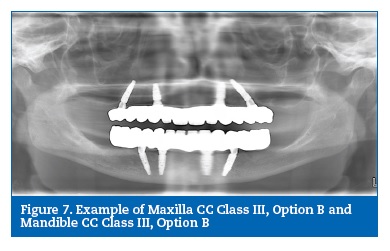
Option B � Placement of four implants in the region limited by the anterior wall of the maxillary sinus. Taking into account the variable slope of the anterior maxillary sinus wall, the distally placed implants should tilt at an angle of 17-30�. These implants usually emerge at the second premolar and are guided by the anterior maxillary sinus wall. An extended 14-mm cantilever reaching a first molar occlusion can be expected in the full-arch rehabilitation (Figure 7).
�
�
Option C � Placement of a full-arch overdenture supported by four implants. Since the inter-antral distance is limited, the mesiodistal space between the implants is short. The implants� entry points are in the central incisors and canine positions.
DECIDING FACTOR
The deciding factors for choosing Option A or B are the edentulous arch extension and the posterior bone quality. In larger edentulous arches, Option A might be preferable. Placing a short posterior implant increases the A/P spread distance.
Distal cantilever extension is short or absent and might be considered in patients with natural opposing arch with a second molar occlusion, patients with parafunctional habits or when low bone density is found in the posterior maxillae. Option B can be considered when the posterior bone quality does not allow placing a short implant, when grafting procedures should be avoided or if a second molar occlusion is unnecessary and the four implants are positioned to assure a stable fixed full-arch rehabilitation.35, 36
Maxilla CCIV
Anterior � advanced resorption: height >8 mm and <12 mm; width >6 mm
Posterior � severe resorption: height <4 mm or width <6 mm
Advanced bone resorption is seen in the anterior region. The bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the nasal cavity is >8 mm and <12 mm. The posterior region is characterized by severe bone resorption. The bone height measured from the alveolar ridge, with a <6-mm crestal width, to the inferior wall of the maxillary sinus is <4 mm.
THERAPEUTIC OPTIONS
In this class, the severe posterior bone resorption (<4 mm) and the maxillary sinus extension prevent implant placement in the area without a sinus lift technique. Therefore, two surgical protocols are suggested for a fixed full-arch rehabilitation with either a grafting or a graftless approach.
Option A � Placement of six implants. Four implants are placed in the anterior region of the maxilla. The two posterior implants are placed simultaneously with a bilateral sinus elevation procedure. Taking into consideration the reduced anterior bone height, only two anterior implants can be placed straight in the lateral incisors position, whereas the other two if necessary can be tilted (17-30o) to contour a proeminent anterior wall of the maxillary sinus, allowing a for an implant with a more frequent entry point in the first premolar position. (Figure 8).
�
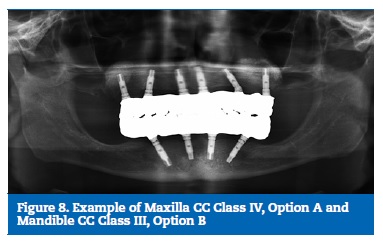
�
Option B � Placement of six implants with the same protocol as Option A for the anterior region of the maxilla. In the posterior region, two pterygoid or tuberosity implants are placed with an average angulation of 70.o to the occlusal plane. These two implants are usually longer (15-20mm). They pass through the maxillary tuberosity, the pyramidal process of the palatine bone and are fixed in a dense cortical bone of the pterygoid process of the sphenoid bone (Figure 9).
�
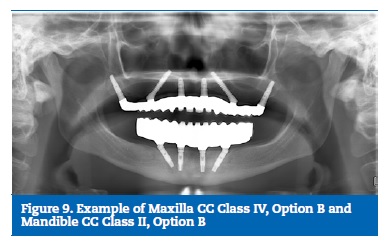
�
Option C � Although there is less bone availability compared to Option C of Class III, the rehabilitation scheme is similar, with four implants placed in the premaxilla to support an overdenture.
DECIDING FACTOR
Option A includes a sinus lift, which reestablishes adequate posterior bone volume for implant placement and is a wellknown approach widely supported in the literature with long-term predictability.37 The limitations of this option are the time to the final rehabilitation, morbidity and the impossibility of immediate loading. However, if the placement of four stable implants in the anterior area is possible, a serial loading protocol with immediate loading of the anterior four implants and a delayed loading after healing of the two posterior implants allows a provisional immediate fixed rehabilitation, thus increasing the quality of life of the patient. It is
also important to mention that using just four implants for the final rehabilitation in Class IV, as shown in Class III Option B, is not recommended, because the amount of anterior bone does not allow a good biomechanical load distribution of the implants, which could compromise long-term predictability.
One of the fundamental criteria for choosing Option B with pterygoid implants in the posterior region is the presence of maxillary sinus pathology, which increases the risk of biological complications in cases of Schneiderian membrane rupture and situations when posterior support is required for immediate loading.38 Both rehabilitation schemes represent a more complex surgical approach than those proposed for Class III. Although both are predictable, Option B is recognized as a less invasive approach, thus avoiding the higher morbidity associated with bone regeneration procedures.
However, this technique requires a more trained and experienced surgeon. For a more predictable immediate loading protocol or whenever a distal cantilever extension should be avoided, Option B may be considered more appropriate. In contrast, clinical conditions associated with a compromised mouth opening or a reduced inter-occlusal space should exclude this option.
Maxilla CCV
Anterior � severe resorption: height <8 mm or width <6 mm
Posterior � severe resorption: height <4 mm or width <6 mm
This class is characterized by severe anterior and posterior bone resorption. In the anterior region, the bone height measured from the osteotomy level, with a <6-mm crestal width, to the inferior border of the nasal cavity is <8 mm. Due to extensive
bone resorption or atrophy, the osteotomy procedure is smaller or not conducted. In the posterior region, the bone height measured from the alveolar ridge, with a <6-mm crestal width, to the inferior wall of the maxillary sinus is <4 mm.
This class is usually defined as a severely atrophic maxilla and is the most challenging class in full-arch rehabilitation.
THERAPEUTIC OPTIONS
Both the anterior and posterior areas have a minimum height and width, challenging the implant placement. Despite the different graft extension, the two fixed full-arch rehabilitation options proposed require horizontal regeneration procedures.
Option A � Placement of six or more straight implants at the same time or after a bilateral sinus lift procedure and horizontal regeneration. These implants are placed straight in the region of the sinus lift graft, usually with entry points corresponding to the canine, first premolar and first molar positions.
Due to extensive horizontal bone resorption, a horizontal augmentation procedure complements the surgical rehabilitation scheme (Figure 10).
�
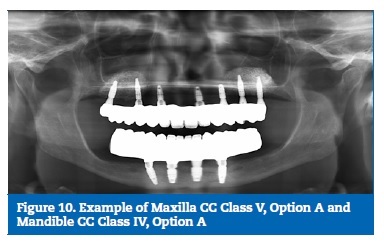
�
Option B � Placement of four short implants in the anterior region of the maxilla. Two straight implants are placed in the lateral incisors position and two implants adjacent to the maxillary sinus lift wall. In the posterior region of the maxilla, two zygomatic implants are placed tilted forward to obtain implant anchorage and stability in the zygomatic bone by increasing the implant length to ≥30 mm. Immediate loading is possible if the anterior implants are stable. When it is not possible to place stable implants in the anterior region, four zygomatic implants can be used. The main advantage of this option is allowing immediate loading without a grafting procedure.
This option requires a surgeon who is trained and skillful in this technique and should be considered as the last option in treatment planning due to the possible surgical complications (Figure 11).
�
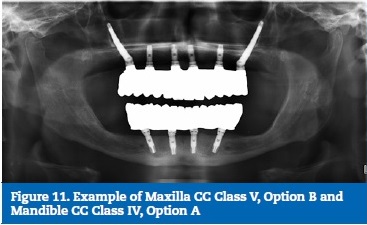
�
Option C � The severe bone resorption of this class requires short implants or augmentation of the premaxilla to stabilize the implants and support an overdenture.
DECIDING FACTOR
The key factor in deciding between these two approaches is whether the density of the remaining bone provides enough implant primary stability because both the previously mentioned options A and B are predictable. Therefore, two surgical protocols are suggested for a fixed full-arch rehabilitation depending on either a grafting or a graftless approach. However, in terms of the height level of atrophy, both techniques are sensitive to the patient�s preference, the risks involved, the expertise and the learning curve of the surgeon. Patient risk factors such as heavy smoking, diabetes, bruxism, sinus pathology and other compromising factors have to be considered in the decision process. Regardless of the vertical augmentation with sinus lift, treatment complexity increases in the presence of a thin ridge (<5 mm). An alveolar width deficiency of this magnitude is often associated with loss of buccal cortical and/or medullary bone, compromising the patients� facial profiles and adding complexity to the treatment plan.39 In these cases, a horizontal ridge augmentation to cover the buccal surface of every implant and re-establish the patients� anatomy is mandatory. Option B with zygomatic implants is one of several techniques described in the literature to approach the atrophic maxilla, with several prospective studies reporting successful outcomes as well as recognized advantages such as reduced treatment time, decreased morbidity and a smaller number of implants necessary to support fixed prostheses.40,41 Several studies have evaluated the use of zygomatic implants combined with standard implants for immediate loading and have reported a high survival rate of 95.8% to 100%, which implies that zygomatic implants may be used with immediate function protocols.42,44 Despite the high survival rate reported in the literature, attention should be drawn to the decision-making process due to the risk of intra- or post-operative complications involved: infections/sinusitis in the maxillary sinus, intraoral soft-tissue problems, oroantral fistula, orbital injury and intracranial penetration.40
Mandible CCI
Anterior � Available bone (height >16 mm; width >6 mm)
Posterior � Available bone (height >12 mm; width >6 mm)
In the anterior region of the mandible, the bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the mandible is >16 mm. In the posterior region, the distance from the >6-mm alveolar crestal width to a 2-mm safe distance from the mandibular canal is >12 mm.
THERAPEUTIC OPTIONS
Considering the posterior bone availability and the favorable anterior region with a higher density bone, two fixed full-arch options and two removable full-arch schemes are proposed.
Option A � Placement of six straight implants. Two anterior implants are placed in the lateral incisors position. Two distal implants are placed in the anterior region following the anatomically driven approach, and their entry point must have a safe anterior distance to the mental nerve and its possible loop. In the posterior region, two implants are placed in the first or second molar position depending on the functional molars of the opposing dentition.
Option B � Placement of four implants. Two straight implants are placed anteriorly to the mental foramen, in the canine position, and two straight implants in the posterior region, in the first molar position.
Option C � Use of an overdenture supported by two or four non-splinted implants placed in the anterior region of the mandible, in the same position as described for Option A.
DECIDING FACTOR
Both of the fixed full-arch schemes do not consider the presence of a distal cantilever. The extension and size of the arch are the main deciding factors for one of the options, i.e., in large arches, Option A should be selected. Other factors like
the presence of parafunctional habits (bruxism and clenching) or natural teeth in the opposing arch up to the first or second molar may also justify that option. The rationale proposed for a removable option follows the principles mentioned for Maxilla CCI-CCIV. Several randomized clinical trials and a meta- analysis confirm both of the options proposed.45 - 47 Thus, the economic, biomechanics and clinical situation should guide the clinician and the patient in which option to choose.27
Mandible CCII
Anterior � Available bone (height >16 mm; width >6 mm)
Posterior � Moderate resorption (height >8 mm and <12 mm; width >6 mm)
The anterior region still has a favorable amount of available bone. The bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the mandible is >16 mm. In the posterior region, moderate posterior bone resorption is observed. The bone height measured from the alveolar crest, with a >6-mm crestal width, to a 2-mm safe distance from the mandibular canal, is >8 mm and <12 mm.
THERAPEUTIC OPTIONS
Considering the posterior low bone availability and the favorable anterior region with higher bone density, two fixed full-arch options and two removable full-arch schemes are proposed.
Option A � Placement of six straight implants. The available anterior bone length enables the placement of four axial implants. Their position and the surgical approach are similar to those of the anterior implants proposed for Mandible CCI Option A. The reduced bone height in the first molar position requires the use of short implants in this area.
Option B � Placement of four implants in the anterior region. The two most anterior implants are placed vertically in the lateral incisors position. Taking into consideration the posterior bone height availability over the mandibular canal, two tilted implants with entry points slightly posterior to the mental foramina, usually at the second premolar position, can be placed. Since an angulation of 17-30� is used, their trajectory passes forward the mental nerve loop. In cases with a maximum mental nerve loop length of 5.7 mm, the implant entry point should coincide with the mental foramen.48 In this rehabilitation scheme, a distal 10-to-14-mm cantilever in the first molar position should be considered (Figure 9).
Option C � Similar to the rehabilitation schemes proposed for Mandible CCI. Based on the principle proposed for Mandible CCI, the same biomechanical factors support Option A without a distal cantilever. If none of the mentioned factors are present, Option B can be a predictable alternative approach. According to a 3-year prospective study,49 no clinical differences were found when comparing schemes similar to Mandible CCI Option B (four straight implants) and Mandible CCII Option B (four implants with the posterior implants tilted). In this study, implant success criteria and mechanical prosthesis complications were evaluated. This work gives rise to further evidence-based studies to validate the Option B proposed for Mandible CCI.
Mandible CCIII
Anterior � Moderate resorption (height >12 mm and <16 mm; width >6 mm)
Posterior � Advanced resorption (height >4 mm and <8 mm; width >6 mm)
Moderate bone resorption is found in the anterior region. The bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the mandible is >12 mm and <16 mm. In the posterior region, advanced posterior bone resorption is characterized by a bone height >4 mm and <8 mm measured from the alveolar crest, with a >6-mm crestal width, to a 2-mm safe distance from the mandibular canal.
THERAPEUTIC OPTIONS
Taking into consideration the advanced posterior bone resorption with a short bone height and moderate anterior bone resorption, two fixed full-arch options and two full-arch removable schemes are proposed.
Option A � Placement of four implants in the anterior region and two in the posterior region. The implants placed in the anterior region follow the surgical and prosthodontic criteria of Mandible CCII Option B. In addition, two short posterior implants are placed in the first molar position (Figure 6).
Option B � Similar to Option B of Mandible CCII. Taking into consideration the reduced posterior bone height available, the entry points of the distal implants should be aligned with the first premolar. In this rehabilitation scheme, a distal cantilever should be considered (Figure 7, Figure 8).
Option C � Taking into consideration a reduced implant length, the removable rehabilitation schemes proposed are similar to Mandible CCI and CCII.
DECIDING FACTOR
Regarding the bone resorption observed, the same deciding factors of Mandible CCI and CCII should be considered. Option B � placing four implants between the mental foramina, is a simple and predictable option. The use of short implants is currently considered predictable, and in several cases, Option A might be more favorable by placing a short implant in the molar region since it avoids cantilevers and allows a second molar occlusion.50, 51
Mandible CCIV
Anterior � Advanced resorption (height >8 mm and <12 mm; width >6 mm)
Posterior � Severe resorption (height < 4mm or width <6 mm)
Advanced bone resorption is confirmed in the anterior region of the mandible. The bone height measured from the osteotomy level, with a >6-mm crestal width, to the inferior border of the mandible is >8 mm and <12 mm. The posterior region presents severe bone resorption. The bone height measured from the alveolar crest, with a <6-mm crestal width, to a 2-mm safe distance from the mandibular canal is <4 mm.
THERAPEUTIC OPTIONS
In this class, the posterior bone height (<4 mm) precludes the placement of short implants, unless vertical bone regeneration procedures are performed. Hence, two options for the surgical approach are described.
Option A � Placement of four equidistant implants in the anterior region of the mandible. Two straight implants are placed in the lateral incisors position and the two other implants are placed tilted at a 17� angle with entry points coincident with the mental foramen or slightly posterior to it (Figure 5, Figure 10, Figure 11).
Option B � Vertical bone grafting in the posterior region for the placement of two implants in the position of the first molar. The length of the implants should range from 6 to 8 mm. Regarding the interforaminal region of the mandible, the surgical approach is the same as previously described in Option A.
Option C � Similar to the previously described removable options for Mandible Classes I, II and III.
DECIDING FACTOR
Placing four implants in between mental foramina, as mentioned earlier, is a simple and predictable option and is considered the most favorable option for this level, compared to Option B with vertical augmentation of the posterior mandible, to place an implant in the molar area. Individual patient-related factors must be analyzed to decide the suitable number of implants and the risk/benefit ratio associated with bone graft procedures on the posterior mandible.
Mandible CCV
Anterior severe resorption (height <8 mm or width <6 mm)
Posterior severe resorption (height <4 mm or width <6 mm)
A severe bone resorption pattern is observed both in the anterior and posterior regions. In the anterior region, the bone height measured from the osteotomy level, with a <6-mm crestal width, to the inferior border of the mandible, is <8-mm.
As described in Mandible CCIV, the same values are seen in the posterior region.
THERAPEUTIC OPTIONS
Two treatment options are suggested for these patients, using short implants in the anterior area versus major augmentation.
Both the anterior and posterior areas have a minimum height and width, challenging the implant placement.
Option A � Placement of four short straight implants (4 or 6 mm) equidistant in the anterior region. The two anterior implants are placed in the lateral incisors position and the two remaining in the first premolars position at a safe distance from the mental foramen.
Option B � A more invasive surgery to augment the height and width of the mandible. In this option, an extraoral autogenous bone graft is suggested (hip, rib, calvarium). Four or six axial implants are placed in the same positions and with the
same lengths as referred in the Mandible CC II Option A or B scheme.
Option C � Similar to the previously described removable options for Mandible Classes I, II, III and IV using two or four short implants.
DECIDING FACTOR
The surgeon�s expertise should be the main deciding factor for performing one of the previously described techniques since a severely atrophic mandible presents high risk for potential complications, mainly mental nerve injury, mandibular fracture or hemorrhagic accidents. Both therapeutic options are described in a 10-year follow-up randomized controlled trial.52 According to this study, the four short implant option presented a higher cumulative survival rate (98.8%) compared to the augmentation procedures (88%). Less morbidity in the patient and retreatment survival were also more favorable in this option. More recently, a systematic review
and meta-analysis that evaluated vertical ridge augmentation procedures in the atrophic mandible recognized that, if 4 mm of vertical augmentation is needed, any technique � inlay block grafting, onlay block grafting or osteogenesis distraction � should be predictable in healthy patients.53
Discussion
The aim of this paper is to propose the first patient-centered decision-aid tool for fixed and removable full-arch rehabilitation of the maxilla and the mandible. This type of classification system should not be perceived as a clinical algorithm or a decision tree. It should provide a justified suggestion of a possibly preferable treatment option but not dictate it.
Contrary to previous descriptions found in the literature, this classification system was developed focused on patient individuality rather than on the implant system technique.
Previous classifications have emphasized the prosthodontic- driven implant concept.23 Papadimitriou et al. proposed a classification based on 100 CBCT analyses previous to implant planning with a software application.23 Although this classification expressed four different levels of jaws atrophy, it was brand-specific and implant-design-specific (StraumannR Tissue level). Despite its long-term clinical outcome assessment, this implant system lacks prosthodontic flexibility when a screw-retained full-arch rehabilitation with tilted implants is proposed.54, 56 As previously mentioned, tilted implants may avoid the use of cantilevers in cases where limited bone height is found in the first molar position of edentulous maxillae and mandibles. However, the rehabilitation schemes proposed by these authors only consider straight implants. Furthermore, and taking into consideration its virtual nature, no intra-surgical modification of the edentulous ridge and no implant loading protocol were mentioned or considered. Possible considerations related to the patients� clinical history or risk factors influencing the therapeutic option were also not included.
Another classification system suggested a complete arch site classification based on four implants, as originally proposed by Branemark and later developed by Mattsson and Krekmanov.33, 34, 57 The system proposed by Jensen22 was based on implant placement strategies for an immediate loading protocol. Based on an anatomically driven implant placement, areas of high-density bone in the edentulous maxilla and mandible were the key factors for a predictable high insertion torque. Although accepted, this principle contradicts the current biological and prosthodontically driven standard. Regions close to the maxillary sinus and the nasal cavity in the maxilla or the inferior border of the mandible, or the inferior alveolar nerve, are described as anchors for the apical part of a two-piece implant (NobelActive NobelBiocareR). Once again, this description is purely based on one implant system and its macrogeometry. Surgical techniques proposing a transverse buccal-to-palatal/lingual implant positioning of the distally tilted implants in the mandible may represent an increased risk of fenestration and hemorrhagic accidents in the first molar region with a lingual undercut ridge.58 Although Jensen�s22 description may reflect extensive surgical experience, its application cannot be considered as �user-friendly� or reproducible among clinicians. In addition, it also did not take into account potential biomechanical risk factors for the patient subjected to the surgical technique. Parafunctional habits, arch size or type, and extension and type of the opposing arch are not addressed as considerations that may modify the rehabilitation scheme.
The limitations identified in both the described classifications have opened the field for discussion. Taking into consideration that patient-related factors potentially interfere with treatment planning, should we not develop a patient-centered classification system for an edentulous maxilla and mandible?
The positive answer to this question was this paper�s rationale. By achieving this, the authors of this manuscript set a significantly relevant path in the integration of these factors into a new classification for fixed or removable full-arch rehabilitation of edentulous jaws.
For each of the five edentulous classes, fixed and removable full-arch rehabilitation schemes were proposed. By providing a broad and flexible spectrum of rehabilitation options, we are providing a tool where the patient�s particularities and needs are taken into account. This viewpoint contrasts with the previous �all-on-four� or �all-on-six� dichotomic principle.59 - 65 By adding a removable option, we are as well addressing the needs of an increasingly aging population and demanding economic situations.2
Contrary to previous classifications, the rehabilitation schemes here proposed are not mainly implant-system dependent. This perspective is in agreement with the findings of a recent systematic review, which concluded that there was not enough available evidence suggesting that any specific implant or implant feature affects the treatment outcome in the maxilla of fully edentulous patients.66 Although a similar analysis is lacking for the mandible, the authors of this paper have adopted the same viewpoint.
The Maxilla CC classes rehabilitation scheme for a fixed full-arch rehabilitation suggesting six implants in cases of anterior and posterior bone availability is in accordance with the results of a meta-analysis.46 When evaluating post-loading implant failure in edentulous maxillae, in terms of the impact of implant number or position, fixed full arches with six or more implants presented favorable results. A low implant failure rate of 0.28% was found. A comparison with fixed full-arch schemes based on four implants could not be made due to a low number of high-quality studies. However, both of the options described are in accordance with the tendency found by Mericske-Stern considering the optimal number of implants for cross-arch fixed prosthesis and a minimally invasive, patient-centered approach.7, 67
Considering the previously mentioned meta-analysis for the edentulous mandible, the post-loading implant failure rate in a fixed full-arch rehabilitation with four implants is statistically significantly higher when compared to five or more implants. The CC classes for the edentulous mandible with any type of anterior and posterior bone availability � CCI, CCII and CIII Option A � are in agreement with these results. Bone augmentation procedures, as proposed in the Mandible CCV Option B, were not the focus of the meta-analysis. As previously mentioned in the deciding factor section of this class, favorable results were found in healthy patients when vertical augmentation procedures were applied.53
Although satisfactory results have been obtained with both all-on-four, all-on-six and, in some exceptional cases, more than six implants, these full-arch rehabilitation schemes should not be generalized and blindly matched with all edentulous cases. Biological considerations such as bone quality and quantity, soft-tissue conditions, medical factors, oral hygiene, the biomechanical profile of the type of the opposing jaw, and parafunctional habits should be weighed before deciding the rehabilitation option.27 Since there is a lack of evidence correlating some of these factors with the survival and success rates of a full-arch rehabilitation, an extrapolation from the available evidence of partial fixed prostheses was considered to be the logical next step. In this regard, several risk factors proposed as modifiers of the CC classes� therapeutic options are identified in the available literature.
For example, bruxism was mentioned as a predictor for implant failure with an odds ratio of 2.71 (95% CI, 1.25, 5.88) in relation to non-bruxers.68 Mechanical and technical complications with implant-supported prostheses were also found.
In a different study, based on a sample of 1406 patients, a cluster behavior of dental implant failures with factors such as bruxism, poor quality bone, age of patient or smoking were found to exert a harmful effect at an implant level.69 Some of these risk indicators and others such as diabetes type 1, bleeding disorders, or intake of medication for osteonecrosis (e.g. oral bisphosphonates) have already been highlighted in previous reviews.70, 71
Taking into consideration the possible effect of distal cantilevers in implant-supported prostheses, the available evidence does not support any correlation between peri-implant bone loss and cantilever extension.71 However, minor mechanical complications were found when cantilevers were present.73 When this extension is greater than 14 mm and in occlusion with a natural second molar, an increased mechanical risk can be expected.74 This factor was also considered a deciding factor in the present classification. It should be noted that the available evidence regarding the role of cantilevers is scarce, heterogeneous, lacks results of clinical trials reporting appropriate outcomes and often excludes patients with parafunctional habits.75 Therefore, depending on the risk factors identified during treatment planning, this classification system proposes a decrease of tension and stress distribution across more implants or a minimally invasive approach when required by the patient�s systemic condition.
The values proposed in each CC class may not match all types of clinical cases as they represent a general averaged standard. A retrospective cohort analysis reporting the implant and prosthodontic success of each rehabilitation scheme will be published to underline the clinical relevance of the proposed classification system.
Finally, assuming a pyramidal complexity structure, the CC also helps with the clinical case level assessment. Although most of the CC rehabilitation schemes may be classified as Advanced or Complex oral surgery procedures, they present different levels of surgical difficulty that increase with jaw atrophy.16 On a Complex level, different degrees of complexity can be found, and this has been rarely described in the literature so far. An example of this situation is the comparison between the difficulty levels of the Maxilla CCI Option B and the Maxilla CCV Option A. Both are Complex treatment options but require different learning curves and surgical expertise and experience. By stating these differences, we intend to optimize communication between clinicians and also recognize the importance of referral in certain clinical cases.
Conclusions
This paper proposed a comprehensible and �user-friendly� patient-centered classification system of the different fixed prosthodontic options for edentulous maxilla and mandible.
In contrast to previous descriptions, this classification system was developed focusing on the patient rather than on the implant system technique. This approach for a classification system is new and has not been previously described. The five levels of jaw anatomy and the illustrated fixed full-arch schemes aim to aid clinicians during treatment planning while underlining a pyramidal complexity hierarchy of the different classes, from simple to complex. Besides being helpful, this classification also aims to optimize and simplify, thus creating a system of communication between clinicians and patients.
�
References
1. Carlsson GE, Omar R. The future of complete dentures in oral rehabilitation. A critical review. J Oral Rehabil. 2010;37:143-56.
2. Schimmel M, Muller F, Suter V, Buser D. Implants for elderly patients. Periodontol 2000. 2017;73:228-40.
3. Polzer I, Schimmel M, Muller F, Biffar R. Edentulism as part of the general health problems of elderly adults. Int Dent J. 2010;60:143-55.
4. de Bruyn H, Collaert B, Linden U, Bjorn AL. Patient�s opinion and treatment outcome of fixed rehabilitation on Branemark implants. A 3-year follow-up study in private dental practices. Clin Oral Implants Res. 1997;8:265-71.
5. Dierens M, Collaert B, Deschepper E, Browaeys H, Klinge B, De Bruyn H. Patient-centered outcome of immediately loaded implants in the rehabilitation of fully edentulous jaws. Clin Oral Implants Res. 2009;20:1070-7.
6. De Bruyn H, Raes S, Matthys C, Cosyn J. The current use of patient-centered/reported outcomes in implant dentistry: a systematic review. Clin Oral Implants Res. 2015;26 Suppl 11:45-56.
7. Pommer B, Mailath-Pokorny G, Haas R, Busenlechner D, Furhauser R, Watzek G. Patients� preferences towards minimally invasive treatment alternatives for implant rehabilitation of edentulous jaws. Eur J Oral Implantol. 2014;7 Suppl 2:S91-109
8. Arvidson K, Esselin O, Felle-Persson E, Jonsson G, Smedberg JI, Soderstrom U. Early loading of mandibular full-arch bridges screw retained after 1 week to four to five Monotype((R)) implants: 3-year results from a prospective multicentre study. Clin Oral Implants Res. 2008;19:693-703.
9. Barbier L, Abeloos J, De Clercq C, Jacobs R. Peri-implant bone changes following tooth extraction, immediate placement and loading of implants in the edentulous maxilla. Clin Oral Investig. 2012;16:1061-70.
10. Degidi M, Nardi D, Piattelli A. 10-year follow-up of immediately loaded implants with TiUnite porous anodized surface. Clin Implant Dent Relat Res. 2012;14:828-38.
11. Tealdo T, Bevilacqua M, Menini M, Pera F, Ravera G, Drago C, et al. Immediate versus delayed loading of dental implants in edentulous maxillae: a 36-month prospective study. Int J Prosthodont. 2011;24:294-302.
12. Testori T, Meltzer A, Del Fabbro M, Zuffetti F, Troiano M, Francetti L, et al. Immediate occlusal loading of Osseotite implants in the lower edentulous jaw. A multicenter prospective study. Clin Oral Implants Res. 2004;15:278-84.
13. Jokstad A, Ellner S, Gussgard A. Comparison of two early loading protocols in full arch reconstructions in the edentulous maxilla using the Cresco prosthetic system: a three-arm parallel group randomized-controlled trial. Clin Oral Implants Res. 2011;22:455-63.
14. Vercruyssen M, van de Wiele G, Teughels W, Naert I, Jacobs R, Quirynen M. Implant- and patient-centred outcomes of guided surgery, a 1-year follow-up: An RCT comparing guided surgery with conventional implant placement. J Clin Periodontol. 2014;41:1154-60.
15. Papaspyridakos P, Chen CJ, Chuang SK, Weber HP. Implant loading protocols for edentulous patients with fixed prostheses: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014;29 Suppl:256-70.
16. Dawson A, Chen S, Implantology ITf. The SAC Classification in Implant Dentistry: Quintessence Pub; 2009. ISBN: 9781850971887
17. Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1988;17:232-6.
18. McGarry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR, Koumjian JH. Classification system for complete edentulism. The American College of Prosthodontics. J Prosthodont. 1999;8:27-39.
19. Wical KE, Swoope CC. Studies of residual ridge resorption. I. Use of panoramic radiographs for evaluation and classification of mandibular resorption. J Prosthet Dent. 1974;32:7-12.
20. Branemark PI, Hansson BO, Adell R, Breine U, Lindstrom J, Hallen O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132
21. Jemt T. Fixed implant-supported prostheses in the edentulous maxilla. A five-year follow-up report. Clin Oral Implants Res. 1994;5:142-7.
22. Jensen OT. Complete arch site classification for all-on-4 immediate function. J Prosthet Dent. 2014;112:741-51 e2.
23. Papadimitriou DE, Salari S, Gannam C, Gallucci GO, Friedland B. Implant-prosthodontic classification of the edentulous jaw for treatment planning with fixed rehabilitations. Int J Prosthodont. 2014;27:320-7.
24. Fradeani M. Esthetic Rehabilitation in Fixed Prosthodontics: Quintessence Publishing Company; 2004. ISBN: 9781850971085
25. Bidra AS, Touloumi F, Wu R. Differences in Lip Support with and without Labial Flanges in a Maxillary Edentulous Population. Part 4: Patient-Centered Analysis. J Prosthodont. 2018;27:29-34.
26. Penarrocha-Oltra D, Penarrocha-Diago M, Canullo L, Covani U, Penarrocha M. Patient-reported outcomes of immediate versus conventional loading with fixed full-arch prostheses in the maxilla: a nonrandomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29:690-8.
27. Schwarz F, Sanz-Martin I, Kern JS, Taylor T, Schaer A, Wolfart S, et al. Loading protocols and implant supported restorations proposed for the rehabilitation of partially and fully edentulous jaws. Camlog Foundation Consensus Report. Clin Oral Implants Res. 2016;27:988-92.
28. Carames J PAS, Chen A. Assessment of host-related risk factors in immediate loading: a 3-year retrospective cohort study. 2006.
29. Harris D, Horner K, Grondahl K, Jacobs R, Helmrot E, Benic GI, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res. 2012;23:1243-53.
30. Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817-26.
31. Buser D BU, Wismeijer D. Achieving optimal esthetic results. ITI Treatment guide: implant therapy in the esthetic zone: single tooth replacement. Berlin: Quintessence Publishing Co; 2007. 25-230 p. ISBN: 9783938947104
32. Grunder U, Gracis S, Capelli M. Influence of the 3-D bone-toimplant relationship on esthetics. Int J Periodontics Restorative Dent. 2005;25:113-9.
33. Krekmanov L, Kahn M, Rangert B, Lindstrom H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15:405-14
34. Mattsson T, Kondell PA, Gynther GW, Fredholm U, Bolin A. Implant treatment without bone grafting in severely resorbed edentulous maxillae. J Oral Maxillofac Surg. 1999;57:281-7.
35. Esposito M, Barausse C, Pistilli R, Sammartino G, Grandi G, Felice P. Short implants versus bone augmentation for placing longer implants in atrophic maxillae: One-year post-loading results of a pilot randomised controlled trial. Eur J Oral Implantol. 2015;8:257-68.
36. Pommer B, Busenlechner D, Furhauser R, Watzek G, Mailath-Pokorny G, Haas R. Trends in techniques to avoid bone augmentation surgery: Application of short implants, narrow-diameter implants and guided surgery. J Craniomaxillofac Surg. 2016;44:1630-4.
37. Starch-Jensen T, Aludden H, Hallman M, Dahlin C, Christensen AE, Mordenfeld A. A systematic review and meta-analysis of long-term studies (five or more years) assessing maxillary sinus floor augmentation. Int J Oral Maxillofac Surg. 2018;47:103-16.
38. Bidra AS, Huynh-Ba G. Implants in the pterygoid region: a systematic review of the literature. Int J Oral Maxillofac Surg. 2011;40:773-81.
39. Tolstunov L. Classification of the alveolar ridge width: implant-driven treatment considerations for the horizontally deficient alveolar ridges. J Oral Implantol. 2014;40 Spec No:365-70.
40. Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J Oral Maxillofac Surg. 2016;74:1949-64.
41. Esposito M, Worthington HV. Interventions for replacing missing teeth: dental implants in zygomatic bone for the rehabilitation of the severely deficient edentulous maxilla. Cochrane Database Syst Rev. 2013(9):CD004151.
42. Aparicio C, Manresa C, Francisco K, Ouazzani W, Claros P, Potau JM, et al. The long-term use of zygomatic implants: a 10-year clinical and radiographic report. Clin Implant Dent Relat Res. 2014;16:447-59.
43. Davo R, Pons O. 5-year outcome of cross-arch prostheses supported by four immediately loaded zygomatic implants: A prospective case series. Eur J Oral Implantol. 2015;8:169-74
44. Dos Santos PL, Silva GH, Da Silva Pereira FR, da Silva RD, Campos ML, Mattos TB, et al. Zygomatic Implant Subjected to Immediate Loading for Atrophic Maxilla Rehabilitation. J Craniofac Surg. 2016;27:e734-e7.
45. Acham S, Rugani P, Truschnegg A, Wildburger A, Wegscheider WA, Jakse N. Immediate loading of four interforaminal implants supporting a locator-retained mandibular overdenture in the elderly. Results of a 3-year randomized, controlled, prospective clinical study. Clin Implant Dent Relat Res. 2017;19:895-900.
46. Kern JS, Kern T, Wolfart S, Heussen N. A systematic review and meta-analysis of removable and fixed implantsupported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res. 2016;27:174-95.
47. Muller F, Duvernay E, Loup A, Vazquez L, Herrmann FR, Schimmel M. Implant-supported mandibular overdentures in very old adults: a randomized controlled trial. J Dent Res. 2013;92(12 Suppl):154S-60S.
48. Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012;23:1022-30.
49. Krennmair S, Weinlander M, Malek M, Forstner T, Krennmair G, Stimmelmayr M. Mandibular Full-Arch Fixed Prostheses Supported on 4 Implants with Either Axial Or Tilted Distal Implants: A 3-Year Prospective Study. Clin Implant Dent Relat Res. 2016;18:1119-33.
50. Sun HL, Huang C, Wu YR, Shi B. Failure rates of short (</= 10 mm) dental implants and factors influencing their failure: a systematic review. Int J Oral Maxillofac Implants. 2011;26:816-25
51. Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol. 2011;38:667-76.
52. Stellingsma K, Raghoebar GM, Visser A, Vissink A, Meijer HJ. The extremely resorbed mandible, 10-year results of a randomized controlled trial on 3 treatment strategies. Clin Oral Implants Res. 2014;25:926-32.
53. Elnayef B, Monje A, Gargallo-Albiol J, Galindo-Moreno P, Wang HL, Hernandez-Alfaro F. Vertical Ridge Augmentation in the Atrophic Mandible: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2017;32:291-312.
54. Buser D, Janner SF, Wittneben JG, Bragger U, Ramseier CA, Salvi GE. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14:839-51.
55. Gamper FB, Benic GI, Sanz-Martin I, Asgeirsson AG, Hammerle CHF, Thoma DS. Randomized controlled clinical trial comparing one-piece and two-piece dental implants supporting fixed and removable dental prostheses: 4- to 6-year observations. Clin Oral Implants Res. 2017;28:1553-9.
56. Zhang XX, Shi JY, Gu YX, Lai HC. Long-Term Outcomes of Early Loading of Straumann Implant-Supported Fixed Segmented Bridgeworks in Edentulous Maxillae: A 10-Year Prospective Study. Clin Implant Dent Relat Res. 2016;18:1227-37.57. Branemark PI, Svensson B, van Steenberghe D. Ten-year survival rates of fixed prostheses on four or six implants ad modum Branemark in full edentulism. Clin Oral Implants Res. 1995;6:227-31.
58. Chan HL, Benavides E, Yeh CY, Fu JH, Rudek IE, Wang HL. Risk assessment of lingual plate perforation in posterior mandibular region: a virtual implant placement study using cone-beam computed tomography. J Periodontol. 2011;82:129-35.
59. Agliardi EL, Pozzi A, Stappert CF, Benzi R, Romeo D, Gherlone E. Immediate fixed rehabilitation of the edentulous maxilla: a prospective clinical and radiological study after 3 years of loading. Clin Implant Dent Relat Res. 2014;16:292-302.
60. Bergkvist G, Sahlholm S, Nilner K, Lindh C. Implantsupported fixed prostheses in the edentulous maxilla. A 2-year clinical and radiological follow-up of treatment with non-submerged ITI implants. Clin Oral Implants Res. 2004;15:351-9.
61. Francetti L, Romeo D, Corbella S, Taschieri S, Del Fabbro M. Bone level changes around axial and tilted implants in full-arch fixed immediate restorations. Interim results of a prospective study. Clin Implant Dent Relat Res. 2012;14:646-54.
62. Johansson B, Friberg B, Nilson H. Digitally planned, immediately loaded dental implants with prefabricated prostheses in the reconstruction of edentulous maxillae: a 1-year prospective, multicenter study. Clin Implant Dent Relat Res. 2009;11:194-200.
63. Malo P, de Araujo Nobre M, Lopes A, Ferro A, Gravito I. All-on-4(R) Treatment Concept for the Rehabilitation of the Completely Edentulous Mandible: A 7-Year Clinical and 5-Year Radiographic Retrospective Case Series with Risk Assessment for Implant Failure and Marginal Bone Level. Clin Implant Dent Relat Res. 2015;17 Suppl 2:e531-41.
64. Meloni SM, De Riu G, Pisano M, Cattina G, Tullio A. Implant treatment software planning and guided flapless surgery with immediate provisional prosthesis delivery in the fully edentulous maxilla. A retrospective analysis of 15 consecutively treated patients. Eur J Oral Implantol. 2010;3:245-51
65. Patzelt SB, Bahat O, Reynolds MA, Strub JR. The all-on-four treatment concept: a systematic review. Clin Implant Dent Relat Res. 2014;16:836-55.
66. Jokstad A, Sanz M, Ogawa T, Bassi F, Levin L, Wennerberg A, et al. A Systematic Review of the Role of Implant Design in the Rehabilitation of the Edentulous Maxilla. Int J Oral Maxillofac Implants. 2016;31 Suppl:s43-99.
67. Mericske-Stern R, Worni A. Optimal number of oral implants for fixed reconstructions: a review of the literature. Eur J Oral Implantol. 2014;7 Suppl 2:S133-53
68. Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Bruxism and dental implant treatment complications: a retrospective comparative study of 98 bruxer patients and a matched group. Clin Oral Implants Res. 2017;28:e1-e9.
69. Chrcanovic BR, Kisch J, Albrektsson T, Wennerberg A. Analysis of risk factors for cluster behavior of dental implant failures. Clin Implant Dent Relat Res. 2017;19:632-42.
70. Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants. 2009;24 Suppl:12-2771. Guazzo R, Sbricoli L, Ricci S, Bressan E, Piattelli A, Iaculli F. Medication-related osteonecrosis of the jaw and dental implants failures: a systematic review. J Oral Implantol. 2016.
72. Aglietta M, Siciliano VI, Zwahlen M, Bragger U, Pjetursson BE, Lang NP, et al. A systematic review of the survival and complication rates of implant supported fixed dental prostheses with cantilever extensions after an observation period of at least 5 years. Clin Oral Implants Res. 2009;20:441-51.
73. Torrecillas-Martinez L, Monje A, Lin GH, Suarez F, Ortega-Oller I, Galindo-Moreno P, et al. Effect of cantilevers for implant-supported prostheses on marginal bone loss and prosthetic complications: systematic review and metaanalysis. Int J Oral Maxillofac Implants. 2014;29:1315-21.
74. Abdulmajeed AA, Lim KG, Narhi TO, Cooper LF. Completearch implant-supported monolithic zirconia fixed dental prostheses: A systematic review. J Prosthet Dent. 2016;115:672-7 e1.
75. Romeo E, Storelli S. Systematic review of the survival rate and the biological, technical, and aesthetic complications of fixed dental prostheses with cantilevers on implants reported in longitudinal studies with a mean of 5 years follow-up. Clin Oral Implants Res. 2012;23 Suppl 6:39-49.
�
Joao Carames
E-mail address: caramesj@gmail.com
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare
�
Article history:
Received 11 October 2019
Accepted 8 November 2019
Available online 20 December 2019
