
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2019 | 60 (3) | 104-110
Original research
Microhardness and flexural strength after chemical aging of chlorhexidine delivery systems based on acrylic resin
Microdureza e resistência à flexão após envelhecimento químico de sistemas de libertação de clorexidina à base de resina acrílica
a Oral and Biomedical Sciences Research Unit (UICOB), Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
c Research Institute for Medicines (iMed.ULisboa), Faculdade de Farmácia, Universidade de Lisboa, Lisbon, Portugal
Joana Costa - cristina.neves@fmd.ulisboa.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 3
Original research
Pages - 104-110
Go to Volume
Article History
Received on 09/08/2019
Accepted on 30/09/2019
Available Online on 22/10/2019
Keywords
Original research
�
Microhardness and flexural strength after chemical aging of chlorhexidine delivery systems based on acrylic resin
Microdureza e resistencia a flexao apos envelhecimento qu�mico de sistemas de libertacao de clorexidina a base de resina acr�lica
�
Cristina Bettencourt Nevesa, Joana Costab,*, Lu�s Nepomucenob, Ana Madeirab, Jaime Portugala, Ana Bettencourtc
a Oral and Biomedical Sciences Research Unit (UICOB), Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal
b Faculdade de Medicina Dent�ria, Universidade de Lisboa, Lisbon, Portugal
c Research Institute for Medicines (iMed.ULisboa), Faculdade de Farm�cia, Universidade de Lisboa, Lisbon, Portugal�
�
http://doi.org/10.24873/j.rpemd.2019.10.458
�
Abstract
Objectives: To evaluate the effect of chlorhexidine incorporation on the microhardness and flexural strength of three reline acrylic resins, after a 28-day chemical aging process.
Methods: Forty-eight specimens were fabricated according to the several possible combinations of acrylic reline resin and concentrations of incorporated chlorhexidine (Kooliner � 0% vs. 2.5%; Ufi Gel Hard � 0% vs. 5%; and Probase Cold � 0% vs. 5%), to set 6 experimental groups (n=8). After a 4-week chemical aging process (pH fluctuation in artificial saliva, with cycles of 6 hours at pH=3 and 18 hours at pH=7), the Knoop microhardness (98.12 mN, 30 seconds) and flexural strength (1 kN, 5 mm/min) of all specimens were evaluated. Data were submitted to non-parametric statistical tests, according to Kruskal-Wallis and Mann-Whitney (α=0.05).
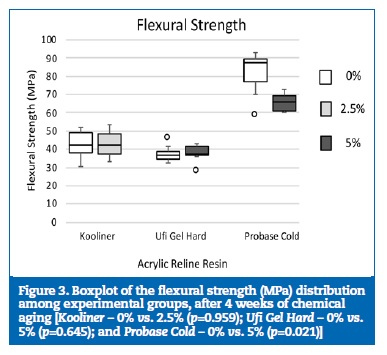
Results: Chlorhexidine incorporation did not significantly affect the microhardness of the three tested resins (Kooliner � p=0.798; Ufi Gel Hard � p=0.798; and Probase Cold � p=0.195). Although chlorhexidine incorporation did not influence the flexural strength of Kooliner (p=0.959) and Ufi Gel Hard (p=0.645), the incorporation of 5% chlorhexidine in Probase Cold led to a statistically lower flexural strength than that obtained without incorporation (p=0.021).
Conclusion: After chemical aging, the microhardness of chlorhexidine-incorporated acrylic resins is not affected. However, the incorporation of 5% chlorhexidine into Probase Cold negatively affects its flexural strength.
Keywords: Acrylic resins, Chlorhexidine, Denture relining, Denture stomatitis, Hardness, Flexural strength
�
Resumo
Objetivos:Avaliar o efeito da incorpora��o de clorexidina na microdureza e na resist�ncia a flex�o de tr�s resinas acr�licas de rebasamento, ap�s um processo de envelhecimento qu�mico de 28 dias.
M�todos: Um total de 48 esp�cimes foi fabricado de acordo com as diversas combina��es poss�veis entre resina acrilica de rebasamento e concentra��o de clorexidina incorporada (Kooliner � 0% vs. 2,5%; Ufi Gel Hard � 0% vs. 5%; e Probase Cold � 0% vs. 5%), de forma a criar 6 grupos experimentais (n=8). Ap�s um processo de envelhecimento quimico durante 4 semanas (varia��es de pH em saliva artificial, com ciclos de 6 horas em pH=3 e 18 horas em pH=7), foram avaliadas a microdureza Knoop (98,12 mN, 30 segundos) e a resist�ncia a flexao (1 kN, 5 mm/minuto) de todos os esp�cimes. Os dados obtidos foram submetidos a testes estat�sticos n�o param�tricos, segundo Kruskal-Wallis e Mann-Whitney (α=0,05).
Resultados: A incorpora��o de clorexidina nao influenciou de forma estatisticamente significativa (Kooliner � p=0,798; Ufi Gel Hard � p=0,798; e Probase Cold � p=0,195) os valores de microdureza de nenhuma das tr�s resinas acr�licas. Apesar da incorpora��o de clorexidina n�o ter influenciado a resist�ncia a flex�o de Kooliner (p=0,959) e de Ufi Gel Hard (p=0,645), a incorpora��o da Probase Cold com 5% de clorexidina conduziu a resist�ncia a flex�o estatisticamente mais baixa que a obtida sem incorpora��o (p=0,021).
Conclus�es: Ap�s envelhecimento qu�mico, n�o se verifica uma diminui��o nos valores de microdureza de resinas acr�licas incorporadas com clorexidina. Contudo, a incorpora��o de 5% de clorexidina em Probase Cold afeta negativamente os valores de resist�ncia a flex�o.
Palavras-chave: Resinas acrilicas, Clorexidina, Rebasamento, Estomatite prot�tica, Dureza, Resist�ncia a flex�o
�
Introduction
Tooth loss is associated with a decreased integrity of the masticatory system, with negative consequences in the functional and esthetic aspects, in speech and in self-esteem. 1, 2 Rehabilitation with removable dentures continues to be one of the most sought options.3 However, the progressive resorption of the alveolar ridge may lead to a decreased adaptation of the denture base to the underlying tissues.
The most common procedure to solve this problem is relining, which consists in placing a material, usually a reline acrylic resin, onto the base of the denture to fill the gap between the contour of the denture and the new contour of the tissues.4, 8
Acrylic resins used in dentures bases are polymeric biomaterials with proper mechanical properties, but their porous structure promotes microbial colonization and the development of oral diseases, such as denture stomatitis.9, 13
Despite the multifactorial etiology of this disease, it appears to be related to a quantitative increase of Candida species, especially Candida albicans,14, 17 a commensal fungal organism that can act as an opportunistic pathogen.18, 19 Treatment is complex and includes reducing the denture wearing time, denture relining and topical antifungal therapy.15, 20 - 23 Medical devices aimed to combine these two last-mentioned options have been proposed, such as reline acrylic resins, which act as reservoirs of antimicrobial agents, like chlorhexidine (CHX), thus allowing a continuous release of drugs at the site of infection.14, 24 - 25 CHX is an agent with antimicrobial properties against a large number of microorganisms, including Candida species.26, 28 When incorporated into resins, it has a high release in the first 2 to 7 days, which then decreases and remains constant for, at least, 28 days.17, 28 - 30
The concentration at which CHX offers antifungal activity but does not influence the properties of several reline resins has been established in some studies.31, 37 However, in those studies, chemical aging was not taken into account. Food and drinks can affect dental materials and intraoral pH values.38, 39
The objective of this study was to evaluate the effect of loading three reline acrylic resins with CHX on their microhardness and flexural strength, after a 28-day chemical aging process. The following hypotheses were studied: 1) there are no differences in microhardness between reline acrylic resins; 2) the reline acrylic resin does not influence flexural strength; 3) the incorporation of CHX does not influence the reline acrylic resin microhardness; and 4) the incorporation of CHX does not affect the flexural strength of the reline acrylic resin.
Materials and methods
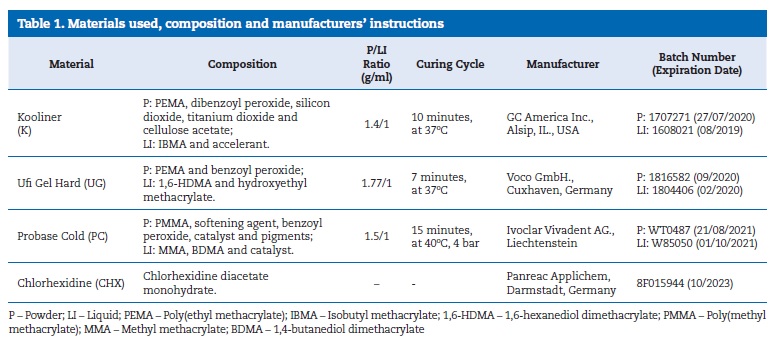
Three auto-polymerizing reline acrylic resins, presented in powder-liquid formulations, were selected. Two were direct reline resins: Kooliner (GC America Inc., Alsip, IL., USA), a non-crosslinking material, and Ufi Gel Hard (Voco GmbH., Cuxhaven, Germany), a crosslinking material; these are both composed of pre-polymerized poly(ethyl methacrylate) powder particles and also the monomers isobutyl methacrylate and 1,6-hexanediol dimethacrylate, respectively. The other one was an indirect reline resin: Probase Cold (Ivoclar Vivadent AG., Liechtenstein), which is composed of poly(methyl methacrylate) and methyl methacrylate (Table 1).
�
�
A chlorhexidine diacetate monohydrate (Panreac Applichem, Darmstadt, Germany) was also selected.
The powder of the reline acrylic resin and CHX were weighed using a precision balance (A&D Company, Limited, Tokyo, Japan), and the liquid was measured using a graduated pipette.
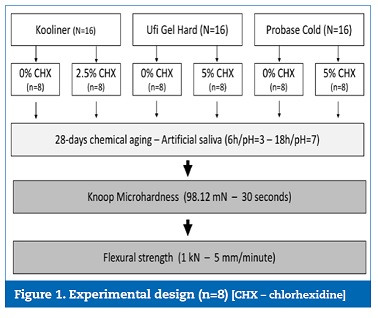
Two groups were established for each material: a control group, with a 0% concentration of CHX; and an experimental group, where a certain concentration of CHX was incorporated (Figure 1). Based on previous studies,31 - 37 a 2.5% CHX concentration was incorporated in the Kooliner experimental group and a 5% CHX concentration in both the Ufi Gel Hard and the Probase Cold experimental groups.
�
�
In each experimental group, CHX was incorporated and mixed with the powder of the corresponding reline acrylic resin, using a mortar and a pestle for homogenization. After mixing with the liquid monomer, eight specimens of each group (n=8) were prepared using rectangular-shaped stainless molds (64�10�3.3 mm).
During the recommended polymerization time of the direct reline resins, specimens were maintained under compression between two glass slabs, in an oven (Ehret, Mahlberg, Germany), at 37 � 2oC. Polymerization of the indirect reline resin was carried out in a pressure device (Ivomat, Ivoclar Vivadent, Schaan, Liechtenstein) at the recommended time, temperature and pressure (Table 1).
After polymerization, the specimens were removed from the mold and polished with a 600-grit silicon carbide paper (Carbimate Paper Discs, Buehler Ltd., Lake Bluff, IL., USA) with constant refrigeration. Each specimen was weighed (A&D Company,
Limited, Tokyo, Japan) and immersed in artificial saliva,35, 40 with a ratio of 1 g/5 mL in individual graduated falcon tubes. The specimens were stored at 37oC (Memmert, Schwabach, Germany) with constant gentle shaking (300 rpm) for 28 days. In order to simulate oral conditions, the samples were subjected to a protocol of chemical aging, based on cycles of 6 hours in artificial saliva at pH=3 interchanging with 18 hours in artificial saliva at pH=7. Between each change, the samples were washed with distilled water and dried with absorbent paper.
The Knoop microhardness test was performed (Duramin, Stuers DK 2750, Ballerup, Denmark) with a 98.12 mN load for 30 seconds. Twelve equidistant measurements were made in each specimen, and the mean value was used as the specimen�s microhardness (KHN).
A three-point flexural test was performed with a universal testing machine (Instron, Model 4502, Bucks, England), with a 1 kN load cell at a crosshead speed of 5 mm/min and a distance of 50 mm between supports. The width and thickness of each specimen were confirmed using a digital micrometer with a �0.01 mm precision (Mitutoyo Digimatic, MFG. Co. Ltd., Tokyo, Japan).
Data were statistically analyzed using IBM SPSS Statistics for Macintosh, version 25.0 (IBM Corp., Armonk, New York, USA). Since normality and homogeneity of variance were not verified (Shapiro-Wilk and Levene tests, p<0.05), data were submitted to Kruskal-Wallis and Mann-Whitney non-parametric tests (α=0.05).
Results
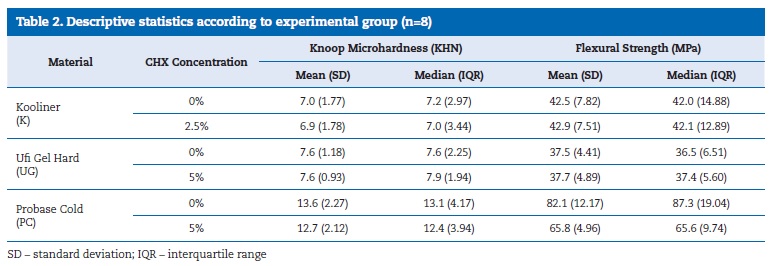
The microhardness mean value ranged between 6.9 KHN, in the Kooliner incorporated with 2.5% CHX, and 13.6 KHN, in the Probase Cold without CHX incorporation (Table 2). The flexural strength ranged between 37.5 MPa, in the Ufi Gel Hard without CHX incorporation, and 82.1 MPa, in the Probase Cold without CHX incorporation.
�
�
Probase Cold showed statiscally significantly (p<0.001) higher microhardness and flexural strength than the other two reline acrylic resins. No significant differences were found between Kooliner�s and Ufi Gel Hard�s microhardness (p=1.000) or flexural strength (p=0.542).
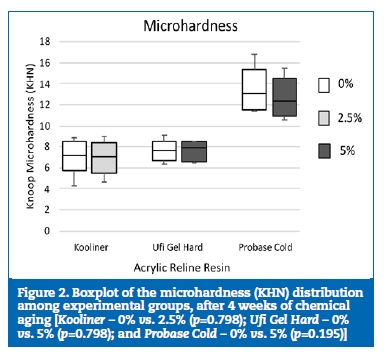
Microhardness was not statistically affected by CHX incorporation in any of the three reline acrylic resins (Kooliner � p=0.798; Ufi Gel Hard � p=0.798; and Probase Cold � p=0.195) (Figure 2).
�
�
The incorporation of CHX did not influence the flexural strength of Kooliner (p=0.959) or Ufi Gel Hard (p=0.645). However, incorporating 5% CHX into Probase Cold led to a statistically significant (p=0.021) decrease in flexural strength (Figure 3).
�
�
Discussion
Loading reline acrylic resins with CHX did not influence microhardness in any of the three materials studied after a chemical aging process. However, although flexural strength was not affected in Kooliner or Ufi Gel Hard, the incorporation of CHX decreased the flexural strength of Probase Cold.
The reline acrylic resins evaluated in this study were selected due to their chemical and structural differences.41,42
Kooliner and Ufi Gel Hard are both direct reline resins composed of poly(ethyl methacrylate) particles; however, Kooliner is also composed of isobutyl methacrylate, forming a non-crosslinking net, whereas Ufi Gel Hard is composed of 1,6-hexanediol dimethacrylate and forms a crosslinking net, thus being more complex than Kooliner.41,42 In turn, Probase Cold is an indirect reline resin composed of poly(methyl methacrylate) and methyl methacrylate that presents a reduced amount of residual monomer after its polymerization.41,42
The CHX concentration used to load each reline acrylic resin was based on the findings of previous studies.30, 37 A 2.5% CHX concentration in Kooliner and a 5% CHX concentration in Ufi Gel Hard and Probase Cold seem to reduce the microbiological activity of Candida albicans without affecting the mechanical properties of the reline resins.31, 33 - 34 Incorporating higher percentages of CHX could negatively influence the mechanical properties of the studied materials.31, 33
In order to simulate oral conditions, all specimens were aged immersed in artificial saliva in interchanging cycles of 6 hours at pH=3 and 18 hours at pH=7.39, 43 - 45
Since the reline acrylic resin may be considered a provisional material, and considering the time during which CHX release levels remain constant for an effective treatment of denture stomatitis, a 28-day aging period was selected to allow comparison with previous research studies.14, 17, 26, 28 - 30, 46
Given that Probase Cold presented higher microhardness and flexural strength than the other reline acrylic resins studied, the first and second null hypotheses are rejected. These results are in accordance with previous studies with different aging conditions.32, 33 The higher degree of conversion of Probase Cold could justify these results.4142
The third hypothesis is not rejected since, after a chemical aging process, the microhardness of the three reline acrylic resins was not affected by the CHX incorporation. These results agree with a previous study that included a thermal, and not chemical, aging protocol.32
Although the incorporation of resins with antimicrobial agents has shown a reduction of flexural strength,31, 33 47 - 52 in the present research, the flexural strength of Kooliner and Ufi Gel Hard was not influenced by the CHX incorporation. The results obtained in the present study agree with previous results found by this research group, where Kooliner loaded with 2.5% CHX and Ufi Gel Hard with 5% CHX did not show a negative impact on flexural strength, with different aging environments.32 - 33 The similar chemical constitution of these direct reline materials could explain why they were not affected.41 In contrast, loading Probase Cold with 5% CHX led to a decrease in flexural strength. So, the fourth null hypothesis is rejected.
Probase Cold has a different polymer matrix organization than Kooliner and Ufi Gel Hard. It is composed of poly(methyl methacrylate), and its polymerization cycle is achieved with high temperature and pressure.4142 Under these conditions, the presence of CHX particles may affect the degree of cure and induce some changes in the polymer shape and matrix, increasing the intermolecular distance between chains.47, 50, 53 - 54
However, although Probase Cold showed a decrease in flexural strength with the incorporation of CHX, under current experimental conditions, its mean flexural strength value was higher than that obtained with Kooliner and Ufi Gel Hard.
The three materials tested in the present study are reline acrylic resins that are not used independently in the oral cavity but always associated with a base denture material. Further research should be conducted to study the flexural and adhesive strength of these materials together. Likewise, other physical and mechanical properties of reline acrylic resins loaded with CHX, under a combination of thermal, chemical and mechanical aging, should be tested, in order to better reproduce the oral environment.
Conclusions
The indirect reline acrylic resin presented higher microhardness and flexural strength than the direct reline acrylic resins tested. After chemical aging, loading Kooliner or Ufi Gel Hard with CHX did not affect their microhardness and flexural strength. However, incorporating 5% chlorhexidine into Probase Cold decreased its flexural strength, even though its microhardness was not affected.
�
References
1. Yamamoto S, Shiga H. Masticatory Performance And Oral Health- Related Quality Of Life Before And After Complete Denture Treatment. J Prosthod Res. 2018;62:370-4.
2. Viola A, Takamiya A, Monteiro D, Barbosa D. Oral Health-Related Quality Of Life And Satisfaction Before And After Treatment With Complete Dentures In A Dental School In Brazil. J Prosthod Res. 2013;57:36-41.
3. Kranjčić J, Stunić M, Celebić A, Komar D, Mehulić K, Vojvodić D. Denture Relining As An Indicator Of Residual Ridge Resorption. Med Glas (Zenica). 2013;10:126-32.
4. Ahmad F, Dent M, Yunus N. Shear Bond Strength Of Two Chemically Different Denture Base Polymers To Reline Materials. J Prosthodont. 2009;18:596-602.
5. Van Meegen H, Kalk W. Improvement Of A Removable Complete Denture By Relining Or Rebasing. Ned Tijdschr Tandheelkd. 2011;118:545-51.
6. Hamanaka I, Shimizu H, Takahashi Y. Bond Strength Of A Chairside Autopolymerizing Reline Resin To Injection-Molded Thermoplastic Denture Base Resins. J Prosthodont Res. 2017;61:67-72.
7. Murata H, Seo R, Hamada T, Polyzois G, Frangou M. Dynamic Mechanical Properties Of Hard, Direct Denture Reline Resins. J Prosthet Dent. 2007;98:319-26.
8. Costa J, Matos A, Bettencourt A, Portugal J, Neves C. Effect Of Ethanol Solutions As Post-Polymerization Treatment On The Properties Of Acrylic Reline Resins. Rev Port Estomatol Med Dent Cir Maxilofac. 2016;57:215-22.
9. Salloum A. Effect Of 5.25% Sodium Hypochlorite On Color Stability Of Acrylic And Silicone Based Soft Liners And A Denture Base Acrylic Resin. J Indian Prosthodont Soc. 2014;14:179-86.
10. Dhir G, Berzins D, Dhuru V, Periathamby A, Dentino A. Physical Properties Of Denture Base Resins Potentially Resistant To Candida Adhesion. J Prosthodont. 2007;16:465-72.
11. Leles C, Machado A, Vergani C, Giampaolo E, Pavarina A. Bonding Strength Between A Hard Chairside Reline Resin And A Denture Base Material As Influenced By Surface Treatment. J Oral Rehabil. 2001;28:1153-7.
12. Bettencourt A, Neves C, de Almeida M, Pinheiro L, Oliveira S, Lopes L, Castro M. Biodegradation Of Acrylic Based Resins: A Review. Dent Mater. 2010;26:e171-80.
13. Elias C, Henriques F. Effect Of Thermocycling On The Tensile And Shear Bond Strengths Of Three Soft Liners To A Denture Base Resin. J Appl Oral Sci. 2007;15:18-23.
14. Salim N, Moore C, Silikas N, Satterthwaite J, Rautemaa R. Fungicidal Amounts Of Antifungals Are Released From Impregnated Denture Lining Material For Up To 28 Days. J Dent.2012;40:506-12.
15. Amin W, Al-Ali M, Salim N, Al-Tarawneh S. A New Form Of Intraoral Delivery Of Antifungal Drugs For The Treatment Of Denture-Induced Oral Candidosis. Eur J Dent. 2009;3:257-66.
16. Ryalat S, Darwish R, Amin W. New Form Of Administering Chlorhexidine For Treatment Of Denture-Induced Stomatitis. Ther Clin Risk Manag. 2011;7:219-25.
17. Boscato N, Radavelli A, Faccio D, Loguercio A. Biofilm Formation Of Candida albicans On The Surface Of A Soft Denture-Lining Material. Gerodontology. 2009;26:210-3.
18. Patel M, Cruchley A, Coleman D, Swai H, Braden M, Williams D. A Polymeric System For The Intra-Oral Delivery Of An Anti-Fungal Agent. Biomaterials. 2001;22:2319-24.
19. Bertolini M, Portela M, Curvelo A, Soares R, Lourenço E, Telles D. Resins-Based Denture Soft Lining Materials Modified By Chlorhexidine Salt Incorporation: An In Vitro Analysis Of Antifungal Activity, Drug Release And Hardness. Dent Mater. 2014;30:793-8.
20. Alcantara C, Macedo A, Gurgel B, Jorge J, Neppelenbroek K, Urban V. Peel Bond Strength Of Resilient Liner Modified By The Addition Of Antimicrobial Agents To Denture Base Acrylic Resin. J Appl Oral Sci. 2012;20:607-12.
21. Gendreau L, Loewy Z. Epidemiology And Etiology Of Denture Stomatitis. J Prosthodont. 2011;20:251-60.
22. da Silva P, Acosta E, Pinto L, Graeff M, Spolidorio D, Almeida R, Porto V. Microscopical Analysis Of Candida albicans Biofilms On Heat-Polymerised Acrylic Resin After Chlorhexidine Gluconate And Sodium Hypochlorite Treatments. Mycoses. 2011;54:712-7.
23. Figueiral M, Fonseca P, Lopes M, Pinto E, Pereira-Leite T, Sampaio-Maia B. Effect Of Denture-Related Stomatitis Fluconazole Treatment On Oral Candida albicans Susceptibility Profile And Genotypic Variability. Open Dent J. 2015;9:46-51.
24. Marra J, Paleari A, Rodriguez L, Leite A, Pero A, Compagnoni M. Effect Of An Acrylic Resin Combined With An Antimicrobial Polymer On Biofilm Formation. J Appl Oral Sci. 2012;20:643-8.
25. Salim N, Moore C, Silikas N, Satterthwaite J, Rautemaa R. Candidacidal Effect Of Fluconazole And Chlorhexidine Released From Acrylic Polymer. J Antimicrob Chemother. 2013;68:587-92.
26. Salim N, Silikas N, Satterthwaite J, Moore C, Ramage G, Rautemaa R. Chlorhexidine-Impregnated PEM/THFM Polymer Exhibits Superior Activity To Fluconazole-Impregnated Polymer Against Candida albicans Biofilm Formation. Int J Antimicrob Agents. 2013;41:193-6.
27. Salim N, Moore C, Silikas N, Satterthwaite J, Rautemaa R. Chlorhexidine Is A Highly Effective Topical Broad-Spectrum Agent Against Candida spp. Int J Antimicrob Agents. 2013;41:65-9.
28. Bueno M, Urban V, Barbério G, da Silva W, Porto V, Pinto L.Effect Of Antimicrobial Agents Incorporated Into Resilient Denture Relines On The CandiD albicans Biofilm. Oral Dis. 2015;21:57-65.
29. Abbeele A, de Meel H, Ahariz M, Perraudin J, Beyer I, Courtois P. Denture Contamination By Yeasts In The Elderly. Gerodontology. 2008;25:222-8.
30 Marcelino N, Barreiros M, Bettencourt A, Neves C. Efeito da Incorpora��o de Clorexidina Em Resinas de Rebasamento � Estudos de Liberta��o. Rev Port Estomatol Med Dent Cir Maxilofac. 2015;56(S1):14.
31. Sousa C, Costa J, Matos A, Bettencourt A, Portugal J, Neves C. Efeito da Incorpora��o de Clorexidina Nas Propriedades de Resinas Acr�licas De Rebasamento. Rev Port Estomatol Med Dent Cir Maxilofac. 2014;55(S1):e23-4.
32. Rijo I, Pedro D, Costa J, Bettencourt A, Portugal J, Neves C. Chlorhexidine Loading Of Acrylic Reline Resins � Microhardness And Flexural Strength After Thermal Aging. Rev Port Estomatol Med Dent Cir Maxilofac. 2018;59:154-61.
33. Lacerda S, Portugal J, Neves C. Efeito da Incorpora��o de Clorexidina Nas Propriedades Mec�nicas de Resinas de Rebasamento. Rev Port Estomatol Med Dent Cir Maxilofac. 2015;56(S1):e21.
34. Costa J, Alexandre F, Bettencourt A, Ribeiro I, Portugal J, Neves C. Incorporação de Clorexidina Em Resinas de Rebasamento � Estudos Microbiológicos. Rev Port Estomat Med Dent Cir Maxilofacial. 2017;58(S1):e51.
35. Bettencourt A, Feliz M, Sousa C, Goncalves L, Neves C. An Acrylic Reline Resin Loaded With Chlorhexidine: Insights On Drug Release. Rev Port Estomatol Med Dent Cir Maxilofac. 2016;57:125-31.
36. Costa J, Barreiros M, Bettencourt A, Portugal J, Neves C. Effect Of Chlorhexidine Loading On The Surface Free Energy Of Acrylic Reline Resins. Book Of Abstracts. 3rd Meeting Of The CQUL (3ECQUL) 2018:52, Abstract Mat.P7.
37. Costa J, Barreiros M, Bettencourt A, Portugal J, Neves C. Loading Of Acrylic Reline Resins With Chlorhexidine � Evaluation Of A Physical Property. Book Of Abstracts. 10th iMed.ULisboa & 3rd i3DU Postgraduate Students Meeting 2018:123.
38. Jepson N, McGill J, McCabe J. Influence Of Dietary Simulating Solvents On The Viscoelasticity Of Temporary Soft Lining Materials. J Prosthet Dent. 2000;83:25-31.
39. da Silva P, Barragan G, Chasqueira F, Oliveira S, Portugal J. Efeito Do Envelhecimento Em �cido Cítrico Na Microdureza E Resistência � Flexão de Resinas Compostas. Rev Port Estomatol Med Dent Cir Maxilofac. 2012;53:227-32.
40. Preetha A, Banerjee R. Comparison Of Artificial Saliva Substitutes. Trends Biomater. Artif. Organs. 2005;18:178-86.
41. Arima T, Murata H, Hamada T. Properties Of Highly Cross-Linked Autopolymerizing Reline Acrylic Resins. J Prosthet Dent. 1995;73:55-9.
42. Arima T, Murata H, Hamada T. Analysis Of Composition And Structure Of Hard Autopolymerizing Reline Resins. J Oral Rehabil. 1996;23:346-52.
43. Turssi C, Hara A, Serra M, Junior A. Effect Of Storage Media Upon The Surface Micromorphology Or Resin-Based Restorative Materials. J Oral Rehab. 2002;29:864-71.
44. da Mata A, Marques D, Silveira J, Marques J, Felino E, Guilherme N. Effects Of Gustatory Stimulants Of Salivary rev port estomatol med dent cir maxilofac . 2019;60(3) :104-110 109 Secretion On Salivary pH And Flow: A Randomized Controlled Trial. Oral Dis. 2009;15:220-8.
45. Anusavice K, Zhang N, Shen C. Controlled Release Of Chlorhexidine From UDMA�TEGDMA Resin. J Dent Res. 2006;85:950-4.
46. Hiraishi N, Yiu C, King N, Tay F, Pashley D. Chlorhexidine Release And Water Sorption Characteristics Of Chlorhexidine-Incorporated Hydrophobic/Hydrophilic Resins. Dent Mater. 2008;24:1391-9.
47. Cunha T, Regis R, Bonatti M, De Souza R. Influence Of Incorporation Of Fluoroalkyl Methacrylates On Roughness And Flexural Strength Of A Denture Base Acrylic Resin. J Appl Oral Sci. 2009;17:103-7.
48. Casemiro L, Martins C, Pires-De-Souza F, Panzeri H. Antimicrobial And Mechanical Properties Of Acrylic Resins With Incorporated Silver-Zinc Zeolite � Part I. Gerodontology. 2008;25:187-94.
49. Regis R, Zanini A, Vecchia M, Silva-Lovato C, Paranhos H, de Souza R. Physical Properties Of An Acrylic Resin After Incorporation Of An Antimicrobial Monomer. J Prosthodont. 2011;20:372-9.
50. Rodriguez L, Paleari A, Giro G, Junior N, Pero A, Compagnoni M. Chemical Characterization And Flexural Strength Of A Denture Base Acrylic Resin With Monomer 2-Tert-Butylaminoethyl Methacrylate. J Prosthodont. 2013;22:292-7.
51. Acosta-Torres L, Mendieta I, Nuñez-Anita R, Cajero-Juárez M, Castaño V. Cytocompatible Antifungal Acrylic Resin Containing Silver Nanoparticles For Dentures. Int J Nanomedicine. 2012;7:4777�86.
52. Addy M, Handley R. The Effects Of The Incorporation Of Chlorhexidine Acetate On Some Physical Properties Of Polymerized And Plasticized Acrylics. J Oral Rehabil. 1981;8:155-63.
53. Jagger R. Effect Of The Curing Cycle On Some Properties Of A Polymethylmethacrylate Denture Base Material. J Oral Rehabil. 1978;5:151-7.
54. Shibata T, Hamada N, Kimoto K, Sawada T, Sawada T, Kumada H, Umemoto T, Toyoda M. Antifungal Effect Of Acrylic Resin Containing Apatite-Coated TiO2 Photocatalyst. Dent Mater J. 2007;26:437-44.
�
Cristina Bettencourt Neves
E-mail address: cristina.neves@fmd.ulisboa.pt
�
Acknowledgments
The authors thank VOCO GmbH for providing the Ufi Gel Hard evaluated in this study.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 9 August 2019
Accepted 30 September 2019
Available online 22 October 2019
