
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (3) | 145-153
Original research
Partial recording protocols performance on the assessment of periodontitis severity and extent: bias magnitudes, sensibility, and specificity
Protocolos parciais periodontais na avaliação da gravidade e extensão da periodontite: magnitude de viés, sensibilidade e especificidade
a Clinical Research Unit (CRU), Centro de Investigação Interdisciplinar Egas Moniz (CiiEM), Instituto Universitário Egas Moniz, Almada, Portugal
Vanessa Machado - vmachado@egasmoniz.edu.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 3
Original research
Pages - 145-153
Go to Volume
Article History
Received on 05/09/2018
Accepted on 25/10/2018
Available Online on 29/10/2018
Keywords
Original research
�
Partial recording protocols performance on the assessment of periodontitis severity and extent: bias magnitudes, sensibility, and specificity
Protocolos parciais periodontais na avalia��o da gravidade e extens�o da periodontite: magnitude de vi�s, sensibilidade e especificidade
�
Vanessa Machado*, Jo�o Botelho, Paulo Mascarenhas, Maria Alzira Cavacas, Ricardo Alves, Jos� Jo�o Mendes
Clinical Research Unit (CRU), Centro de Investiga��o Interdisciplinar Egas Moniz (CiiEM), Instituto Universit�rio Egas Moniz, Almada, Portugal
�
�
http://doi.org/10.24873/j.rpemd.2018.11.239
�
Abstract
Objectives: This study aimed to assess bias magnitudes, sensibility, and specificity of particular partial-mouth recording protocols (PRPs) to estimate periodontal clinical measurements and periodontal status.
Methods: Estimates of mean clinical attachment loss (MCAL) and mean probing depth (MPD) were calculated for 15 different PRPs and were compared to full-mouth recording protocol (FRP) data from 402 Portuguese. Biases, relative biases and intra-class correlations for all PRPs were evaluated. Bland�Altman plots and Receiver Operating Characteristic / Area Under the Curve (ROC/AUC) analysis were used to assess the sensitivity and specificity for each PRP periodontal diagnosis.
Results: Regarding MPD, Half RD6 UR/LL and RD6 UL/LR had the lowest bias observed with 0.00 mm (-0.22% and 0.22%, respectively) and all full-mouth PRPs significantly produce an underestimation. Concerning MCAL, the Half MB-B-DL UR/LR had the lowest bias observed with 0.01 mm (0.16%). Excluding CPITN, Full-Mouth PRPs outperforms in average Half Mouth PRPs correlations. The Half RD6 UR/LL had the highest AUC (0.96) with 95.5 and 97.1% of sensitivity and specificity, respectively.
Conclusions: Three half-mouth PRPs (Half MB-B-DL UR/LR, Half RD6 UR/LL and Half RD6 UL/LR) protocols can be used to estimate periodontal clinical measurements with limited bias, and high sensitivity, specificity, and concordance. All full-mouth PRPs failed to estimate pocket depth means, and for clinical attachment loss, they present less ability then half-mouth partial protocols, despite presenting high sensitivity levels.
Keywords: Bias, Epidemiology, Periodontal attachment loss, Periodontal index, Periodontal pocket, Prevalence
�
Resumo
Objetivos: Este estudo teve como objetivo avaliar as grandezas de vi�s, sensibilidade e especificidade de protocolos parciais de registo parcial (PRPs) para estimar as medi��es de sondagens e de perda de inser��o cl�nica.
M�todos: A estimativas de perda m�dia de inser��o cl�nica (MCAL) e profundidade m�dia de sondagem (MPD) foram calculadas para 15 PRPs diferentes e comparadas com dados de protocolo periodontal de registo total (FRP) de 402 portugueses doentes periodontais. Foram avaliadas a magnitude de vieses, vieses relativos e correla��es intraclasses para todos os PRPs. A an�lise por gr�ficos de Bland � Altman e de Receiver Operating Characteristic / �rea Under the Curve (ROC / AUC) avaliou a sensibilidade e especificidade para cada PRP.
Resultados: Em rela��o ao MPD, os protocolos RD6 UR / LL e RD6 UL / LR tiveram o menor vi�s observado com 0,00 mm (-0,22% e 0,22%, respectivamente) e todos os PRPs de boca-total produziram uma subestima��o. Em rela��o ao MCAL, o meio MB-B-DL UR / LR apresentou o menor vi�s observado com 0,01 mm (0,16%). Excluindo CPITN, os PRPs totais superam em m�dia as correla��es de PRPs parciais. O PRP parcial RD6 UR / LL teve a maior AUC (0,96) com 95,5 e 97,1% de sensibilidade e especificidade, respetivamente.
Conclus�es: Tr�s PRPs parciais (MB-B-DL UR / LR, RD6 UR / LL eRD6 UL / LR) podem ser usados para estimar medidas cl�nicas periodontais com vi�s limitado e alta sensibilidade, especificidade e concord�ncia. Todos os PRP totais falharam em estimar as m�dias da profundidade da bolsa e perda da inser��o cl�nica, apesar de apresentarem altos n�veis de sensibilidade.
Palavras-chave: Vi�s, Epidemiologia, Perda de inser��o periodontal, �ndice periodontal, Bolsa periodontal, Preval�ncia
�
Introduction
Periodontal diseases are a crucial dental public health problem, since it is the sixth most prevalent disease worldwide and have increased by 57% over the last two decades. 1 - 5
Periodontitis was recently defined as a microbially‑associated and host‑mediated inflammation that results in loss of periodontal attachment.6
Further, periodontal diagnosis is mandatory to determine the severity and extent of periodontitis and demands a thorough anamnesis for the assessment of known risk factors.5
Currently, in periodontal clinical practice and research, the gold standard method for assessing periodontal status is a full‑mouth recording protocol (FRP), where six sites per tooth are probed, possibly involving to at least 168 sites within each person (excluding third molars). However, in periodontal diseases� studies at a large scale, FRP consumes time and is demanding for the patients and examiners, possibly leading to dropout rates and measurement errors. 7, 8
A partial‑ recording protocol (PRP) is a representative clinical set of the patient,9 and is preferred to estimate large scale studies� periodontal status in circumstances of budget limit and time restriction.10 In past epidemiological studies of periodontal disease, some PRPs have been proposed, although such protocols may be unsuitable to assess properly the level and pattern of periodontal disease. Among the proposed PRPs are the community periodontal index of treatment needs (CPITN) or a set‑based teeth and/or sites as the National Health and Nutrition Examination Survey (NHANES) III and IV protocols.11
Since 1972, several articles have compared the performance of PRPs. 12, 13 In most studies, PRPs revealed divergent upshots in periodontitis diagnosis, although other PRPs had insignificant biases for forecasts of periodontal disease severity8 and extent.7 It has been shown that the use of PRPs showed varying degrees of underestimation of disease prevalence. 11, 14, 15 Thus, there is no literature consensus on a PRP that should be employed in epidemiological studies. 16 - 18
It is essential to standardize the method for assessing the prevalence, severity, and extent of the disease in epidemiological studies to be comparable.
For instance, a previous study8 focused on eight PRPs and have concluded that assessing three specific sites per tooth (mesiobuccal, buccal and distolingual) had a minimal bias in estimating disease severity with elevated sensitivity for disease prevalence estimation. Nevertheless, the authors raised the need for more convenience‑based databases to establish PRPs� bias levels or bounds.8
Thereby, this study aimed to estimate the bias and precision associated with probing depth (PD) and clinical attachment loss (CAL) measurements (taken as estimates of periodontitis prevalence, severity, and extent) obtained from PRP methods against the �gold standard� FRP protocol, in a referenced Portuguese population suffering from periodontitis.
Materials and Methods
The data analyzed in this study was sourced from a previous ethically approved research19 (Egas Moniz Ethics Committee authorization number 595). This retrospective study analyzed data from 405 periodontal patients, before periodontal treatment, from the database of the Periodontology Department of the Egas Moniz Dental Clinic.
Regarding the periodontal measures, in the previous study,19 it was performed a circumferential full‑mouth recording protocol (FRP) using CDC/AAP full‑mouth methodology.1
All permanent fully erupted teeth were observed, and third molars, implants, and retained roots were excluded. For this study the following parameters were included: probing depth (PD), gingival recession (REC) and clinical attachment loss (CAL). PD stood for the distance between the cementoenamel junction (CEJ) and the bottom of the pocket, and REC the distance from the gingival margin to the CEJ. If the gingival margin was above the CEJ, REC received negative values. The algebraic sum of PD and REC represented CAL. A CP‑12 SE probe was used for this periodontal assessment (Hu‑Friedy, Chicago, IL, USA).
Concerning the periodontal estimates using the PRP, three of the 405 original patients were excluded due to having 2, 3, and 5 teeth in one quadrant, respectively. The PD and CAL data from the FRP were defined as the �gold‑standard� and were compared with several half and full‑mouth PRP methodologies.
The selected half‑mouth PRPs were: (i) NHANES III (MB‑B measurements) in upper and lower right quadrants (UR/LR); (ii) NHANES III in upper and lower left quadrants (UL/LL); (iii) HANES III (MB‑B‑DB measurements) in UR/LR; (iv) NHANES IV in UL/LL; (v) MB‑B‑DL measurements in UR/LR; (vi) MB‑B‑DL measurements in UL/LL; (vii) 6‑sites (MB‑B‑DB‑ML‑L‑DL) in UR/LR; (viii) 6‑sites in UL/LL; (ix) 6‑sites in UR/LL; (x) 6‑sites in UL/LR. Regarding full‑mouth PRPs we selected: (xi) 6‑sites on ��Ramfjord�� teeth � right maxillary first molar, left maxillary central incisor, left maxillary first premolar, left mandibular first molar, right mandibular central incisor and right mandibular first premolar; (xii) MB�B measurements in all teeth; (xiii) MB�B�DB measurements in all teeth; (xiv) MB�B�DL measurements in all teeth; (xv) 6‑sites on Community Periodontal Index of Treatment Needs (CPITN) teeth � right maxillary first and second molar, right maxillary central incisor, left maxillary first and second molar, left mandibular first and second molar, left mandibular central incisor and right mandibular first and second molar.
Data analyses were completed with IBM SPSS Statistics version 24.0 for Windows (Armonk, NY: IBM Corp.). FRP, partial and full‑mouth PRPs data were presented as mean, standard deviation and standard error for PD, CAL and tooth sites with specified disease severity (PD ≥4 or ≥6 mm, CAL ≥4 or ≥6 mm).
The proportion of sites with unsound depths within specified disease threshold (PD ≥4 to ≥7 mm, CAL ≥4 to ≥7 mm) represented the prevalence of disease. FRP and PRPs� means across disease severity groups were compared through a paired t‑test.
Evaluation of PRPs bias against FRP was made upon patient level summary measures of MPD (Mean Probing Depth) and MCAL (Mean Clinical Attachment Loss) across all 402 subjects in the sample. Bias was defined as the difference between the mean PRP and the mean �gold standard� FPR, for each subjects� PRP, 8, 17, 18 i.e., [bias (PRP) = PRP (mean) � FRP (mean)].
Relative bias, for each PRP, was computed as the percentage of the bias divided by the FRP average score, 8, 17, 18, i.e., [relative bias (PRP) = 100 x bias (PRP) / FRP].
The discrepancy of partial‑mouth assessment (PMA) was expressed as the following ratio: (FRP mean � PRP mean)/FRP mean. Discrepancy positive outcome was considered underestimation, whereas a negative outcome was considered overestimation.
PRP reliability was evaluated through the Intraclass Correlation Coefficients (ICC) who expressed the agreement between FRP and PRP assessments. The degree of correlation between FRP and PRPs was expressed as the Pearson correlation coefficient. A p‑value <0.05 was defined as statistically significant.
Bland�Altman plots (20, 21) were used to investigate and assess the agreement between the PRP and gold standard FRP mean, by studying the mean difference and outlining limits of agreement. The statistical limits were calculated through mean and the standard deviation of the differences amid PRP and gold standard FRP. The resulting graph is an XY scatter plot, in which Y‑axis shows the differences between PRP and FRP and X‑axis represents the average of the two measures. As recommended, 95% confidence interval was added into the plots.21
Logistic regression analyses output were used to estimate accuracy and the probability of concordance between FRP‑based and each tested PRP‑based periodontal disease diagnosis.
An FRP‑based periodontal disease status (present/absent) was the binary dependent variable (CAL > 3.0 as cutoff), and as an independent factor, each tested PRP‑based periodontal disease status binary output (same conditions). For each logistic model, potential covariates (sex, age, and the number of missing teeth) contribution for model fitness were hierarchically assessed, and if turned out redundant covariates were removed from the final model. Receiver Operating Characteristic / Area Under the Curve (ROC/AUC) with 95% confidence intervals at threshold p=0.5 were used to estimate concordance, sensitivity, and specificity for each tested PRP outcome against the gold standard FRP. A p‑value <0.05 was defined as statistically significant.
Results
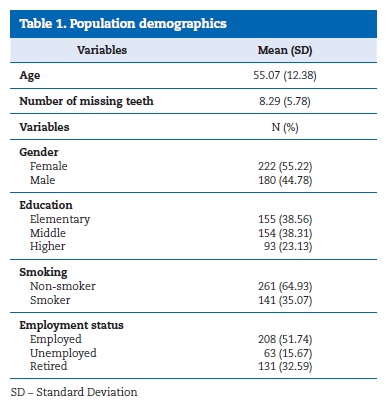
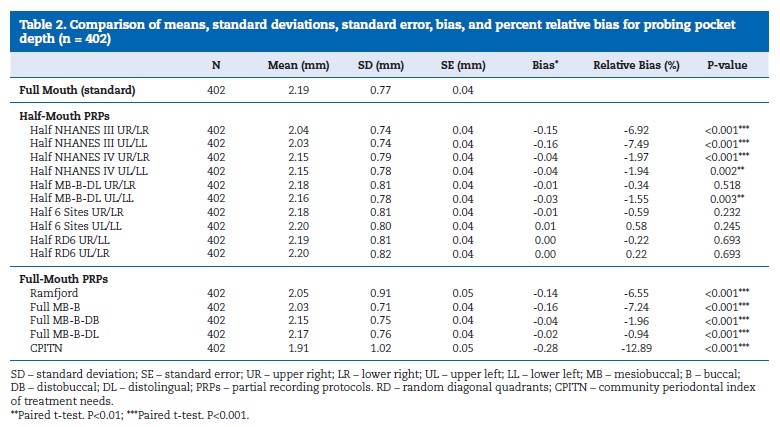
Table 1 describes the population demographics of the Portuguese sample that hampered this study. A summary for the MPD estimates for each PRP is presented in Table 2, and the �gold standard� FRP was 2.19 mm (�0.77) for this study population.
�
�
�
All multi‑site PRPs had an MPD absolute bias lower than 0.1 mm. The respective relative biases ranged from ‑ 12.89% to 0.58%. The bias (relative bias) for the NHANES III IV half‑mouth PRPs ranged between ‑ 0.16 mm (‑7.49%) and ‑0.04 mm (‑0.34%), identical to their full‑mouth forms [‑0.16 mm (‑7.24%) and ‑0.04 mm (‑1.96%)], respectively. The bias and relative biases for the Half 6 sites diagonal (UR/LL and UL/LR) PRP‑based MPD are much smaller, 0.00 mm (‑0.22% and 0.22%, respectively) for both partial‑mouth versions. The MPD estimate based on the Ramfjord PRP had ‑0.14 mm (‑6.55%) negative bias. There were no statistically significant biases for five half‑mouth PRPs (Half MB‑B‑DL UR/LR, Half 6 Sites UR/LR, Half 6 Sites UL/LL, Half 6 Sites UR/LL, and Half 6 Sites UL/LR). All full‑mouth PRPs showed a statistically significant underestimation of the �gold standard� FRP.
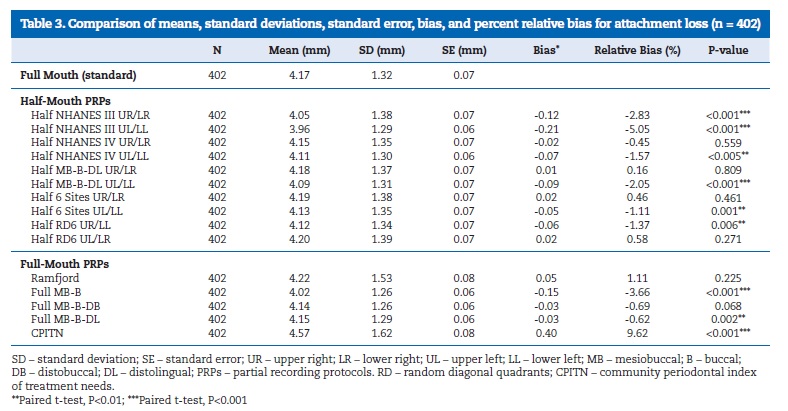
Table 3 presents mean scores and standard deviations of all recording protocols, besides it has bias and percent relative bias (scores further from zero indicate more relative bias) of each PRP compared to FRP (standard). The true full‑mouth mean clinical attachment loss (MCAL) was 4.17 mm (� 1.32) for this study population. Biases for partial mouth PRPs MCAL estimates were all less than 0.02 mm, and the associated relative biases ranged between ‑ 5.05% and 9.62%. Further, CPITN relative biases were the highest of all PRPs both in MPD and MCAL. MCAL biases (relative biases) for NHANES III and NHANES IV half‑mouth PRPs ranged between ‑ 0.21 mm (‑ 5.05%) and ‑0.02 mm (‑ 0.45%) away from their corresponding full‑mouth versions, who were ‑0.15 mm (‑3.66%) and ‑0.03 mm (‑0.69%), respectively. The Half MB‑B‑DL UR/LR had the lowest bias observed with 0.01 mm (0.16%), and the bias for its homologous full‑mouth estimate was ‑0.03 mm (‑ 0.62%).
�
�
The MCAL estimate based on the Ramfjord PRP had 0.05 mm (1.11%) positive bias. There were no significant biases for four half‑mouth PRPs (NHANES IV UR/LR, MB‑B‑DL UR/LR, 6 Sites UR/LR, and 6 Sites UL/LR) and two full‑mouth PRPs (Ramfjord and MB‑B‑DB).
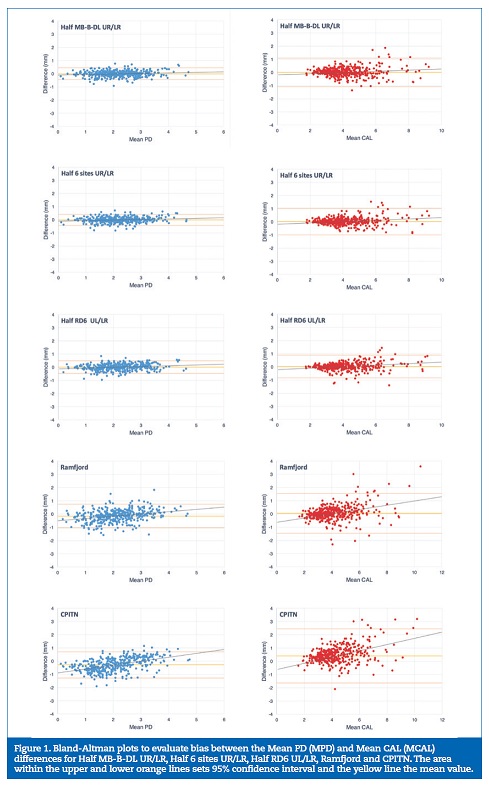
The extent and severity of different thresholds of PD and CAL are presented in Supplements S1‑S8. Figure 1 represents Bland�Altman plots for the half‑mouth versions of NHANES III (UR/LR and UL/LL), NHANES IV (UR/LR and UL/LL), MB�B�DL (UR/LR and UL/LL) and six‑site (UR/LR, UL/LL, UR/LL, and UL/LR) PRPs. The SDs for the MPD scores were higher than the respective mean values (ranged from 0.08 in full‑mouth MB‑B‑DL to 0.51 in CPITN). In the CPITN and Ramfjord PRPs, there were substantial variations among subject‑specific MPD differences compared with those for the MB�B�DL full‑mouth PRPs. The SDs for the MPD scores were slightly larger than the associated means (ranged from 0.22 in half six‑ sites UL/LL and UR/LR to 0.28 in NHANES III UR/LR and NHANES IV UL/LL). The SDs for the MCAL scores were slightly larger than the associated means (from 0.16 in full‑mouth MB‑B‑DL to 1.05 in CPITN). In the CPITN and Ramfjord PRPs, there were substantial variations among subject‑specific MCAL differences compared with MB�B�DL full‑mouth PRPs results. The remaining Bland�Altman plots for MPD and MCAL are as Supplements S9-10.
�
�
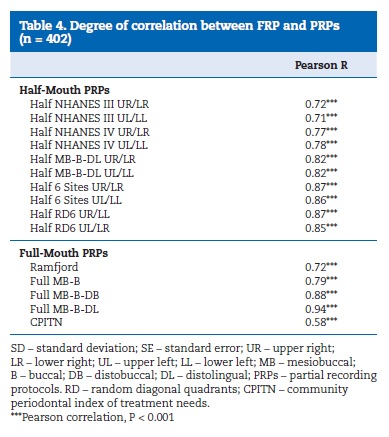
Table 4 shows the Pearson�s correlation as a measure of the relationship between FRP and PRPs MCAL values. In general, all correlations shown in this table are quite high, being indicative of strong relationships. Excluding CPITN, Full‑Mouth PRPs outperforms in average Partial Mouth PRPs correlations.
�
�
Furthermore, the highest correlation was 0.94 for Full MB‑B‑DL and the lowest 0.58 for CPITN.
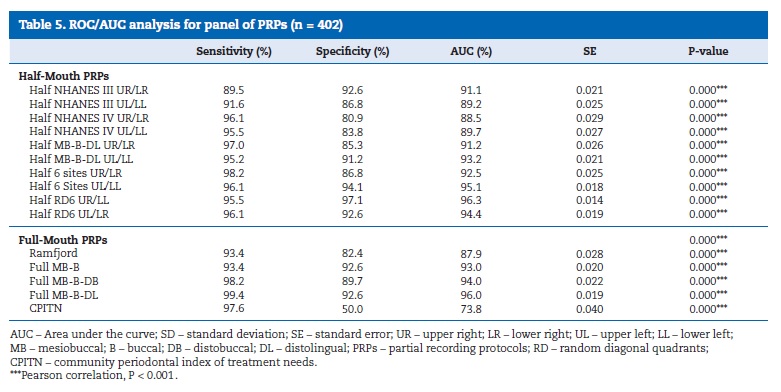
The ROC/AUC values obtained from the logistic analysis ranged between 73.8% for CPITN and 96.3% for Half RD6 UR/LL (p<0.0001). There was no significant improvement in sensitivity and specificity when sex, age, and the number of missing teeth covariables were hierarchically added to the logistic model (Supplement S11).
Table 5 shows the corresponding sensitivity of PRPs in sensing clinical attachment loss distributions. All PRPs had high sensitivity for mean CAL > 3 mm. The MB‑B‑DL full‑mouth PRP was the only to achieved 99% sensitivity. There was a decrease in sensitivity, although the half MB‑B‑DL UR/LR, half 6 sites UR/LR, MB‑B‑DB full‑mouth protocol maintained reasonably high sensitivity. In contrast, NHANES III PRPs showed the lowest sensitivity values.
�
�
On the other hand, most of PRPs had high specificity for mean attachment loss > 3 mm. The half RD6 UR/LL was the only partial recording protocol that achieved a specificity of at least 97%. In opposition, the CPITN and Ramfjord protocols had the smallest specificity (50% and 82.4%, respectively).
Discussion
The balance of advantages and disadvantages of PRPs, in the assessment of the prevalence and severity of periodontal disease in epidemiologic research, needs to be carefully evaluated.
In large‑scale surveys, time and resource demanding are the primary considerations and usually mandates the use of a partial‑mouth periodontal examination. 7, 8, 17, 22 The prevalence and severity of estimated periodontal disease produced by these PRPs are necessarily biased. 8, 23 However, their bias magnitude depends on the group of teeth/sites examined, and prevalence of the disease in that particular population. 8, 10, 24
An important strength of this study is the access to full‑mouth periodontal examination sourced from a large‑scale population‑based study, with a considerable variation in chronic periodontitis severity. This database allowed to investigate the effects of specific PRPs in estimating the prevalence and severity of periodontal disease with bias and relative bias.
Moreover, in assessing the usefulness of different PRPs diagnostic methods, both the sensitivity and specificity are essential criteria and must be taken into consideration when selecting a suitable system. Comparatively, the disease severity in this Portuguese study population was substantially higher (full‑mouth MCAL=4.17 mm and MPD=2.19 mm) than that before reported, 25 - 26 in Guatemalan and American populations, respectively.
A previous study25 (25) reported similar findings for the half random diagonal six‑site PRP (full‑mouth MCAL=2.76 mm and full‑mouth MPD=2.88 mm). In contrast, in the US multicentric study of Beck et al.,26 NHANES III, NHANES IV and Ramfjord PRPs have shown higher relative bias for MPD and MCAL (MCAL=1.77 mm and MPD=1.89 mm) comparing with our study. The mouth characteristics of each population and their demographics may explain these contradictory findings. 26 - 27
The NHANES III and IV protocols randomly select one upper quadrant and one lower quadrant at the same side and involve three fixed buccal sites per tooth (MB�B� DB).28 In this study, we decided to appraise both two random options separately (one upper and one lower) to investigate the effect of the quadrants random selection. The current study has indicated that when used in an epidemiological survey, both NHANES III and IV lead to an underestimate of the MCAL and MPD. Also, the half NHANES IV UR/LR was the only one that did not have statistically significant differences with the gold‑standard full‑mouth examination and had the highest sensitivity (96.1%).
Numerous authors have used Ramfjord teeth for evaluating periodontal status, and the results have been acceptable and representative of FME. 26, 29 In contrast, other investigators 8, 30, 31 8,30,31 have reported that examination of the Ramfjord teeth is not suitable for evaluating the extension, degree, or prevalence of both PD or CAL. In fact, a study 30 has verified that Ramfjord Teeth are an inadequate surrogate for epidemiologic studies of periodontitis. This limitation of the Ramfjord teeth also becomes evident in our research, since Ramfjord PRP produces one of the more substantial biases for estimating MPD, and, in Bland�Altman plots, there were significant variations among subject‑specific in both MCAL and MPD.
The current study demonstrates that partial and full‑mouth PRPs underestimated MPD and MCAL. This investigation identified three potential PRPs that better estimated the MPD and MCAL standard values: (1) Half MB‑B‑DL UR/LR, (2) Half 6 sites UL/LR, and (3) Half RD 6 UL/LR. These results are following previous findings. 17 Furthermore, all full‑mouth PRPs presented significant different results for MPD, and CPITN was the protocol that had higher bias and relative bias results of all PRPs (‑0.28 and ‑12,89%, respectively). Whereas concerning MCAL, Ramfjord and Full MB‑B‑DB did not have statistically different results from the standard, and once again, CPITN had the higher bias and relative bias results (0.40 and 9,62%, respectively). These results comport with previous studies that have highlighted the biasing potential of CPITN in epidemiological surveys. 17, 32 Moreover, our results reveal a significant reduction in bias and high sensitivity for periodontal disease severity when using the half‑mouth MB�B�DL UR/LR PRP, and this has been previously reported for a Brazilian population. 23
Notwithstanding, regarding the extent and severity of different thresholds of PD and CAL, PRPs tend to fail when the established threshold is low. About the extent of PD, the Ramfjord PRP was the only protocol that was consistent with gold standard values in all considered thresholds. Concerning CAL extent, Half NHANES IV UR/LR was the protocol that better estimated the extent of attachment loss of the respective standard value. Besides, only one study has addressed this comparison with other variables like age and gender. 18 This is the first time that is assessed the potential bias of PRPs on the extent and severity of periodontal disease. The extent and severity are elements of extreme importance since they have long been used as a critical descriptor of periodontitis cases,6 and remain highly relevant in the most recent World Workshop Consensus Report of the 2017. 6, 33
With these being said, there is a lack of agreement on which PRP should be used in epidemiological surveys. Hereupon and considering the possible effect of the characteristics of each population, as previously mentioned, it has been proposed to perform an FMP on a randomly selected subsample of the subjects (5 to 10%) to calculate the degree of bias of the proposed partial protocol. In the future, to apply this method in population surveys, there is the need to appraise the epidemiological impact on the periodontal estimates.8
Conclusion
Our findings suggest that a half‑mouth three sites and two half‑mouth six sites protocols can be used to estimate periodontal clinical measurements and status in Portuguese patients with limited bias. Also, these protocols showed high sensitivity, specificity, and concordance. Nevertheless, although all full‑mouth partial protocols had high sensitivity levels, they all failed to estimate pocket depth and clinical attachment loss means, presenting less ability then half‑mouth partial protocols.
�
References
1. Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of Periodontitis in Adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914-20.
2. Petersen PE, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 2000. 2012;60:15-39.
3. Kassebaum NJ, Bernab� E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global Burden of Severe Periodontitis in 1990-2010. J Dent Res. 2014;93:1045-53.
4. Jin LJ, Lamster IB, Greenspan JS, Pitts NB, Scully C, Warnakulasuriya S. Global burden of oral diseases: emerging concepts, management and interplay with systemic health. Oral Dis. 2016;22:609-19.
5. Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017;44:45662.
6. Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis : Framework and proposal of a new classification and case definition. J Clin Periodontol. 2018 Jun;45 Suppl 20:S149-S161.
7. Owens JD, Dowsett SA, Eckert GJ, Zero DT, Kowolik MJ. Partial-mouth assessment of periodontal disease in an adult population of the United States. J Periodontol. 2003;74:1206-13.
8. Kingman A, Susin C, Albandar JM. Effect of partial recording protocols on severity estimates of periodontal disease. J Clin Periodontol. 2008;35:659-67.
9. Ramfjord SP. Indices for Prevalence and Incidence of Periodontal Disease. J Periodontol. 1959;30:51-9.
10. Kingman A, Albandar J. Methodological aspects of epidemiological studies of periodontal disease. Periodontol 2000. 2002;29:11-30.
11. Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA. Accuracy of NHANES periodontal examination protocols. J Dent Res. 2010;89:1208-13.
12. Downer MC. The relative efficiencies of some periodontal partical recording selections. J Periodontal Res. 1972;7:334-40.
13. Leroy R, Eaton KA, Savage A. Methodological issues in epidemiological studies of periodontitis � how can it be improved? BMC Oral Health. 2010;10:8.
14. Dalla Vecchia CF, Susin C, Ro CK, Oppermann RV, Albandar JM. Overweight and Obesity as Risk Indicators for Periodontitis in Adults. J Periodontol. 2005;76:1721-8.
15. Vettore MV, Lamarca G de A, Le�o ATT, Sheiham A, Leal M do C. Partial recording protocols for periodontal disease assessment in epidemiological surveys. Cad Saude Publica. 2007;23:33-42.
16. Figueiredo A, Soares S, Lopes H, Dos Santos JN, Ramalho LMP, Cangussu MC, et al. Destructive periodontal disease in adult Indians from Northeast Brazil: Cross-sectional study of prevalence and risk indicators. J Clin Periodontol. 2013;40:1001-6.
17. Tran DT, Gay I, Du XL, Fu Y, Bebermeyer RD, Neumann AS, et al. Assessing periodontitis in populations: A systematic review of the validity of partial-mouth examination protocols. J Clin Periodontol. 2013;40:1064-71.
18. Tran DT, Gay I, Du XL, Fu Y, Bebermeyer RD, Neumann AS, et al. Assessment of partial-mouth periodontal examination protocols for periodontitis surveillance. J Clin Periodontol. 2014;41:846-52.
19. Machado V, Botelho J, Amaral A, Proen�a L, Alves R, Rua J, et al. Prevalence and extent of chronic periodontitis and its risk factors in a Portuguese subpopulation: a retrospective cross-sectional study and analysis of Clinical Attachment Loss. PeerJ. 2018.
20. Giavarina D. Understanding Bland Altman analysis. Biochem Medica. 2015;25:141-51.
21. Bland JM, Altman DG. Statistical Methods for Assessing Agreement Between Two Methods of Clinical Measurement. Lancet. 1986;327:307-10.
22. Benigeri M, J-m B, Payette M, Charbonneau A. Community periodontal index of treatment needs and prevalence of periodontal conditions. J Clin Periodontol. 2000;27:308-12.
23. Susin C, Kingman A, Albandar JM. Effect of Partial Recording Protocols on Estimates of Prevalence of Periodontal Disease. J Periodontol. 2005;76:262-7.
24. Kingman A, Morrison E, L�e H, Smith J. Systematic errors in estimating prevalence and severity of periodontal disease. J Periodontol. 1988;59:707-13.
25. Dowsett S a, Eckert GJ, Kowolik MJ. The applicability of half-mouth examination to periodontal disease assessment in untreated adult populations. J Periodontol. 2002;73:975-81.
26. Beck JD, Caplan DJ, Preisser JS, Moss K. Reducing the bias of probing depth and attachment level estimates using random partial-mouth recording. Community Dent Oral Epidemiol. 2006;34:1-10.
27. Albandar JM. Underestimation of Periodontitis in NHANES Surveys. J Periodontol. 2011;82:337-41.
28. Dye BA, Thornton-Evans G. A Brief History of National Surveillance Efforts for Periodontal Disease in the United States. J Periodontol. 2007;78:1373-9.
29. Diamanti‐Kipioti A, Papapanou PN, Moraitaki‐Tsami A, Lindhe J, Mitsis F. Comparative estimation of periodontal conditions by means of different index systems. J Clin Periodontol. 1993;20:656-61.
30. Fleiss JL, Park MH, Chilton NW, Alman JE, Feldman RS, Chauncey HH. Representativeness of the �Ramfjord teeth� for epidemiologic studies of gingivitis and periodontitis. Community Dent Oral Epidemiol. 1987;15:221-4.
31. Rams, T.E, Oler J., Listgarten M.A. SJ. Utility of Ranjford index teeth to assess periodontal disease progression in longtudinal studies. J Clin Periodontol. 1993;20:147-50.
32. Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the Case Definitions for Population-Based Surveillance of Periodontitis. J Periodontol. 2012;83:1449-54.
33. Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, et al. Periodontitis : Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri ‐ Implant Diseases and Conditions. J Periodontol. 2018;89 Suppl 1:S173-S182.
�
Vanessa Machado
Correio eletr�nico: vmachado@egasmoniz.edu.pt.
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Appendices
Supplementary content Supplementary data associated with this article can be found, in the online version, at http://doi.org/10.24873/j.rpemd.2018.11.239.
�
Article history:
Received 5 September 2018
Accepted 25 October 2018
Available online 30 November 2018
