
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (2) | 67-74
Original research
Interrelationship between facial pattern, malocclusion, TMDs, head and neck posture and type of breathing in young people
Inter-relação entre padrão facial, má-oclusão, DTM, postura cervical e tipo de respiração em jovens de 12 a 15 anos
a CESPU, Instituto de Investigação e Formação Avançada em Ciências e Tecnologias da Saúde, Gandra, Portugal
b ESS-IPP, Escola Superior de Saúde do Instituto Politécnico do Porto, Porto, Portugal
c IBMC – Instituto Biologia Molecular e Celular, i3S – Inst. Inovação e Investigação em Saúde, Universidade do Porto, Porto, Portugal
Teresa Pinho - teresa.pinho@iucs.cespu.ptteresa.pinho@iucs.cespu.pt
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 2
Original research
Pages - 67-74
Go to Volume
Article History
Received on 02/11/2017
Accepted on 04/08/2018
Available Online on 11/09/2018
Keywords
Original research
�
Interrelationship between facial pattern, malocclusion, TMDs, head and neck posture and type of breathing in young people
Inter-rela��o entre padr�o facial, m�-oclus�o, DTM, postura cervical e tipo de respira��o em jovens de 12 a 15 anos
�
Sara Valinhasa, Maria Pa�oa, Ricardo Santosb, Teresa Pinhoa,c,*
a CESPU, Instituto de Investiga��o e Forma��o Avan�ada em Ci�ncias e Tecnologias da Sa�de, Gandra, Portugal.
b ESS-IPP, Escola Superior de Sa�de do Instituto Polit�cnico do Porto, Porto, Portugal.
c IBMC � Instituto Biologia Molecular e Celular, i3S � Inst. Inova��o e Investiga��o em Sa�de, Universidade do Porto, Porto, Portugal.
�
�
http://doi.org/10.24873/j.rpemd.2018.09.229
�
Abstract
Objectives: To compare occlusal, facial, and craniocervical postural characteristics according to the breathing pattern, study the association between temporomandibular disorders� (TMDs) class and severity, gauge the influence of the breathing pattern, head and neck posture, occlusal class, and facial pattern on TMDs severity and the lower cervicofacial ratio, and identify any prevalent differences in TMDs severity by gender.
Methods: This cross-sectional study included a convenience sample of 139 individuals, 81 females (58.3%) and 58 males (41.7%), with a mean age of 13.0�0.72 years old. Data were collected from observations, medical forms and photographic records. We classified TMDs severity according to Fonseca Anamnestic Index and used Software for Postural Assessment.
Results: Compared to nasal breathers, oral breathers exhibited a predominance of Class II occlusion (p<0.01), a convex profile (p<0.05), increased cervicofacial ratio (p<0.01), and a tendency for head anteriorization (p<0.05). An association between TMDs and individuals with Class II occlusion was also found (p<0.01). Oral breathers showed a greater risk of increased lower cervicofacial ratio and mild TMDs (OR: 9.64 and 4.01, respectively). Signs and symptoms of TMDs appeared in 60% of young females, though the difference between genders was not significant (p=0.290).
Conclusions: We detected associations between oral breathing and head anteriorization, TMDs, Class II malocclusion, convex facial profile, and increased lower cervicofacial ratio. TMDs were associated with occlusal Class II, and oral breathing increased the risk of developing mild TMDs and increased lower cervicofacial ratio.
Keywords: Craniocervical posture, Dental occlusion, Malocclusion, Oral breathing, Temporomandibular disorders
�
Resumo
Objetivos: Comparar as caracter�sticas posturais, oclusais, faciais e craniocervicais de acordo com o padr�o de respira��o; estudar a associa��o entre a classe e a gravidade das DTM; avaliar a influ�ncia do padr�o de respira��o, a postura da cabe�a e do pesco�o, a classe oclusal e o padr�o facial na severidade da DTM e propor��o cervicofacial inferior; e identificar a preval�ncia e gravidade das DTMs por g�nero.
M�todos: Estudo transversal com amostra de conveni�ncia de 139 indiv�duos, 81 do sexo feminino (58,3%) e 58 do sexo masculino (41,7%) com idade m�dia de 13,0�0,72 anos. Os dados foram recolhidos atrav�s de exame cl�nico, formul�rios m�dicos e registos fotogr�ficos. Atrav�s dos sinais e sintomas classificou-se a severidade das DTM de acordo com o �ndice Anamn�sico da Fonseca e o Software usado para a Avalia��o Postural.
Resultados: Comparados os respiradores nasais, aos respiradores orais, estes exibiram predomin�ncia de oclus�o de Classe II (p<0,01), perfil convexo (p<0,05), aumento da rela��o cervicofacial (p<0,01) e tend�ncia de anterioriza��o da cabe�a (p<0,05). Uma associa��o entre DTM e indiv�duos com oclus�o Classe II tamb�m surgiu (p<0,01). Os respiradores orais apresentaram maior risco de aumento da rela��o cervicofacial inferior e DTM moderadas (OR: 9,64 e 4,01, respetivamente). Sinais e sintomas de DTM apareceram em 60% das mulheres jovens, embora a diferen�a entre os sexos n�o tenha sido significativa (p=0,290).
Conclus�es: Foram detetadas associa��es entre respira��o oral e antecipa��o da cabe�a, DTM, m� oclus�o de Classe II, perfil facial convexo e aumento da rela��o cervicofacial mais baixa. As DTM foram associadas � Classe II oclusal e a respira��o oral aumentou o risco de desenvolver DTM leves e aumentou a propor��o cervicofacial mais baixa.
Palavras-chave: Postura craniocervical, Oclus�o dent�ria, M�-oclus�o, Respira��o oral, Disfun��o temporomandibular
�
Introduction
The stomatognathic system involves the teeth, jaws, and associated soft tissues. It is a complex, interconnected system of structures that performs vital body functions, and changes to any of its structures can cause general systemic imbalance. 1, ‑ 10
Research has shown that the overall body posture interferes with the position of the head, which is directly responsible for the position of the jaw and tongue in the oral cavity, and vice versa. 1, 6 ‑ 9
However, the results of several studies on the relationship between malocclusion and abnormal head and neck posture remain ambiguous. 3, 4 On the other hand, other evidence shows that disorders in the stomatognathic system, particularly temporomandibular disorders (TMDs) and malocclusion, can increase the risk of developing postural changes.1 During childhood up to 8 years of age, postural changes are normal; however, after that age, the body adapts and realigns, and such disorders can persist when children breathe through their mouths. 1, 6
Breathing is a vital body function developed at birth. Nasal breathing is associated with normal chewing function, swallowing, and the posture of the tongue and lips, and it also affords proper muscle action and favors the craniofacial development of the midface. However, when certain factors prevent the passage of air through the nasal cavity, the breathing pattern becomes predominantly oral. The persistence of oral breathing during the growth phase can determine several changes beyond the craniofacial region. 2 7 ‑ 9
In fact, research has shown that alterations in craniocervical growth relate to corresponding changes in growth patterns of the facial skeleton,3 as evident in the facial skeletal patterns of oral breathers.
Since the temporomandibular joint (TMJ) relates directly to the cervical and scapular region via a common neuromuscular system, postural changes of the cervical spine can cause disturbances in the TMJ, and vice versa,11 that can result in signs and symptoms of TMDs. As defined by the American Academy of Orofacial Pain, TMDs are a group of musculoskeletal and neuromuscular conditions involving the TMJs, masticatory muscles, and all associated structures in reciprocal interaction and influence.11 Several questionnaires and indexes are available to describe and validate TMDs diagnoses and the severity of their signs and symptoms, including the Helkimo Index, 12, 13 the Fonseca Anamnestic Index, 14 and the Diagnostic Criteria for TMDs developed by the International Research Diagnostic Criteria for TMDs Consortium Network, 15, 16 all of which vary in their ease of application.
Considering all the above, it is important to ascertain which factors can interfere with the stomatognathic system in order to allow early diagnoses of disorders and plan the best interventions accordingly. In this sense, based on a sample of young people with 12 to 15 years old, we aimed to a) compare occlusal, facial, and craniocervical postural characteristics according to the breathing pattern; b) study the association between occlusal class and TMDs severity; c) and estimate the influence of the breathing pattern, head and neck posture, occlusal class and facial pattern on the severity of TMDs and on the lower cervicofacial ratio. Secondarily, we aimed to identify any prevalent differences in TMDs severity by gender, in the selected sample.
Materials and methods
This observational, cross‑sectional, analytical study took place at two Portuguese schools between November 2015 and April 2016, with a convenience sample of 139 individuals (81 females and 58 males) aged from 12 to 15 years (13.0�0.72).
The minimum age was 12 years and the maximum 15 years. The most common age was 13 years (N=76), corresponding to 54% of the sample and the least common was 15 years, in only 2.2% of the sample (N=3).
The inclusion criteria were: the presence of definitive dentition and being aged between 12 and 15 years. The exclusion criteria were: a history of orthodontic treatments, a history of physical therapy treatments related to cervico�craniofacial issues, ears, nose, and throat surgical interventions (e.g., nose, tonsils, adenoids), and the presence of neurological, orthopedic, or craniofacial malformations.
The participants� parents or guardians were informed about the study and its objectives and procedures and asked to sign an informed consent, per the recommendations of the Declaration of Helsinki. The Ethics Committee of the University Institute of Health Sciences (CESPU) approved the study.
Clinical evaluation started with a functional matrix of data from a short questionnaire and clinical observations, followed by the evaluation of occlusion and posture via intraoral clinical examination and photographic analysis. Lastly, a questionnaire on TMDs was administered. 12, 13
Prior to data collection, a pilot study was performed to calculate the average time needed to assess each participant, train the investigators responsible for data collection (S.V.; T.P.) on how to use the assessment protocol, and calculate the reliability of the measurements. The pilot study was conducted in two phases, separated by one week, with a total of 15 participants (46% female) who did not participate in the primary sample but who presented similar characteristics. Inter‑and intraobserver reliability assessed via intraclass correlation coefficients (ICC) were 0.86 and 0.94, respectively, with Angle�s classification and an ICC=0.96 for the identification of landmarks necessary for postural analysis. Those results demonstrated a good reliability of the measurements.
The functional assessments were conducted via four methods:
1. Questions addressed to participants and their parents regarding whether the participant snored at night, drooled during sleep, slept with his or her mouth open, among others;
2. Lip sealing without voluntary muscle contraction; 6, 17
3. A water in the mouth test, which assessed the time that the participant could breathe with sealed lips (normal: ≥2 min),6, 17 to identify nasal breathing difficulty; and
4. A mirror test, which involved placing an intraoral disposable mirror under the nostrils 7, 8, 17 to gauge water vapor formation (normal: mirror fogging).
We identified oral breathing when these assessments� results deviated from the norm. 17 Given the impossibility of conducting complementary ear, nose, and throat tests, we decided to match nasal and oral breathing as indicators of normality and change, respectively. In addition, we applied a supplementary questionnaire and conducted observations to identify any typical features of oral breathers. 2, 5, 7, 8
The dental occlusion was evaluated by analyzing the position of the first permanent molars and the presence of crossbite and open bite according to Angle�s and Moyers�s (1991) classification, respectively. 7, 18 To minimize the possibility of bias, two investigators performed the evaluations.
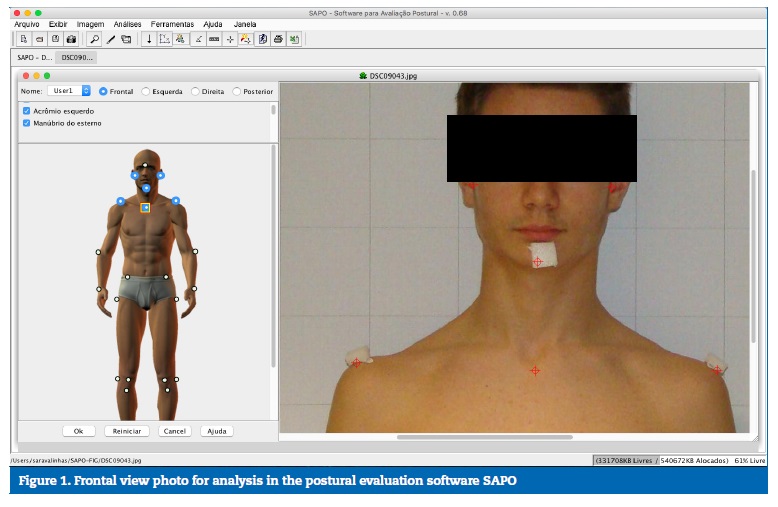
All participants were photographed to evaluate head and neck posture using photogrammetric analysis, with the help of Software for Postural Assessment, version 0.68. A 9x9‑cm checkered screen was used to set image calibration, as well as a Sony� Cyber‑shot camera with 8.1‑megapixel resolution, a tripod with the same calibration parameters, and foam anatomical markers for all participants. Participants were photographed (males without shirts, females with tops) in an orthostatic position. Foam labels and stickers were used to set the anatomical sites for analysis. The camera was placed 1.5 m away from the participant to capture his or her upper body, and three photographs were taken: a frontal view, a right‑side view, and a left‑ side view (Figures 1 and 2).
�
�
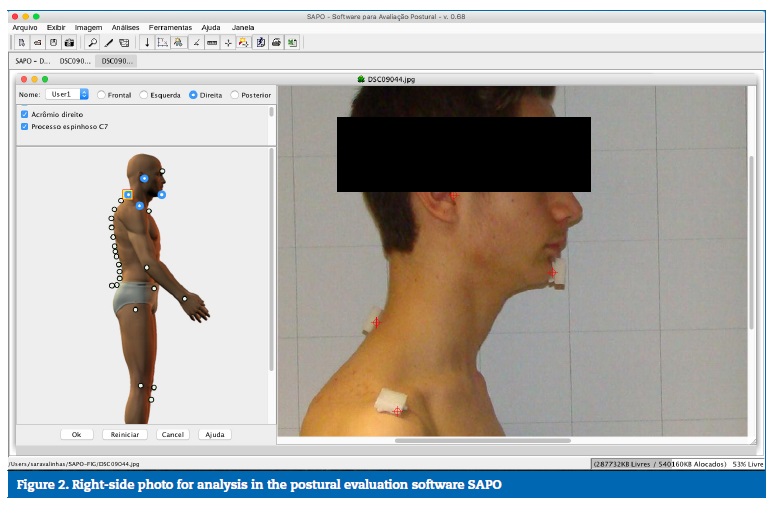
�
The following variables were used: horizontal head and acromion alignment (frontal view), horizontal head alignment (C7), and vertical head alignment with the acromion (sagittal plane), as shown in Figures 1 and 2.
Signs and symptoms of TMDs were classified according to the Fonseca Anamnestic Index developed by Fonseca14 and based on the Helkimo Anamnesis Index.12 This index is recommended for epidemiological studies due to its simplicity, as it includes 10 questions to be answered with �yes� (10 points), �no� (0 points), or �sometimes� (5 points), with only one answer for each question. According to their final scores, we classified participants as having mild TMDs (20�40), moderate TMDs (45�65), severe TMDs (70�100), or being TMDs‑free (0�15).14
The collected data were analyzed with the Statistical Package for the Social Sciences for Macintosh, version 23.0.0.2 (IBM, New York, NY, USA), considering a significance level of 5%. An exploratory study was conducted using descriptive statistics of frequencies, central tendency (mean [M] or median [Med], according to variable distribution), and dispersion (standard deviation [SD] or interquartile range [IR], according to variable distribution). The normal distribution analysis was performed using the Kolmogorov�Smirnov test and Student�s t‑test and Mann-Whitney U Test for variables with normal and non‑normal distribution, respectively.
Proportions were compared using the chi‑square test when conditions for its use were present, and the degree of association was checked using Cramer�s V coefficient. To estimate the influence of the breathing pattern, head and neck posture, occlusal class, and facial pattern on TMDs severity and the lower cervicofacial ratio, we performed a multinomial regression analysis, following the validation of its assumptions.Results
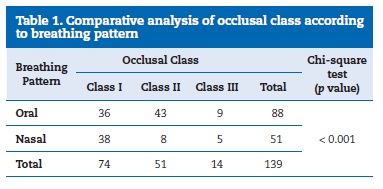
The sample comprised 139 participants aged between 12 to 15 years, with a mean age of 13.0�0.72 years, and most of whom (n=58; 41.7%) were male. The frequency of oral breathing was 63%, and the most frequent occlusal classes were Classes I and II (53% and 37%, respectively).
An increased prevalence of Angle Class II occlusion was found in individuals with oral breathing patterns (p<0.001), with a dependency relationship between the variables (Table 1).
�
�
Convex profiles were predominant in individuals with standard oral breathing, with statistically significant differences (p<0.05), as shown in Table 2.
�
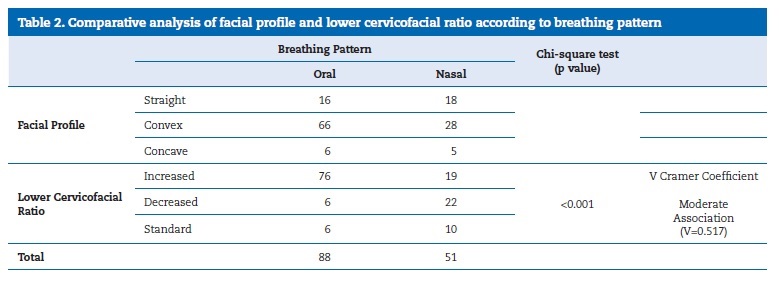
�
Results showed an increased cervicofacial ratio for oral breathers (ratio: 86.3%), which was far greater than for nasal breathers (ratio: 37.2%) to a statistically significant degree (p<0.05).
Our relational study using Cramer�s V coefficient revealed a positive and moderate association (V=0.517), as shown in Table 2.
Results of our comparative analysis of head and neck posture according to breathing pattern are presented in Table 3.
�
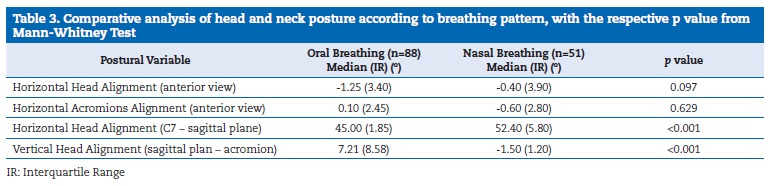
�
Horizontal head alignment: Anterior view
Oral breathers exhibited a predominant tilt of the head to the left and nasal breathers a predominan tilt to the right, with statistically significant differences (p<0.05).
Horizontal acromion alignment: Anterior view
Right shoulder elevation was more pronounced among oral breathers than among nasal breathers, but without any statistically significant differences (p =0.63).
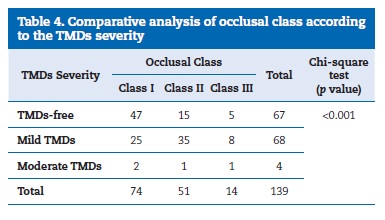
Horizontal head alignment: Sagittal plane to C7 Oral breathers tended to show a forward tilt of the head (<45.�), with statistically significant differences (p<0.05) between groups, yet with lower values in the group of standard oral breathers. Vertical head alignment: Sagittal plane to acromion Oral breathers demonstrated a tendency toward anteriorization in vertical head alignment. Values of vertical head alignment showed a statistically significant difference (p<0.05) between the groups, as the group with an oral breathing pattern had greater, more positive values. Class II occlusion predominated in individuals with mild TMDs (Table 4). Using a chi‑square test to compare Class I and Class II variables in the absence and presence of mild TMDs, we found statistically significant differences (p<0.05) between the groups (Table 4).�
�
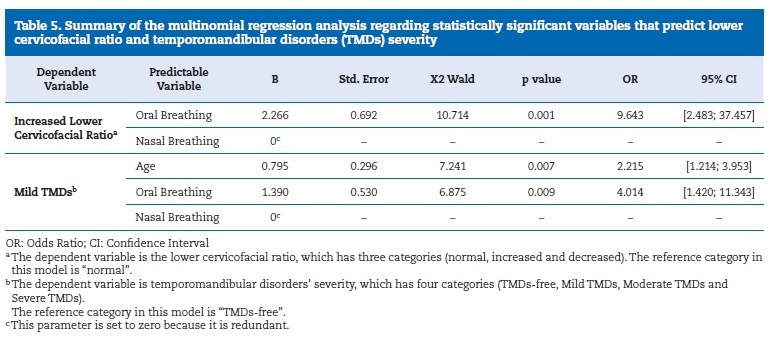
The adjusted model was statistically significant (G2 (24) = 48.317; p<0.01), and statistically significant estimates of coefficients of the model are presented in Table 5. According to the adjusted model, only the breathing pattern significantly influenced an increase in the lower cervicofacial ratio, and the breathing pattern and age significantly influenced the development of mild TMDs. Variables concerning head and neck posture, sex, occlusal class, and facial profile did not influence the results significantly (p>0.05).
Females presented a higher proportion of mild TMDs (60%), although the relationship between gender and TMDs severity was not statistically significant (p=0.290).
�
�
Discussion
In our sample of males and females aged 12 to 15 years, 63.3% of individuals presented a predominance of oral breathing, which is coherent with data from studies that reported variations between 6.6% and 77.8% of prevalence. Those varied results could relate to the different methods used to assess breathing mode in those studies. 5, 18, 19, 20
Regarding postural evaluation, our results indicate that oral breathers tend to have a more forward head posture than nasal breathers, which could stem from the former�s need to adapt their posture and thus the position of the head in order to promote the passage of air through the oropharyngeal space. 1, 6 ‑ 8
The literature supports our results by describing a forward head posture as a major change in individuals with a dominant oral breathing pattern. 7, 9 Baldini et al. (2013)6 found that the change in head posture could change the resting position of the jaw and occlusal contacts, as well as promote changes in the masticatory pattern, and that the breathing pattern would thus determine the development of malocclusion. 5, 19 Similarly, other authors 7, 10 reported a relationship between an oral breathing pattern and Angle Class II occlusion, which our results corroborate. We also verified statistically significant differences between the breathing pattern and Angle occlusal class. The dominance of the Class II occlusal pattern in oral breathers could derive from a different positioning of the tongue in the oral cavity that inhibits mandibular growth and stimulates forward maxillary growth. In accordance with the above three parameters, Nobili and Adversi (1996)20 related posture to Angle occlusal classification by demonstrating that individuals with Class II malocclusion tilted their heads forward. Our results have also shown changes in the anterior view of the horizontal head alignment between oral and nasal breathers. To our knowledge, there is no biological reason that could justify this directionality. The authors acknowledge ththat this may be a finding with no scientific grounding.
In our study, most children presenting Class I malocclusion had no TMDs according to the Fonseca Anamnestic Index.
However, 70% of Class II individuals had mild TMDs, with a statistically significant relationship between the groups. Some authors21 found that some occlusal factors, particularly Classes II and III, are risk factors for the development of TMDs. Most children in our study who were oral breathers and had Class II occlusion exhibited that feature.
Our study also found that individuals with oral breathing had an increased risk of developing mild TMDs, as corroborated by the results of Chaves.22 That situation could result from an altered function, which may constitute repetitive trauma to the TMJs and consequent dysfunction.
Our results show a statistically significant relationship between the oral breathing pattern and Class II malocclusion.
Also, as literature has revealed,23 imbalances in facial muscles in Class II individuals are normal, as a result of an increased overjet, and their facial profiles are generally convex. Some authors24 found a more convex profile among oral breathers than nasal ones, which our results confirm. Tourn� (1990)25 hypothesized that oral breathing was a chief etiological factor of induced excessive vertical growth.
Our results seem to corroborate that hypothesis, since oral breathing increased the odds of having an increased lower cervicofacial ratio by nine‑fold, and similar findings appear in other studies.26 The functional matrix hypothesis could explain that influence of oral breathing on the lower cervicofacial ratio. That hypothesis states that the origin, growth, and maintenance of all skeletal tissues and organs are always secondary, compensatory, and mandatory responses to temporally and operationally prior events or processes that occur in specifically related non‑skeletal tissues, organs, or functioning spaces. That is, the function directly influences the shape.
Considering that nasal breathing represents an important function in the stomatognathic system, if that function is altered to oral breathing, it may condition the skeletal growth of the surrounding structures. Oral breathing is thought to contribute to a posterior rotation of the mandible, with a consequent increase of the lower cervicofacial ratio, which could also interfere with the TMJs and thus result in or contribute to the development of TMDs. Furthermore, it should be considered that, in the growth period, the oral function may lead to adaptative changes of the TMJ, since it is highly adaptative in this period, responding to a wide variety of stimuli. Accordingly, TMDs symptoms experienced by young people may be transitory, and this fact was not controlled in this study, as it is beyond our scope.
Our results verified that changes in head and neck posture, breathing pattern, dental occlusion and the presence or absence of TMDs presented an interdependent and complex relationship.
Considering all the above and our results, it seems relevant to reinforce the importance of developing an interdisciplinary assessment of the breathing pattern, postural changes, facial features, and presence of TMDs. Therefore, the authors hypothesize that the assessment of the individual as a whole could play an important role in intervention planning and the preventive decision‑making process. If changes are detected early, practitioners can increase the possibility of prevention and treatment. However, those considerations are beyond the scope of our study, and further trials should be performed to enlighten the scientific community regarding their feasibility.
One limitation of this study is the absence of a clinical examination and laboratory findings for the diagnosis of TMDs.
Instead, we used a valid and reliable questionnaire � Fonseca�s Anamnestic Index, which is a self‑reported questionnaire often used for epidemiological studies on TMDs that allows characterizing the signs and symptoms of TMDs and obtaining a score about TMDs severity.27 Moreover, different studies support the use and validity of questionnaires for epidemiological studies on TMDs� symptoms. 28, 29 Since this was a cross‑sectional study, no etiological conclusions can be drawn, and the reader should have in mind that no clinical confirmation of the data retrieved by the participants was available.
Conclusions
Our results show an association between the presence of oral breathing and head anteriorization, signs and symptoms of TMDs, Class II malocclusion, convex facial profile, and increased lower cervicofacial ratio. TMDs were associated with occlusal Class II, and oral breathers had an increased risk of developing mild TMDs and increased lower cervicofacial ratio. Lastly, our results indicate no sex‑related differences in the prevalence of TMDs.
�
References
1. Khan M, Verma S, Maheshwari S, Zahid S, Chaudhary P. Neuromuscular dentistry: Occlusal diseases and posture. J Oral Biol Craniofac Res. 2013;3:146‑150.
2. Korbmacher H, Koch L, Eggers‑Stroeder G, Kahl‑Nieke B. Associations between orthopaedic disturbances and unilateral crossbite in children with asymmetry of the upper cervical spine. Eur J Orthod. 2007;1:100-4.
3. Solow B, Siersbaek‑ Nielsen S. Growth changes in head posture related to craniofacial development. Am J Orthod. 1986;89:132-40.
4. Perinetti G, Contardo L, Biasati AS, Perdoni L, Castaldo A. Dental malocclusion and body posture in young subjects: A multiple regression study. Clinics. 2010;65:689-95.
5. Cuccia AM, Lotti M, Caradonna D. Oral Breathing and Head Posture. Angle Orthod. 2008;78:77-82.
6. Baldini A, Nota A, Cravino G, Cioffi C, Rinaldi A, Cozza P. Influence of vision and dental occlusion on body posture in pilots. Aviat Space Environ Med. 2013;84:823‑7.
7. Tecco S, Tete S, Festa F. Electromyographic evaluation of masticatory, neck, and trunk muscle activity in patients with posterior crossbites Eur J Orthod. 2010;32:747‑52.
8. Crispiniano T, Bommarito S. Evaluation of orofacial muscles and body posture in pattients with mouth breathing and malocclusion. Rev Odonto. 2007;15:88-97.
9. Costa JR, Pereira SRA, Mitri G, Motta JC, Pignatari SSN, Weckx LLM. Rela��o da oclus�o dent�ria com a postura de cabe�a e coluna cervical em crian�as respiradoras orais. Rev Paul Pediatr. 2005;23:88-93.
10. de Lemos CM, de Souza Junqueira PA, Gomez MVSG, de Faria MEJ, de C�ssia Basso S. Study of the Relationship Between the Dentition and the Swallowing of Mouth Breathers. Intl. Arch. Otorhinolaryngol. 2006;10:114‑118.
11. Leeuw R, Klasser GD. Orofacial Pain. Guidelines for assessment, diagnosis and management. Quintessence Books. 5th Edition; 2013.
12. Helkimo M. Studies on Function of the Mastigatory System. Index for Anamnestic and Clinical Dysfunction and Occlusal state. Swed Dent J. 1974;67:101-21.
13. Van Der Weele L T, Dibbets JMH. Helkimo�s index: a scale or just a set of symptoms?. J Oral Rehabil. 1987;14:229‑237.
14. Campos J, Carrascosa, AC, Bonaf� F, Maroco J. Severity of temporomandibular disorders in women: validity and reliability of the Fonseca Anamnestic Index. Braz Oral Res 2014;28:1‑6.
15. Peck CC, Goulet JP, Lobbezoo F, Schiffman EL, Alstergren P, Anderson GC, List T. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J Oral Rehabil. 2014;41:2‑23.
16. Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G. Diagnostic Criteria for Temporomandibular Disorders (DC/ TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J Oral Facial Pain Head. 2014;28:6‑27.
17. Morimoto T, Karolczak APB. Associa��o entre as altera��es posturais e a respira��o bucal em crian�as. Fisioter Mov 2012;25:379‑88.
18. Moyers R. Ortodontia. 4th ed. Rio de Janeiro: Guanabara Koogan; 1991;p. 8‑16, p.175‑467.
19. Abreu RR, Rocha RL, Guerra �FM. Prevalence of mouth breathing among children. J Pediatr. 2008;84:467‑70.
20. Nobili A, Adversi R. Relationship between posture and occlusion: a clinical and experimental investigation. J Cranio Practice. 1996; 14(4): 274‑85.
21. Magnusson T, Egermark I, Carlsson GE. A prospective investigation over two decades on signs and symptoms of temporomandibular disorders and associated variables. A final summary. Acta Odontol Scand 2005;63:99‑109.
22. Chaves TC, Grossi DB, Oliveira AS, Bertolli A. Correlation between signs of temporomandibular (TMD) and cervical spine (CSD) disorders in asthmatic children. J Clin Pediatr Dent 2005;29:287‑92.
23. Proffit WR. Ortodontia Contempor�nea. 4th ed. Rio de Janeiro: Guanabara Koogan. 2007;p.155‑216.
24. Motonaga SM, Berti LC, Anselmolima WT. Respira��o bucal: causas e altera��es no sistema estomatogn�tico. Rev Bras� Otorrinolaringol. 2000; 66(41):373‑9.
25. Tourne LP. The long face syndrome and impairment of the nasopharyngeal airway. Angle Orthod 1990;60:167-76.
26. Ung N, Koenig J, Shapiro PA, Shapiro G, Trsk G. A quantitative assessment of respiratory patterns and their effects on dentofacial development. Am J Orthod Dentofac Orthop. 1990; 98: 523‑32.
27. Fonseca DM. Diagn�stico pela anamnese da disfun��o craniomandibular. RGO (Porto Alegre), 1994;42:23‑8.
28. Akhter R, Hassan N, Ohkubo R. The relationship between jaw injury, third molar removal, and orthodontic treatment and TMD symptoms in university students in Japan. J Oral Facial Pain Head. 2008;22:50‑56.29. Matsuka Y, Yatani H, Kuboki T, Yamashita A. Temporomandibular disorders in the adult population of Okayama City, Japan. CRANIO. 1996;14:158‑62.
�
Corresponding author.
Teresa Pinho
Correio eletr�nico: teresa.pinho@iucs.cespu.pt
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 2 November 2017
Accepted 4 August 2018
Available online 11 September 2018
