Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2019 | 60 (1) | 13-17
Case report
A rare extracranial arteriovenous malformation of the face: a case report
Uma malformação arteriovenosa extracraniana da face rara: caso clínico
a Tehran University of Medical Sciences, Shariati hospital, Tehran, Tehran Province, Iran
Askar Ghorbani - askar.ghorbani.40@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 1
Case report
Pages - 13-17
Go to Volume
Article History
Received on 15/08/2018
Accepted on 11/02/2019
Available Online on 25/03/2019
Keywords
Case report
A rare extracranial arteriovenous malformation of the face: a case report
Uma malformacao arteriovenosa extracraniana da face rara: caso clinico
Behnam Molavi, Mehrnaz Fallah Tafti, Farnaz Sinaei, Nazila Malekian, Askar Ghorbani*
Tehran University of Medical Sciences, Shariati hospital, Tehran, Tehran Province, Iran
http://doi.org/10.24873/j.rpemd.2019.03.441
Abstract
Arteriovenous malformations are classic examples of congenital vascular anomalies involving the head and the neck. Extracranial arteriovenous malformations constitute a small subgroup of these vascular malformations. Despite the rarity of these cases, their tendency to grow throughout life and their resulting complications make them one of the most life-threatening vascular lesions. Effective treatment of extracranial arteriovenous malformations is quite challenging, and different techniques have been proposed. The ultimate goal is to ablate the whole nidus, which is not readily achieved by either surgical resection or embolization. Therefore, the aim of arteriovenous malformations’ management is often the control of the lesions, rather than their complete obliteration. This study reports a case of giant facial arteriovenous malformation that was successfully treated by selective embolization and complete radical resection.
Keywords: Arteriovenous malformations, Extracranial, Face, Vascular malformations
Resumo
As malformações arteriovenosas são exemplos clássicos de anormalidades vasculares congénitas que envolvem a cabeça e o pescoço. As malformações arteriovenosas extracranianas constituem um pequeno subgrupo dessas malformações vasculares. Apesar da raridade destes casos, a tendência que têm para crescer ao longo da vida e as complicações resultantes fazem com que sejam uma das lesões vasculares que apresentam um maior potencial de fatalidade. O tratamento das malformações arteriovenosas extracranianas é bastante desafiador e têm sido propostas diferentes técnicas. O objetivo final é remover todo o nicho, o que não é imediatamente obtido por ressecção cirúrgica ou embolização. Portanto, o objectivo da gestão das malformações arteriovenosas é muitas vezes o controlo, em vez de obliteração completa. Neste estudo, foi relatado um caso de malformação arteriovenosa facial gigante que foi curada por embolização seletiva e resseção radical completa.
Palavras-chave: Malformações arteriovenosas, Extracraniana, Face, Malformações vasculares
Introduction
Arteriovenous malformations (AVMs) are rare congenital vascular lesions. According to their endothelial features, vascular lesions are classified into vascular tumor and vascular malformations (VMs). VMs can further be divided into low-flow lesions and high-flow lesions, including AVMs.1, 2 These lesions cause clinical signs and symptoms such as pain, bruit, ulceration and bleeding.3 The likelihood of intense and remittent hemorrhage is the main concern of patients with head and neck AVMs.4 Computed tomography (CT), Doppler ultrasonography, and magnetic resonance imaging, together with the clinical history, can be used to confirm the diagnosis and evaluate the extent of the lesions.5, 6 Surgical resection, embolization, electrothrombosis or a combination of these modalities have been performed to treat AVMs. Complete surgical excision is rarely possible because AVMs are usually diffuse, involving various tissues in critical anatomical areas.3, 7
Therefore, the goal of AVMs management is often the control rather than the complete obliteration of the lesions. Here we report a case of a giant facial AVM that was successfully treated by selective embolization and complete radical resection, despite the rare reports of successful resection of giant facial AVMs.
Case report
The patient was a 21-year-old man whose chief complaint was a cervical mass for the past 10 years. In the past 3 years, the mass, on the right side of the neck, had shown a rapid growth while the patient started to have gingival hypertrophy, right facial weakness, and red right eye. He had had two episodes of massive gingival bleeding and was unable to brush his teeth. He also reported a self-audible bruit and a thrill sensation when touching the lesion. His family history was unrevealing.
In the physical examination, his blood pressure was normal and his pulse rate showed a bounding pulse. A large mass measuring about 15 cm (in length) was evident on the right mandibular angle (Figures 1 and 2). It was spongy and had a palpable thrill. A strong bruit could be easily heard over the mass. The right eye was congested, and gingival hypertrophy along with purple discoloration of the labial mucosa was also evident (Figure 3). In the neurologic examination, complete facial weakness without any sensory symptoms of hypoesthesia or paresthesia was found on the right side. The rest of the neurologic examination was unremarkable.
The patient had undergone a diagnostic evaluation in another center and therapies had been initiated with the diagnosis of facial AVM (Figure 4). More specifically, it was an intraparotid AVM arising from external carotid branches including the facial, lingual, posterior auricular, and venous pouch of the external jugular vein. In the first embolization, a direct puncture of the venous pouch and a mixed arterial and venous embolization (by Onyx) were done. The patient had undergone two sessions of embolization with an initial partial improvement followed by deterioration in a matter of months.

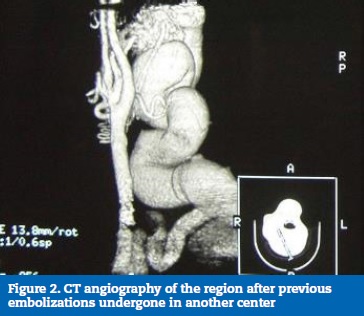

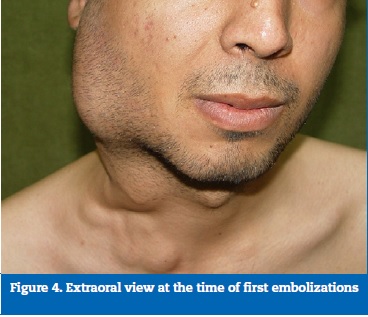
The investigations were repeated with a CT angiography of the region (Figure 2). A vascular lesion with a very complex anatomy was found in the right cervical area. The investigation proceeded with an angiography. The angiograms showed multiple feeding arteries, including the right facial, lingual, external carotid, and ophthalmic arteries. A huge draining vein was connected to the right external jugular vein, and there was venous engorgement in the nearby veins, including the facial and angular veins. Embolization was performed at the origin of the right external carotid artery. A small branch from the right ophthalmic artery was also selectively embolized (by Onyx). In the next step, the large draining vein was coiled (Figure 5). The isolated vascular lesion was then successfully resected by the vascular surgeon. In this procedure, an incision was made along the anterior border of the sternocleidomastoid (SCM) muscle. After releasing the SCM, a dissection up to the surface of the mass was done. The external jugular vein and all of its branches leading to the mass were isolated and ligated separately. Also, the external carotid artery inferiorly supplying the mass was ligated. After complete dissection, the mass was totally excised.

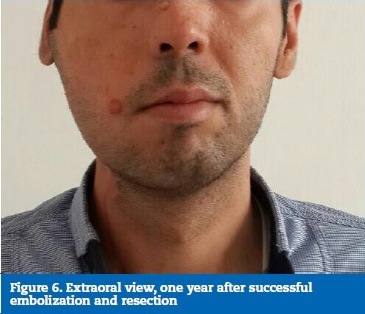
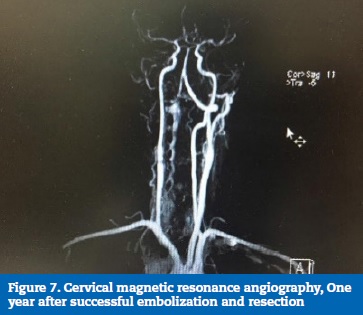
During the year after the embolization and surgery, besides no signs of recurrence, a significant reduction in the size of the mass and a significant improvement in the gingival-oral status were observed. A cervical magnetic resonance angiography (MRA) showed no residual mass in the area of the previous surgery (Figures 6 and 7).
Discussion and conclusions
Arteriovenous malformations are classified as congenital high-flow vascular anomalies and constitute only 4.7% of all vascular lesions. The central nervous system is the most common location, and extracranial AVMs occur quite rarely.8, 9
Even though most AVMs are in the midface and the oral cavity, in the neck and the face, rare instances have been reported in the larynx and the cervical soft tissue.10
Extracranial AVMs, like other types of AVMs, are originated by a mal-development of the vascular system in the 4th-6th weeks of gestation.11 As a result, a defective capillary network connects the high-pressure arterioles and the low-pressure venous system. Even though these malformations are congenital, they usually do not manifest at birth and early childhood. Extracranial AVMs typically progress and expand, and this occurs most frequently in adolescence.7, 12 Consequently, massive bleeding, disfigurement, soft-tissue and bone destruction, surface ulceration, and high-output heart failure may ensue.10 13 There are various grading systems for AVMs, with the Schobinger being one of the most widely used.11 According to this classification, our patient had a class II AVM (a pulsatile lesion with soft-tissue infiltration without cutaneous or cardiac complications).
The strategy for the treatment of extracranial AVMs is a matter of continuing debate. It is best individualized based on the patient’s age, class of AVM, its location, and the feasibility of using different techniques. The options vary from the conservative watch-and-wait approach to embolization and surgery, independently or in combination.13 However, according to the current knowledge, embolization followed by surgical resection is the method of choice in most cases.10 Incomplete embolization without resection produces a hypoxic environment and further expands the lesion through recruitment of new feeding arteries.11, 14, 15 In this case study, the previous embolization in the external carotid artery and branches (the facial and the lingual arteries) had led to temporary regression but was followed by a rebound growth with the addition of new feeders. Selective embolization of the external carotid artery and a branch of the ophthalmic artery were performed, and then the huge vein that drained into the external jugular vein was successfully obliterated by coiling. After vascular isolation of the lesion, it was radically resected. The major concern in the follow-up process of these lesions is the risk of recurrence.
As it was already mentioned, the patient was followed for a year, and the follow-up imaging did not show any evidence of recurrence.
Reports of successful resection of giant facial AVMs are rare, and most of them lack the follow-up imaging to search for the recurrence. This patient is a novel example of a giant facial AVM cured by a combination of careful embolization and complete surgical resection.
References
1. Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children a classification based on endothelial characteristics, Plast Recontr Surg. 1982;69:412-22.
2. Oueis H, Geist JR, Tran MU, Stenger J. High-flow arteriovenous malformations of the mandible and the maxilla: report of 2 cases. Pediatr Dent. 2010;32:451-6.
3. Kitagawa, A, Yamamoto, T, Matsunaga, N, Yamaji, M, Ikeda, S, Izumi, Y, Hagihara, M, Ota, T, Ishiguchi, T. Polidocanol Sclerotherapy Combined with Transarterial Embolization Using n-Butyl Cyanoacrylate for Extracranial Arteriovenous Malformations. Cardiovasc Intervent Radiol. 2018;41:856-66.
4. Garzon MC, Huang JT, Enjolras O, Frieden IJ. Vascular malformations: Part I. J Am Acad Dermatol. 2007;56:353-70.
5. Monsignore LM, Nakiri GS, Santos DD, Abud TG, Abud DG. Imaging findings and therapeutic alternatives for peripheral vascular malformations. Radiol Bras. 2010;43:185-94.
6. Carvalho MF, Oliveira NK, Duailibi E, Homem MD, Deboni MC. Extensive arteriovenous malformation in the face of a pediatric patient–Case report. Rev Port Estomatol Med Dent Cir Maxilofac. 2014;55:250-5.
7. Gupta, A. K, Iyengar S. N, Sharma, A. Scalp arteriovenous malformation: A case report with review. Rom Neurosurg. 2018;32:151-5.
8. Visser A, Fitz JT, Tan ST. Surgical management of arteriovenous malformation. J Plast Reconstr Aesthet Surg. 2011;64:283-91.
9. Gomes MM. Arteriovenous fistula: a review and ten-year experience at the Mayo Clinic. InMayo Clin Proc. 1970;45:81-102.
10. Eivazi B, Werner JA. Extracranial vascular malformations (hemangiomas and vascular malformations) in children and adolescents–diagnosis, clinic, and therapy. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2014;13:Doc02.
11. Kohout MP, Hansen M, Pribaz JJ, Mulliken JB. Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg. 1998;102: 643-54.
12. Ogul, H, Keskin, E. Huge Extra Cranial Arteriovenous Malformation Presenting as Fluctuant Mass in Scalp. J Craniofac Surg. 2018;29:828-9.
1313. Liu AS, Mulliken JB, Zurakowski D, Fishman SJ, Greene AK. Extracranial arteriovenous malformations: natural progression and recurrence after treatment. Plast Reconstr Surg. 2010;125:1185-94.
14. Sure U, Battenberg E, Dempfle A, Tirakotai W, Bien S, Bertalanffy H. Hypoxia-inducible factor and vascular endothelial growth factor are expressed more frequently in embolized than in nonembolized cerebral arteriovenous malformations. Neurosurg. 2004;55: 663-70.
15. Kadirvel R, Dai D, Ding YH, Danielson MA, Lewis DA, Cloft HJ, Kallmes DF. Endovascular treatment of aneurysms: healing mechanisms in a swine model are associated with increased expression of matrix metalloproteinases, vascular cell adhesion molecule-1, and vascular endothelial growth factor, and decreased expression of tissue inhibitors of matrix metalloproteinases. Am J Neuroradiol. 2007;28:849-56.
Askar Ghorbani
E-mail address: askar.ghorbani.40@gmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interest
The authors have no conflicts of interest to declare.
Article history:
Received 15 August 2018
Accepted 11 February 2019
Available online 25 March 2019