
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2017 | 58 (4) | 212-218
Original research
Dental implants in patients with xerostomia
Implantes dentários em pacientes com xerostomia
a Oral Medicine Department, Facultad de Medicina y Odontologia. Universidad de Murcia, Murcia, Spain
b Interdisciplinary Laboratory of Clinical Analysis Interlab-UMU, Regional Campus of International Excellence Campus Mare Nostrum, University of Murcia, Murcia, Spain
Pia Lopez-Jornet - majornet@um.es
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 4
Original research
Pages - 212-218
Go to Volume
Article History
Received on 10/12/2017
Accepted on 03/03/2018
Available Online on 22/03/2018
Keywords
Original research
�
Dental implants in patients with xerostomia
Implantes dentarios em pacientes com xerostomia
�
Consuelo Rodrigueza, Alfonso Zambudioa, Gemma Vicentea, Eduardo Pons-Fustera,Asta Tvarijonaviciuteb, Pia Lopez-Jorneta,*
a Oral Medicine Department, Facultad de Medicina y Odontologia. Universidad de Murcia, Murcia, Spain.
b Interdisciplinary Laboratory of Clinical Analysis Interlab-UMU, Regional Campus of International Excellence Campus Mare Nostrum, University of Murcia, Murcia, Spain
�
�
http://doi.org/10.24873/j.rpemd.2017.02.212
�
ABSTRACT
Objectives: To evaluate the dental, periodontal and implantological state of patients with xerostomia.
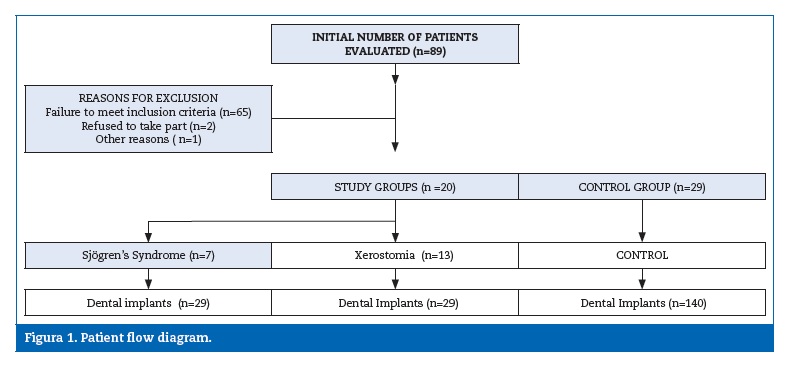
Methods: This transversal study reviewed a total of 20 patients with xerostomia, plus 29 patients in the control group. The two groups (study and control) had a total of 198 implants.
Patients� oral and periodontal health was evaluated, including bleeding index, gingival index, clinical attachment level, probing depth, pain on percussion, gingival suppuration, and oral quality of life (OHIP-14).
Results: Mean patient age was 59.8 � 12.04, and evolution time was 3.6 � 3.05 years. Plaque index was higher in patients with xerostomia than in the control group (p=0.012). No significant differences were found in periodontal disease between the groups (p>0.05). Fifteen percent of patients in the xerostomia group presented mucositis and probe depths shorter than 3 mm. Overall quality of life (OHIP-14) was high in both groups.
Conclusions: Dental implants are a favorable treatment option for patients with xerostomia.
Keywords: Dental implant, Sj�gren�s Syndrome, Xerostomia
�
RESUMO
Objetivos: Estudar o estado de sa�de oral e periodontal em pacientes com implantes dent�rios e xerostomia.
M�todos: Este estudo transversal analisou um total de 20 pacientes com xerostomia (grupo de estudo) e 29 pacientes sem xerostomia (grupo controlo). Os dois grupos inclu�ram um total de 198 implantes dent�rios. O estado de sa�de oral e periodontal dos pacientes foi avaliado atrav�s do �ndice de placa, �ndice de hemorragia, �ndice gengival, n�vel cl�nico de inser��o, profundidade de sondagem, dor � percuss�o, supura��o gengival e qualidade de vida oral (OHIP-14).
Resultados: A m�dia de idades dos pacientes foi de 59,8�12,04 e o tempo de evolu��o foi de 3,6� 3,05 anos. O �ndice de placa foi maior em pacientes com xerostomia que nos pacientes do grupo controlo (p=0,012). N�o foram encontradas diferen�as estatisticamente significativas na doen�a periodontal entre os grupos (p>0,05). Quinze por cento dos pacientes no grupo xerostomia apresentaram mucosite e profundidades de sondagem inferiores a 3 mm. A qualidade de vida global (OHIP-14) foi alta em ambos os grupos.
Conclus�es: Os implantes dent�rios s�o uma op��o de tratamento favor�vel em pacientes com xerostomia.
Palavras-chave: Implantes dent�rios, Sindroma de Sj�gren, Xerostomia
�
Introduction
In recent decades, the use of implants in dentistry has increased to become a relatively common treatment. Some pathologies and patient habits constitute risk factors for a successful outcome, but as our knowledge of implant therapies and patient management has increased, the cases in which dental implants can be indicated have grown in number. 1 , 2 In general, the factors that influence dental implant success include the patient�s health status, the characteristics of the implant site, the technique employed, and the type of prosthetic rehabilitation chosen, among others. 1 - 6
The term �xerostomia� refers to symptoms (subjective), while the term �hyposalivation� refers to function (objective) in cases of xerostomia. Although the two terms are often applied as synonyms, patients suffering from xerostomia do not necessarily experience hyposalivation. 7 - 9 Xerostomia usually occurs when salivary flow drops 40% from the original value while hyposalivation occurs with values below 0.1 ml/min.
Sj�gren�s syndrome (SS) is a chronic autoimmune disease that results from a lymphocyte infiltration of the exocrine glands, especially tear glands and salivary glands, which leads to progressive gland damage, consequently causing sicca symptoms (xerostomia, xerophthalmia); B-lymphocyte hyperactivity is the main immunological mechanism involved. That disease may present as primary SS (pSS) or be associated with another connective tissue diseases such as rheumatoid arthritis or systemic lupus erythematosus, as what is known as secondary SS (sSS).10
Patients usually present a high incidence of dental caries as a consequence of decreased saliva production. This condition can lead to the loss of teeth and, consequently, a need for prosthetic rehabilitation. In the absence of the lubricating effect of saliva, the oral mucosa is prone to infection and lesion caused by rubbing against dental prostheses. When that happens, the prosthetic retention becomes inadequate, often leading to speech and eating difficulties and deteriorating quality of life.11 Under these circumstances, rehabilitation by means of dental implants is of particular interest. 12 - 17 Implant treatments show high success rates and longitudinal studies conducted among the general population show survival rates that vary between 90 and 95% over 5-10-year follow-ups, which have made implantology one of the most widely used dental treatments during the last 20-30 years. 3 - 6
Little scientific literature has been published on dental implant treatment in patients presenting xerostomia and SS, and the existing literature consists mostly of individual case reports or small case series involving patients. 15 , 16 Binon at al.17 described a case of xerostomia caused by SS and osseointegrated implants. Isidor at al.18 found an 84% implant success rate after a 4-year follow-up. Payne at al.19 found an 88.4% success rate in 26 implants placed in three patients, although the follow-up period was only two years.
We hypothesize that the treatment outcome of implant-therapy patients with xerostomia and suspected SS is similar to the results obtained in matched healthy controls.
The objective of this study was to evaluate the dental, periodontal and implantological state of patients with xerostomia.
Materials and methods
A total of 89 patients were referred by the Rheumatology Service of the Morales Meseguer Hospital (Murcia, Spain) with xerostomia derived from suspected SS, according to the European criteria proposed by the American-European Consensus Group.10 Patients were then asked if they had dental implants.
All patients were adults in full possession of their faculties and able to answer questions and participate in data registration.
The study was conducted at the Dental Clinic of the Faculty of Medicine and Dentistry, University of Murcia (Spain).
Patients were recruited consecutively over a period from September 2014 to April 2017. Of these, 20 patients who had dental implants were invited to take part in the study. An SS diagnosis was confirmed in seven cases according to the European criteria proposed by the American-European Consensus Group.10 The remaining thirteen patients presented xerostomia (Figure 1).
�
�
Patients with lymphoma, acquired immune deficiencysyndrome (AIDS), sarcoidosis and graft-versus-host disease, as well as patients in radiotherapy and/or chemotherapy, were excluded.
A control group was created comprising patients with dental implants who were willing to take part in the study but did not suffer any symptoms of xerostomia or autoimmune disease nor presented any salivary gland pathology. The study protocol was designed to meet the criteria established by the Declaration of Helsinki for experiments involving human subjects and was approved by the University of Murcia�s Ethics Committee.
All patients were provided with full information about the purpose of the study and the procedures involved before giving their informed consent in writing to participate in the study.
The work followed the STROBE guidelines for case-control studies. A single clinician performed all oral and periodontal assessments and evaluations of teeth and implants.
Dental caries was assessed with the DMFT (decayed, missing, filled teeth) index, according to the 1997 WHO parameters.20
The Silness-L�e index was used to evaluate the bacterial plaque on the gingival area around each of the teeth present in the oral cavity (except third molars); this technique does not require plaque disclosing agents. Four surfaces per tooth were evaluated (vestibular, mesial, palatine and distal) and a score of 0-3 was attributed to each of them, depending on the amount of plaque visible: 0, no plaque; 1, plaque only registered when passing a probe over the tooth surface; 2, moderate accumulation of plaque deposits easily visible; 3, abundance of soft material and/or calculus. The final score was obtained by totaling the score on all the surfaces explored and dividing this figure by the total number of surfaces examined.
To evaluate the presence of gingival inflammation, the four dental surfaces (mesial, vestibular, distal and palatine) of all the teeth present in the oral cavity were evaluated using a periodontal probe. The presence of bleeding on probing was marked by a plus sign and the absence by a minus sign. A percentage was calculated applying the formula: (number of surfaces presenting bleeding/number of surfaces with no bleeding) x 100. The value 0 was considered to indicate gingival health.
The probing depth was measured for each tooth present in the oral cavity using a millimeter probe. Six points per tooth were explored.The same six sites were also explored to find the percentage of sites presenting epithelial insertion loss greater than 3 mm. Gingival recession was obtained by measuring (in millimeters) the distance from the amelocemental junction to the gingival margin.21 To calculate insertion loss, the recession and pocket depth were added together for each site explored, and the index was obtained by applying the formula: (number of sites explored with insertion loss > 3 mm / number of sites explored) x 100. Periodontitis was classified according to Becks and Loe criteria,17 considering a value of 0% as indicating no periodontal disease, 0-32% as slight periodontitis, 33-66% as moderate periodontitis, and 67-100% as severe periodontitis.
The following data were collected: the implant position (anterior when in the canine or incisor area and posterior when in the molar or premolar area), its antagonists (natural teeth, prosthesis), its localization (upper arch, lower arch), the presence/absence of signs of inflammation in the mucosa around it (such as redness, dehiscence or altered form), pain on percussion and mobility (yes/no).
Sialometry was performed to measure the overall saliva at rest using the drainage technique. Patients were instructed not to eat, drink, smoke, chew, or perform oral hygiene in the 60 min before the saliva collection using the drainage technique.22
Samples were collected following a standardized 15-minute procedure between 9 a.m. and 12 p.m., and an unstimulated salivary flow of ≤1.5mm/15 min was considered positive.
The Thompson Xerostomia Inventory23 was applied to assess xerostomia symptoms; the inventory consists of 11 items referring to the four weeks previous to the conduction of the test and evaluates the frequency of dry mouth symptoms.
Patients� quality of life was assessed using the OHIP-14 (Oral Health Impact Profile) questionnaire (Spanish version), which consists of 14 questions assessing seven domains formulated in response to a theoretical model of oral health, and provides scores ranging from 0 to 56, with higher scores indicating a poorer quality of life.24
In addition, overall patient satisfaction with implant-supported prostheses was assessed in terms of aesthetics and masticatory function, using a visual analog scale (VAS) scoring 0-10 (0 = completely dissatisfied; 10 = extremely satisfied). Subjects were asked to mark a vertical line through a 10-cm horizontal line to indicate their level of satisfaction.
Data were analyzed using the SPSS 19.0 statistics program (SPSS� Inc, Chicago, IL, USA). A descriptive study was made for each variable. The Kolmogorov-Smirnov normality test and Levene�s homogeneity of variance test were applied; data showed a skewed distribution, and so were analyzed using a non-parametric ranking test. The associations between the different qualitative variables were studied using Pearson�s chi-square test. A p≤0.05 was accepted as statistically significant.
Results
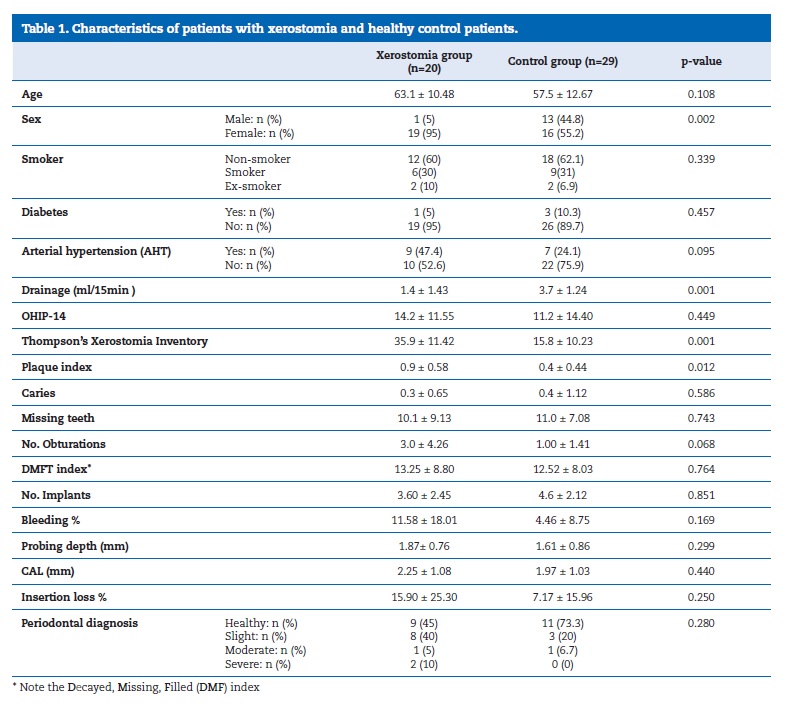
The mean age of the patient group was 59.8 � 12.04, with a minimum age of 30 years and maximum of 79. Of the 49 subjects, 14 were men (28.6%) and 35 women (71.4%) (Table 1).
�
�
It was possible to observe how xerostomia interfered in the oral function of the 49 patients as the Thompson Xerostomia Inventory obtained higher scores in the study group, 35.9 � 11.40 versus 15.8� 10.23 in the control group (p=0.001). The plaque index was significantly higher in patients with xerostomia compared with the control group (p=0.012). Regarding probing depth around natural teeth, study group patients obtained 1.8 � 0.76 mm, while control patients obtained 1.6 � 0.86 mm (p=0.299).
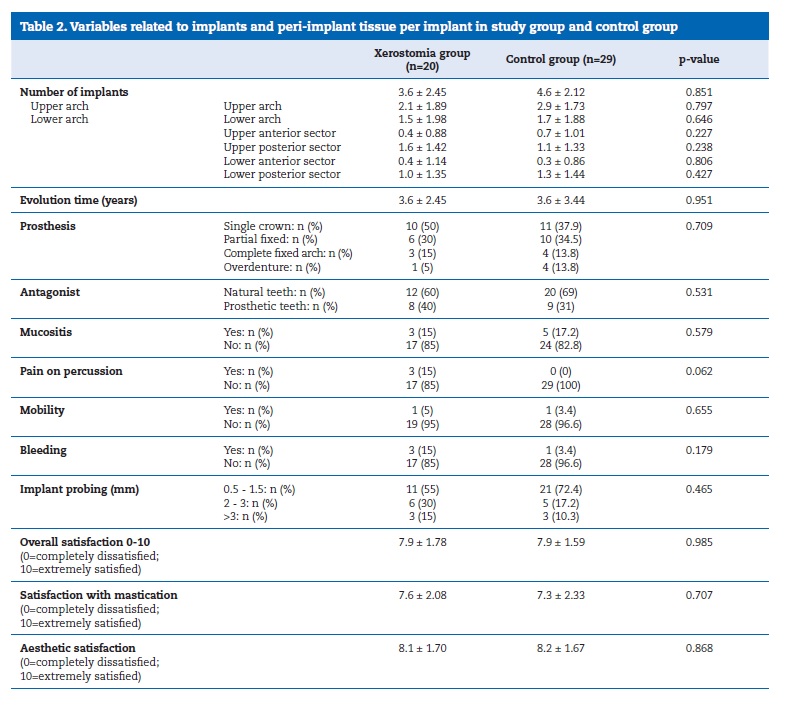
A total of 198 implants were assessed. The mean evolution time after implant placement was 3.6 � 3.04 years, ranging from a minimum of 6 months to a maximum of 12 years. Although 198 implants were included in the study, four patients in the study group reported losing a total of four implants, while one control group patient reported losing two implants.
No significant differences were found in the OHIP-14 quality of life scores, with 14.2 � 11.50 in the study group versus 11.2 � 14.40 in the control group (p=0.449). The overall satisfaction with implant rehabilitation was high in both groups (Table 2).
�
�
Discussion
This single-center study assessed the clinical state of teeth and implants in patients with xerostomia (hyposalivation) compared with a control group without xerostomia. The study group presented dry mucosas and a higher plaque index than the control group (p=0.012). However, despite these findings, patients presenting xerostomia did not suffer more from periodontal disease, a fact that concurs with previous research. 12 , 20 , 24
Many studies have provided information about risk factors for implant survival, but the information has been heterogeneous, and the evidence for absolute contraindications to implant placement remains scarce. 1 - 4 Currently, it seems that some of the diseases and clinical circumstances previously regarded as contraindications to implant insertion are no longer so, thanks to scientific evidence of successful treatment outcomes in cases published during the past ten years.1,6,24 In this sense, a wider knowledge of the underlying disease has improved the management of implantology patients with bone metabolism disorders, diabetes mellitus, SS, xerostomia, among others. 5 , 6 Nevertheless, it is clear that systemic diseases can affect oral tissues, increase susceptibility to other diseases, or interfere with the healing of surgical wounds. Implant survival rates in healthy individuals are high: 93-97%. 1 - 4 Of the 198 implants assessed in the present study, the patients in the study group reported having lost four while a single patient in the control group lost two during the first months following surgery.
Peri-implant mucositis is fairly common � occurs in around 10% of cases � and constitutes a considerable clinical challenge. The present study investigated whether xerostomia patients might present more peri-implant mucositis, or bleeding on probing, than a healthy population of similar age and the results were similar.
Studies of dental implants in SS patients are scarce and very limited in terms of follow-up duration. Some are individual case reports. 15 , 16 Binon at al.17 described a case with mandibular osseointegrated implants that remained stable after a 13-year follow-up. Isidor at al.18 obtained an 84% success rate among 54 implants placed in eight patients. Payne at al.19 described a case series of 26 implants placed in three patients, obtaining a success rate of 88.4% during a follow-up of only two years. It is very important to understand that oral treatment does not end when surgical procedures are completed: ongoing monitoring of patients can be crucial. Korfage at al.26 examined 50 patients with SS and found a 14% prevalence of peri-implantitis (11% of the implants placed), which is a rate similar to that of healthy subjects. Over the 46-month follow-up, the implant survival rate was 97%, as, of the 142 implants placed, four from two patients were lost.
Those authors also reported that, in those patients, oral functioning correlated negatively with xerostomia and mastication capacity so that SS did not constitute a barrier to osseointegration or implant survival.
These results also agree with a research conducted by Albertcht at al.27 with 32 SS patients and a mean number of implants per patient of 3.1 � 2.00. A total of five out of 104 (4.8%) implants had to be eliminated over a period of 4.9 years. Notably, 75% of the patients were very satisfied with their implants. Although that study had the largest sample size studied to date, it depended on patient reports instead of dental exploration carried out by a professional.
After any implant-based treatment, it is essential to assess patient satisfaction with the treatment outcome, to ensure that general satisfaction, comfort, stability, speech and mastication capacity are adequate. Improvements in these areas have brought benefits in terms of the patients� social and psychological well-being, as shown when objective methods for evaluating satisfaction and quality of life are applied (such as the OHIP-14). In 2013, Kuoppala at al.28 used the OHIP-14 to assess 58 patients who had undergone rehabilitation by means of implants, finding significant improvement in their quality of life after treatment. Reductions in saliva flow can compromise quality of life and patient satisfaction with treatment outcomes. However, the present study did not find statistically significant differences in quality of life between the study and control groups.
The present findings agree with other studies, 26 , 27 suggesting that SS does not compromise osseointegration biology despite a considerable number of dentists and rheumatologists having expressed initial concerns over the potential dangers to osseointegration. The present study had some limitations: the number of patients with implants, which was small, and the study design.
Conclusion
To sum up, based on the research available, implant survival rates among SS patients would appear to be comparable to those of patients free from systemic diseases. Dental implants are a favorable treatment option for patients with xerostomia.
�
REFERENCES
1. Beikler T, Flemmig TF. Implants in the medically compromised patient. Crit Rev Oral Biol Med. 2003;14:305-16.
2. Bornstein MM, Cionca N, Mombelli A. Systemic conditions and treatments as risks for implant therapy. Int J Oral Maxillofac Implants. 2009;24(Suppl):12-27.
3. Albrektsson TN, Donos G. Working. Implant survival and complications. The third EAO consensus conference 2012. Clin Oral Implants Res. 2012;23(Suppl 6):63-5.
4. Diz P, Scully C, Sanz M. Dental implants in the medically compromised patient. J Dent. 2013;41:195-206.
5. Alsaadi G, Quirynen M, Kom�rek A, van Steenberghe D. Impact of local and systemic factors on the incidence of late oral implant loss. Clin Oral Implants Res. 2008;19:670-6.
6. Mombelli A, Cionca N. Systemic diseases affecting osseointegration therapy. Clin Oral Implants Res. 2006;17:97-103.
7. Amerongen AV, Veerman EC. Saliva � the defender of the oral cavity. Oral Dis. 2002;8:12-22.
8. Epstein JBDC. Villines and H.Y. Sroussi. Oral symptoms and oral function in people with Sj�gren�s syndrome. Clin Exp Rheumatol. 2015;33:132-3.
9. Donaldson MJ. Epstein and D. Villines. Managing the care of patients with Sj�gren syndrome and xerostomia: comorbidities medication use and dental care considerations. J Am Dent Assoc. 2014;145:1240-7.
10. Vitali C, Bombardieri S, Jonsson R at al. Classification criteria for Sj�gren�s syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002;61:554-8.
11. Pereira R, Amaral J, Marques D, Barcelos F, Patto JV, Mata A. Qualidade de vida oral e sist�mica na S�ndrome de Sj�gren Prim�ria. >Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58:97-104.
12. Bolstad AI, Skarstein K. Epidemiology of Sj�gren�s Syndrome � from an Oral Perspective. Curr Oral Health Rep. 2016; 328-36.
13. Le Gall M, Cornec D, Pers JO at al. A prospective evaluation of dental and periodontal status in patients with suspected Sj�gren�s syndrome. Joint Bone Spine. 2016;83:235-6.
14. Antoniazzi RP, Miranda LA, Zanatta FB at al. Periodontal conditions of individuals with Sj�gren�s syndrome. J Periodontol. 2009;80:429-35.
15. Reichart PA, Schmidt-Westhausen AM, Khongkhunthian P, Strietzel FP. Dental implants in patients with oral mucosal diseases � a systematic review. J Oral Rehabil. 2016;43:388-99.
16. Candel-Marti ME, Ata-Ali J, Pe�arrocha-Oltra D, Pe�arrocha- Diago MA, Bag�n JV. >Dental implants in patients with oral mucosal alterations: an update. Med Oral Patol Oral Cir Bucal. 2011;16:e787-93.
17. Binon PP. Thirteen-year follow-up of a mandibular implantsupported fixed complete denture in a patient with Sj�gren�s syndrome: a clinical report. J Prosthet Dent. 2005;94:409-13.
18. Isidor F, Br�ndum K, Hansen HJ, Jensen J, Sindet-Pedersen S. Outcome of treatment with implant-retained dental prostheses in patients with Sj�gren syndrome. Int J Oral Maxillofac Implants. 1999;14:736-43.
19. Payne AG, Lownie JF, Van Der Linden WJ. Implant-supported prostheses in patients with Sj�gren�s syndrome: a clinical report on three patients. Int J Oral Maxillofac Implants. 1997;12:679-85.
20. World Health Organization. Oral Health Surveys: Basic methods. 3rd ed. Genebra: WHO, 1997.
21. Beck JD, L�e H Epidemiological principles in studying periodontal diseases. Periodontol 2000. 1993;2:34-45.
22. Navazesh M, Kumar SK. Measuring salivary flow: challenges and opportunities. J Am Dent Assoc. 2008;139(Suppl):35S-40S.
23. Thomson WM. Measuring change in dry-mouth symptoms over time using the Xerostomia Inventory. Gerodontology. 2007;24:30-5.
24. Montero-Mart�n J. Bravo-P�rez M. Albaladejo-Mart�nez A. Hern�ndez-Mart�n LA. Rosel-Gallardo EM. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med Oral Patol Oral Cir Bucal. 2009;14:E44-50.
25. Krennmair G, Seemann R, Piehslinger E. Dental implants in patients with rheumatoid arthritis: clinical outcome and peri-implant findings. J Clin Periodontol. 2010;37:928-36.
26. Korfage A, Raghoebar GM, Arends S at al. Dental implants in patients with Sj�gren�s syndrome. Clin Implant Dent Relat Res. 2015;18:937-45.
27. Albrecht K, Callhoff J, Westhoff G, Dietrich T, D�rner T, Zink A. The prevalence of dental implants and related factors in patients with Sj�gren syndrome: results from a cohort study. J Rheumatol. 2016;43:1380-5.
28. Kuoppala R, N�p�nkangas R, Raustia A. Quality of life of patients treated with implant-supported mandibular overdentures evaluated with the oral health impact profile (OHIP-14): a survey of 58 patients. >J Oral Maxillofac Res. 2013;4:e4.
�
P�a L�pez-Jornet
Correio eletr�nico: majornet@um.es
�
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
�
Conflict of interest
The authors have no conflicts of interest to declare.
�
Article history:
Received 10 December 2017
Accepted 3 March 2018
Available online 22 March 2018
