
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Rev Port Estomatol Med Dent Cir Maxilofac | 2017 | 58 (1) | 52-57
Original research
Diode LASER surgery in the treatment of fibrous hyperplasia: a prospective case series study
Tratamento da hiperplasia fibrosa com laser cirúrgico de diodo: estudo prospectivo tipo série de casos
a Department of Oral Surgery and Pathology. School of Dentistry. Universidade Federal de Minas Gerais. Belo Horizonte - MG, Brazil.
Marcio Bruno Figueiredo Amaral - marciobrunoamaral@yahoo.com.br, marciobrunoamaral@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 1
Original research
Pages - 52-57
Go to Volume
Article History
Received on 17/04/2016
Accepted on 13/02/1917
Available Online on 31/03/2017
Keywords
Original research
Diode LASER surgery in the treatment of fibrous hyperplasia:
a prospective case series study
Tratamento da
hiperplasia fibrosa com laser cirúrgico de diodo: estudo
prospectivo tipo série de casos
Marcio Bruno Figueiredo Amaral*, Larissa Fernandes Correia, Mariana Saturnino de Noronha, Ricardo Alves Mesquita
Department of Oral Surgery and Pathology. School of Dentistry. Universidade Federal de Minas Gerais. Belo Horizonte – MG, Brazil.
http://doi.org/10.24873/j.rpemd.2017.05.001
Abstract
Objective: Fibrous hyperplasia is frequently treated by surgical incision with a scalpel associated with removal of chronic trauma. However, hemostasis of the surgical wound is specially difficult for patients with hemorrhagic disorders or those undergoing antithrombotic therapy without the suturing of the wound borders. High-power LASER have been applied as a useful tool in the management of soft tissue lesions. Therefore, the present study aimed to present a prospective case series of fibrous hyperplasia treated using a high-power diode LASER.
Methods: Fifteen patients with fibrous hyperplasia were enrolled in this study. LASER irradiation was performed using an 808 nm diode LASER with an optical fiber of 600 μm, at a power of 2.0W to 3.5W (average 2.96W), in a continuous-wave mode. The treatment performance of fibrous hyperplasia using a high-power diode LASER was determined by evaluating the pain, postoperative functional alterations, edema, secondary infection and bleeding.
Results: Diode LASER surgery proved to be effective and presented a good performance in the treatment of fibrous hyperplasia.
Conclusions: Randomized clinical trials may be performed to compare diode LASER and other LASER systems with conventional surgery and electrosurgery in the management of fibrous hyperplasia and other oral lesions.
Keywords: Diode laser, Hyperplasia, Oral surgery
Resumo
Objetivo: Hiperplasia fibrosa é frequentemente tratada pela excisão cirúrgica com bisturi associado com a remoção do trauma crônico. Entretanto, hemostasia da ferida cirúrgica é especialmente dificultada em pacientes com desordens hemorrágicas ou aqueles submetidos a terapia anticoagulante sem sutura das bordas das feridas cirúrgicas. LASER de alta intensidade tem sido utilizados como uma ferramenta útil no manejo de lesões de tecidos moles. Portanto, o presente estudo objetiva-se a apresentar uma série de casos prospectivo no tratamento da hiperplasia fibrosa utilizando o LASER de diodo de alta intensidade.
Métodos: Quinze pacientes com hiperplasia fibrosa foram envolvidos no estudo. A aplicação do LASER foi realizada utilizando um LASER de diodo de 808nm com uma fibra óptica de 600μm, em uma potência de 2.0W a 3.5W (média 2.96W), em modo continuo. A eficácia do tratamento da hiperplasia fibrosa utilizando LASER de diodo de alta intensidade foi determinada pela avaliação da dor, alterações funcionais pós-operatórias, edema, infecção secundária e sangramento.
Resultados: O LASER cirúrgico de diodo provou ser efetivo e apresentou bom resultado no tratamento da hiperplasia fibrosa.
Conclusões: Ensaios clínicos randomizados devem ser realizados comparando LASER de diodo e outros sistemas de LASER com a cirurgia convencional e eletrocautério no manejo da hiperplasia fibrosa e outras lesões orais.
Palavras-chave: Laser de diodo, Hiperplasia, Cirurgia oral
Introduction
Hyperplasia is an increase in the number of cells in any portion of human tissues,including the oral cavity tissues. Fibrous hyperplasia (FH) is caused by a low-intensity chronic trauma, often provoked by ill-fitting dentures or by parafunctional habits,and is represented by an increase in fibroblast cells and collagen fibers. 1 FH is a frequent oral mucosal disease that affects 5% to 16.7% of the population. 2 , 3
FH first appears as a limited-size growth, with a fibrous to flaccid consistency, and an erythematous to pale color lesion that may be ulcerated. FH presents a slow growth that ceases with the removal of the traumatic agent. In the majority of cases, as FH is painless, the patient may not realize its existence.
However, the patient may complain of pain if the area is ulcerated or has an associated infection caused by a fungus, such as Candida ssp. Moreover, the flange of the complete or partial denture often fits conveniently into the folds of the lesion. 4 , 5
FH is frequently treated by surgical incision with a scalpel associated with removal of chronic trauma. Scalpel techniques are associated with a loss of sulcus depth and/or with the full elimination of the vestibule in cases induced by ill-fitting dentures.6
Also, hemostasis of the surgical wound is specially difficult for patients with hemorrhagic disorders or those undergoing antithrombotic therapy without the suturing of the wound borders. 6-8
Electrobisturi has been applied in the management of oral tissues and provides enhanced hemostasis by sealing blood vessels before cutting. However, cutting performance is harmed by muscle fasciculation, and wound healing is delayed by extensive thermal damage when compared to scalpel surgery.9
High-power LASER have been applied as a useful tool in the management of soft tissue lesions. Surgical LASER have been used to treat oral lesions, including: 1) Potassium Titanyl Phosphate (KTP), 2) neodymium-yttrium-aluminium-gamet (Nd:YAG), 3) carbon dioxide (CO2), and 4) diode LASER with semiconductors. 10 , 11
High-power diode LASER, as compared to other high-power LASER, are more portable, compact, and cost effective. Diode LASER have wavelengths of between 805 and 980nm that can be used in continuous or pulsed mode, according to the clinical recommendation, using an optical fiber with or without contact.12
High-power diode LASER can be applied in the management of oral tissues due to high absorption by water and hemoglobin, thus providing positive results in periodontal surgery, tissue alteration related to orthodontic treatments, and oral lesions. 10 , 13 , 14 Considering that diode LASER surgery may well produce a solid performance in the treatment of oral diseases, including FH, and that prior literature is based on case reports, 7 , 8 the current study aimed to present a prospective case series of FH managed using a high-power diode LASER considering the evaluating of the pain, postoperative functional alterations, edema, secondary infection and bleeding. The objective of this study is to verify if diode LASER surgery is effective to remove FH safetly based on clinical parameters.
Materials and methods
This study was approved by the Ethics Committee of Universidade Federal de Minas Gerais, under protocol number 23083713.1.0000.5149, and informed written consent forms were obtained from all participants. Fifteen patients with FH were recruited from the Oral Medicine Clinic of the Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Brazil from a period of nine months. The selection of cases included patients who presented FH induced either by dentures or by parafunctional habits. Patients with limited-size growths, with flaccid to a fibrous consistency, that were sessil or pedicle,with an erythematous to pale color,and that were associated with dentures or parafuctional habits were enrolled in this study. Dentures were removed 2 weeks before the surgical procedures to eliminate inflammation and/or chronic pain. Patients currently using anti-inflammatory or analgesic medications were excluded.
Topical anesthesia (Emla® AstraZeneca do Brasil LTDA, São Paulo, Brazil or Benzocaine 20%, DFL Indústria e Comércio S. A., Rio de Janeiro, Brazil) was applied to all patients. Infiltrative anesthesia with 2% lidocaine and adrenaline at 1:100.000 (DFL Indústria e Comércio S. A., Rio de Janeiro, Brazil) was applied if the patient complained of any kind of pain. Slight traction of the lesion using mosquito forceps was performed to facilitate the application of the diode LASER incision. Sutures were not performed. The surgical specimens were fixed in 10% buffer formalin and sent for histopathological analysis.
LASER irradiation was performed using an 808nm diode LASER (Thera Lase Surgery, DMC LTDA, São Carlos, Brazil), with an optical fiber of 600 μm, at a power of 2.0W to 3.5W (average 2.96W), in a continuous-wave mode.
The treatment performance of FH with high-power diode LASER was determined by evaluating pain, postoperative functional alterations, edema, secondary infection and bleeding. The patients were asked to separately rate the degree of pain and postoperative functional alterations, which included discomfort during eating and speech,on a 10cm horizontal visual analog scale (VAS) by placing a vertical mark to assess the position between the two endpoints.15 The left endpoint of the pain scale was designated as “no pain, and the right endpoint was marked as unbearable pain.” The end-points of the scales for the degree of discomfort during eating and speech were marked as no discomfort on the left side and unbearable discomfort on the right side. The patients were asked to mark the position between the two endpoints that best described their personal perception of the degree of pain and discomfort during eating and speech that they had experienced on postoperative days 1 and 7. The hatch mark placed by the patient was measured to the nearest centimeter; the scores for the degree of pain and functional complications were between 0 and 10. A single operator recorded these scores on postoperative days 1 and 7. After completion, all recordings were analyzed. All patients were instructed to use the same analgesic medicine containing paracetamol, if needed to alleviate the pain, and were subsequently analyzed. In addition, the patients were asked whether or not an edema was present. Secondary infection was investigated by the presence or absence of local exudation and fever. Bleeding was investigated by its presence or absence. Clinical healing was assessed by the weekly follow-up of the post-operative wounds until they had been completely healed.
All patients underwent special oral hygiene care, especially as regards hot, hard, and acidic foods, during the post-surgical laser period. Patients were instructed not to ingest any form of analgesic during the post surgical period, except in case of unbearable pain.
Results
The clinical profiles of patients and data concerning FH lesions treated with diode LASER surgery are presented in Table 1.
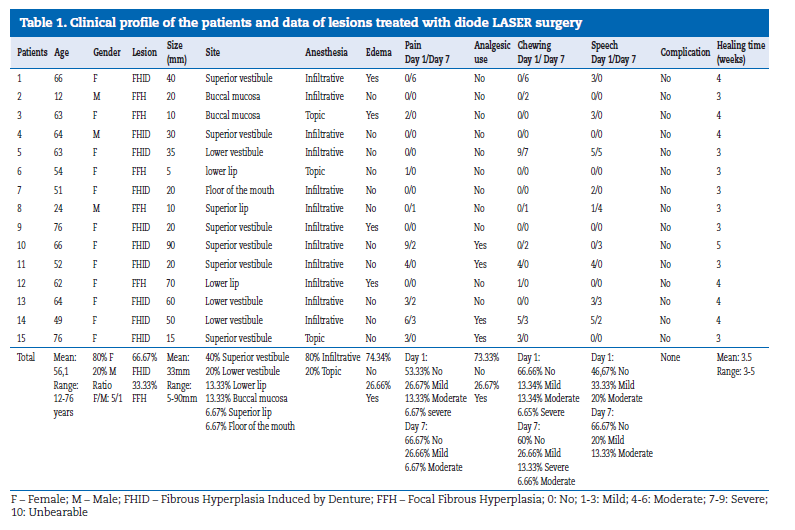
Patient ages ranged from 12 to 76 years (mean 56.13 ± 17.55 years). The study sample consisted of 12 females (80%) and 3 males (20%). Ten (66.67%) patients presented a clinical diagnosis of FH induced by denture (FHID), while five (33.33%) presented a diagnosis of focal FH (FFH). The size of the lesions ranged from 5 to 90 mm (Mean: 33 mm). Six (40%) patients with FHID presented a lesion on the superior vestibule, three (20%) patients presented the lesion on the lower vestibule, and one (6.67%) presented the lesion on the floor of the mouth. Two (13.33%) patients with FFH presented lesions on the buccal mucosa, two (13.33%) on the lower lip, and one (6.67%) on the upper lip. Twelve (80%) patients needed infiltrative anesthesia, while three (20%) needed only topic anesthesia to remove the lesions.All lesions were removed without the need for complementary sutures to control the bleeding during and after diode LASER surgery. No edema was reported by eleven (74.34%) patients, while four (26.66%) reported edema in the postoperative period. The patients classified the intensity of pain on the first postoperative day as no pain in 53.33%, mild in 27.67%, moderate in 13.33% and severe in 6.67%. On day 7, the patients classified the edema as no pain in 66.67%, mild in 26.66%, moderate in 6.66%; no patients reported unbearable pain. Regarding analgesic medication in the postoperative period, twelve (73.33%) patients reported no need for use, while three (26.67%) took an analgesic due to moderate or severe pain. Considering functional alterations during the chewing reported by the patients on the first postoperative day, no discomfort was reported in 66.66% of the cases,mild discomfort in 13.34%, moderate in 13.34%, and severe in 6.65%. On day 7, no discomfort was reported in 60% of the patients, mild discomfort in 26.66%, severe in 13.33%, and moderate in 6.66%. Considering functional alterations during speech reported by the patients on the first post operative day, no discomfort was reported in 46.67%, mild discomfort in 33.33% and moderate in 20%.In the same category, on day 7, no discomfort was reported in 66.67% of the patients, as compared to mild discomfort in 20% and moderate discomfort in13.33%. No patient reported unbearable discomfort. No persistent bleeding or infections could be observed.
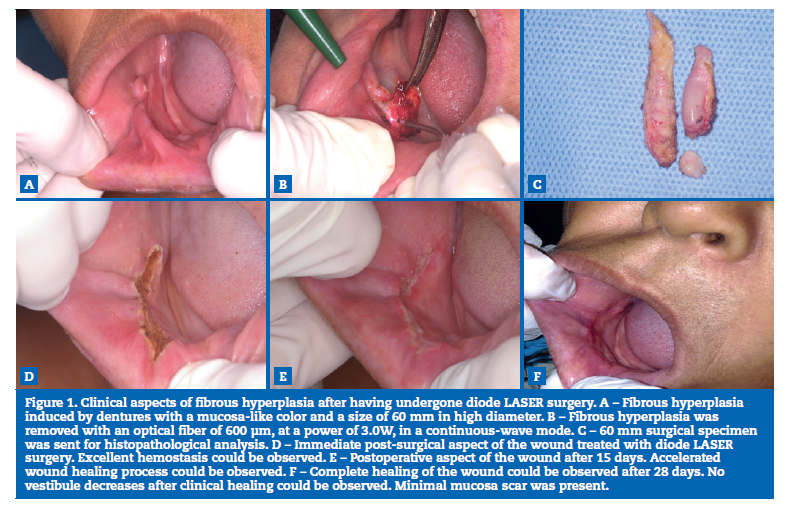
All patients presented a clinical healing of the surgical wounds in a period that ranged from 3 to 5 weeks (mean 3.5 weeks). Regarding patients with a diagnosis of FHID (66.67%), no vestibule decreases could be identified after the clinical healing of the surgical wounds, which left a minimal mucosa scar (Figure 1).
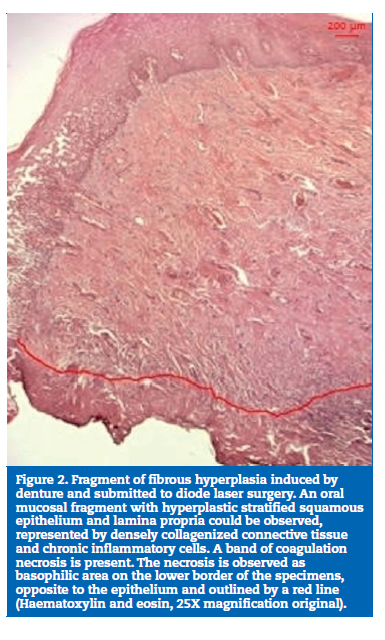
In all specimens, microscopic analysis showed oral mucosal fragments with hyperplastic stratified squamous epithelium, lamina propria of the densely collagenized connective tissue, and chronic inflammatory cells. A band of coagulation necrosis was presented in the lower border of the specimens (opposite to the epithelium) (Figure 2).
Discussion
The current study aimed to verify the performance of diode LASER surgery on the treatment of FH. The main observations included: 1) diode LASER surgery proved to be effective on the treatment of FH, 2) diode LASER surgery shows low postoperative pain and no complications, 3) diode LASER surgery shows low discomfort during chewing and speech in the postoperative period, and 4) there was minimal thermal damage in the treated specimens.
LASER surgery treatment has been used as an adjuvant or substitute to conventional therapies due to several advantages, including cutting, ablation or vaporization, hemostasis, bacterial reduction, and surgical procedures without infiltrative anesthesia. 10 , 17 , 18
Diode LASER is considered a good cutting device for oral tissues.10 However, more tissue damage occurs than with the use of a scalpel,19p> but this damage is not prejudicial to the specimen tissue, specially when the specimens contained a diameter of at least 5 mm.11 In the current study, the tissue damage was minimal, and only one lesion was measured at 5 mm in diameter. In addition, the LASER characteristics and settings, such as power output, wavelength, emission modalities, type of optical fiber, and affinity with target tissues can control the width and severity of the thermal damage caused to the tissue.11 By contrast, diode LASER surgery provides a thermal damage zone of less than 1mm, which allows for surgical precision and excellent hemostasis within a dry operative field.20, 21 Hemostasis caused by LASER surgery is due to the increase in platelet activation at the end point of the wound, which leads to the sealing of the blood vessels.22
Rapid wound healing with diode LASER surgery has been described in prior literature.13 This benefit is related to the photobiomodulation phenomenon, which works at cellular levels by promoting faster healing with a toxin reduction through the accceleration of lymphatic flow, thereby helping to reduce pain, enhance repair, and induce regeneration.13,23 The current results demonstrated that each of the 15 cases of FH treated with diode LASER surgery with specific parameters presented a clinical healing without complications in an average time of 3.5 weeks.
Considering surgical procedures without infiltrative anesthesia, Fornaini et al.24reported the surgical management of oral tissues with only topical anesthesia using diode and Nd:YAG LASER systems. However, Aras et al.18 demonstrated that, when compared with diode LASER, a lower quantity of infiltrative anesthesia was required when using Er:YAG LASER. In the present study, twelve (80%) patients needed infiltrative anesthesia, while three (20%) needed only topic anesthesia to remove the lesions.
Management of oral tissues causes post-operative pain and functional discomfort during chewing and speech.18 Benefits of LASER surgery systems, as compared to the use of scalpels, in decreasing post-operative pain and functional complications have been demonstrated in randomized clinical trials reported in prior literature.25 These benefits may be explained due to the protein coagulum that is formed on the wound surface, thereby acting as a biological dressing, sealing the end of sensory nerves, as well producing photobiomodulation.13
Moreover, less edemas have been reported when using LASER surgery systems, which is related to the sealing of the lymphatic vessels.20,26 In this prospective case series study, the post-operative follow-up was uneventful with no edema in 74.34% of the patients. The majority of patients (73.33%) reported no need to take analgesic medication in the postoperative period. Additionally, the majority of patients reported no or mild pain on postoperative day 1 (80%) and day 7 (93.33%).
Considering functional alterations during chewing, the majority of patients reported no or mild discomfort on postoperative day 1 (80%) and day 7 (86.66%). Regarding functional alterations during speech, the majority of patients reported no or mild discomfort on postoperative day 1 (80%) and day 7 (86.67%).
Despite of this present study seemed to have good internal validity with satisfactory management of FH using high-power diode LASER, the external validity of this findings is poor with this study design due to lack of control group and patients differences.
Conclusions
Diode LASER surgery proved to be effective and presented a satisfactory performance in the treatment of FH. The use of diode LASER surgery allowed for suitable and accurate incisions without requiring sutures, thus decreasing surgery time and maintaining the vestibule fundus in patients with FHID. However, the present study design has limititions to analyze and compare data with other treatment modalities, therefore, randomized clinical trials may be performed to compare diode LASER and other LASER systems with conventional surgery and electrosurgery in the management of FH and other oral lesions.
References
1. Canger EM, Celenk P, Kayipmaz S. Denture-related hyperplasia: A clinical study of a turkish population group. Braz Dent J. 2009;20:243-8.
2. Corbet EF, Holmgren CJ, Philipsen HP. Oral mucosal lesions in 65-year-old Hong Kong Chinese. Community Dent Oral Epidemiol. 1994;22:392-5.
3. Coelho CM, Souza YT, Daré AM. Denture-related oral mucosal lesions in a Brazilian school of dentistry. J Oral Rehabil. 2004;31:135-9.
4. Firoozmand LM, Almeida JD, Cabral LA. Studyof dentureinduced fibrous hyperplasia cases diagnosed from 1979 to 2001.Quintessence Int. 2005;36:825-9.
5. Freitas JB, Gomez RS, De Abreu, MH, Ferreira e Ferreira, E. Relationship between the use of full dentures and mucosal alterations among elderly Brazilians. J Oral Rehabilit. 2008;35:370-4.
6. Keng SB, Loh HS. The treatmentof epulis fissuratum of the oral cavity by CO 2 laser surgery.J Clin Laser Med Surg. 1992;10:303-6.
7. Niccoli-Filho W, Neves ACC, Penna LAP, Seradairian PI, Riva R. Removal of epulis fissuratum associated to vestibuloplasty with carbon dioxide laser. Lasers Med Sci. 1999;14:203-6.
8. Monteiro LS, Mouzinho J, Azevedo A, Câmara MI, Martins MA, La Fuente JM. Treatment of epulis fissuratum with carbon dioxide laser in a patient with antithrombotic medication. Braz Dent J. 2012;23:77-81.
9. Liboon J,Funkhouser W,Terris DJ. A comparison of mucosal incisions made by scalpel, CO2 laser, electrocautery, and constant-voltage electrocautery. Otolaryngol Head Neck Surg. 1997;116:379-85.
10. Romanos G, Nentwig GH. Diode laser (980 nm) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. J Clin Laser Med Surg. 1999;17:193-7.
11. Angiero F,Parma L, Crippa R, Benedicenti S. Diode laser (808 nm) applied to oral soft tissue lesions: a retrospective study to assess histopathological diagnosis and evaluate physical damage. Lasers Med Sci. 2012;27:383-8.
12. Jackson SD, Lauto A. Diode-pumped fiber lasers: a new clinical tool? Lasers Surg Med. 2002;30:184-90.
13. Elanchezhiyan S,Renukadevi R,Vennila K. Comparison of diode laser-assisted surgery and conventional surgery in the management of hereditary ankyloglossia in siblings: a case report with scientific review.Lasers Med Sci. 2013;28:7-12.
14. El-Kholey KE. Efficacy and safety of a diode laser in secondstage implantsurgery: a comparative study. Int J Oral Maxillofac Surg. 2014;43:633-8.
15. Mannion AF, Balagué F, Pellisé F, Cedraschi C. Pain measurement in patients with low back pain. Nature Clin Pract Rheumatol. 2007;3:610-8.
16. Peñarrocha M, Carrillo C, Boronat A, Martí E. Level of satisfaction in patients with maxillary full-arch fixed prostheses: zygomatic versus conventional implants. Int J Oral Maxillofac Implants. 2007,22:769-73.
17. Kara, C. Evaluation of patient perceptions of frenectomy: a comparison of Nd:YAG laser and conventional techniques. Photomed Laser Surg. 2008;26:147-52.
18. Aras MH, Göregen M, Güngörmüs M, Akgül HM.Comparison of diode laser and Er:YAG lasers in the treatment of ankyloglossia. Photomed Laser Surg. 2010;28:173-7.
19. Jin JY, Lee SH, Yoon HJ. A comparative study of wound healing following incision with a scalpel, diode laser or Er,Cr:YSGG laser in guinea pig oral mucosa: A histological and immunohistochemical analysis.Acta Odontol Scand. 2010;68:232-8.
20. Coleton, S. Lasers in surgical periodontics and oral medicine. Dent Clin N Am. 2004;48:937-62.
21. Strauss RA, Fallon SD. Lasers in contemporary oral and maxillofacial surgery. Dent Clin N Am. 2004;48:861–8.
22. Mordon S, Begu S, Buys B, et al. Study of platelet behavior in vivo after endothelial stimulation with laser irradiation using fluorescence in trivital videomicsocopy and PEG-ylated liposome staining. Microvasc. 2002;64:316-25.
23. Bornstein E. Near infra red dental diode lasers. Scientific and photobiologic principles and applications. Dent Today. 2004;23:102-8.
24. Fornaini C, Rocca JP, Bertrand MF, Merigo E, Nammour S, Vescovi P.Nd:YAG and diode laser in the surgicalmanagement of soft tissues related to orthodontic treatment.Photomed Laser Surg. 2007;25:381-92.
25. Haytac MC, Ozcelik O. Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J. Periodontol. 2006;77:1815-9.
26. Cernavin I, Pugatpchew A, De Boer N, Tyas MJ. Laser applications in dentistry: a review of the literature. Aust Dent J. 1994;39:28-32.
Marcio Amaral
E-mail address: marciobrunoamaral@yahoo.com.br, marciobrunoamaral@gmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Funding
Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, #309209/2010-2, #472045/2011-3)
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgments
The authors would like to thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq: #309209/2010-2, #472045/2011-3). RA Mesquita is research fellow of CNPq.
Article history:
Received 17 April 2016
Accepted 13 January 2017
Available online 30 March 2017
