
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
Rev Port Estomatol Med Dent Cir Maxilofac | 2017 | 58 (2) | 126-131
Clinical case
Surgical treatment of Adenomatoid Odontogenic Tumor: A 5-year follow-up
Tratamento cirúrgico de Tumor Odontogénico Adenomatóide: Acompanhamento de 5 anos
a Departamento de Patologia da Faculdade de Odontologia da Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brasil.
b Departamento de Cirurgia da Faculdade Newton Paiva, Belo Horizonte, Minas Gerais, Brasil
Andrea María López Soto - andre17cr@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 58
Issue - 2
Clinical case
Pages - 126-131
Go to Volume
Article History
Received on 11/04/2017
Accepted on 26/06/2017
Available Online on 06/07/2017
Keywords
Case report
Surgical treatment of Adenomatoid Odontogenic Tumor: A 5-year follow-up
Tratamento cirúrgico de Tumor Odontogénico Adenomatóide: Acompanhamento de 5 anos
Henrique Côrtes Meiraa, Igor Figueiredo Pereiraa, Flávia Fonseca Carvalho Soaresa, Aline Fernanda Cruza, Andrea María López Sotoa,*, Vladmir Reimar de Souzab
aDepartamento de Patologia da Faculdade de Odontologia da Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brasil.
b Departamento de Cirurgia da Faculdade Newton Paiva, Belo Horizonte, Minas Gerais, Brasil
http://doi.org/10.24873/j.rpemd.2017.07.018
ABSTRACT
Adenomatoid odontogenic tumor (AOT) is a rare odontogenic tumor with limited growth and usually associated with an unerupted permanent tooth. It is a benign lesion, with a low rate of recurrence after surgical treatment. This is a case report of an 11-year-old female with an asymptomatic tumor growth on the maxilla and palatal displacement of the lateral incisor. A unilocular lesion surrounding the coronal impacted right upper canine and the displacement of premolars were observed radiographically. After incisional biopsy, the tumor was diagnosed as AOT. The enucleation of the lesion and the removal of the impacted canine was performed. Four months later, the patient had not shown any signs of recurrence and was referred for orthodontic treatment. New surgical procedure was performed to remove the gums that covered the premolars to promote their eruption. Five years later, the premolars are in position in the dental arch and there are no signs of recurrence of the lesion. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(2):126-131)
Keywords: Adenomatoid odontogenic tumor,Impacted tooth, Odontogenic tumors, Oral surgery
RESUMO
O tumor odontogênico adenomatóide (TOA) é um tumor raro com crescimento limitado e geralmente associado a um dente permanente não erupcionado. É uma lesão benigna, com baixa taxa de recorrência após tratamento cirúrgico. Relato de caso de uma menina de 11 anos de idade com crescimento tumoral assintomático na maxila e deslocamento palatino do incisivo lateral. Radiograficamente, foi observada uma lesão unilocular em torno da coroa do canino superior direito impactado e deslocamento dos pré-molares. Após a biópsia incisional, o tumor foi diagnosticado como TOA. A enucleação da lesão e do canino impactado foi realizada. Quatro meses depois, o paciente não apresentou sinais de recorrência e foi encaminhado para tratamento ortodôntico. Um novo procedimento cirúrgico foi realizado para remover a gengiva que cobria os pré-molares para promover sua erupção. Após cinco anos, os pré-molares encontram-se em posição no arco dentário e não existem sinais de recorrência da lesão. (Rev Port Estomatol Med Dent Cir Maxilofac. 2017;58(2):126-131)
Palavras-chave: Tumor odontogênico adenomatóide, Dente impactado, Tumores odontogênicos, Cirurgia oral
Introduction
Odontogenic tumors and hamartomas are included in a wide variety of rare lesions that originate from odontogenic tissues and are present at variables levels of differentiation. The determination of its exact nature (i.e., hamartoma or neoplasm)is difficult and often inconclusive, which makes the nomenclature for these types of lesions difficult.1
The Adenomatoid odontogenic tumor (AOT) was first reported in 1907, called the pseudo‑adenoameloblastoma.2 Different nomeclatures have also been used to describe this tumor: adenoameloblastic and ameloblastic adenomatoid tumor. The term Adenomatoid odontogenic tumor, adopted by the World Health Organization classification of odontogenic tumors in 1971, is still the most accepted and currently used nomenclature. 3,4
AOT is a rare and non‑aggressive epithelial odontogenic tumor that occurs in intraosseous and peripheral forms. The intraosseous variants are the most frequent and include follicular and extrafollicular types. Radiographically, the central lesions (intraosseous) appear as a unilocular and radiolucent area, which is well-defined and often associated with an impacted tooth. Two‑thirds of intraosseous cases present radiopacitywithin them.5
This type of lesion corresponds to 2% to 7% of all odontogenic tumors, usually affecting young patients, mostly during their second and third decades of life. Women are affected more often than men (a ratio of 1.9:1.0), and the lesions tend to occur in the anterior maxilla region. 4,6
The aim of this study was to report the surgical management of an AOT, show the results from the five years of follow‑up, and discuss clinical and radiographic aspects with the current literature.
Case report
An 11‑year‑old female patient was referred to the Oral and Maxillofacial Surgery service of the School of Dentistry of the Federal University of Minas Gerais (UFMG), Belo Horizonte, Brazil, presenting a 5‑6‑month history of asymptomatic tumor growth on the right side of the maxilla. There was no history of trauma and the lesion had progressively increased in size in recent months.
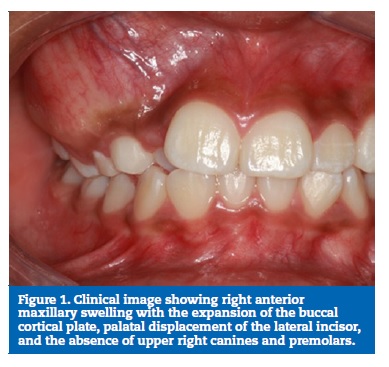
Clinical examination revealed swelling with ill‑defined margins, with normal overlying mucosa, which was firm on palpation. The buccal cortical plate of the right maxilla was expanded from the central incisor to the first molar and palatal displacement of lateral incisor on the same side (Figure 1). Facial asymmetry was not observed upon extra oral examination.
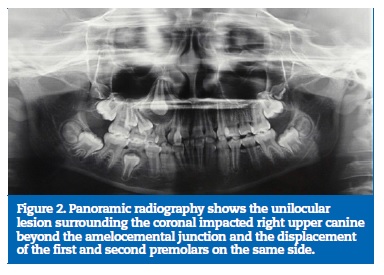
The panoramic radiography showed a well‑defined, unilocular radiolucency in the maxilla associated with the unerupted right upper canine, with no evidence of calcifications or root resorptions. It also showed the displacement of first and second premolars on the same side and a delay in its eruption process (Figure 2). Radiographic and clinical findings were compatible with the diagnosis of dentigerous cyst, AOT, and unicystic ameloblastoma.
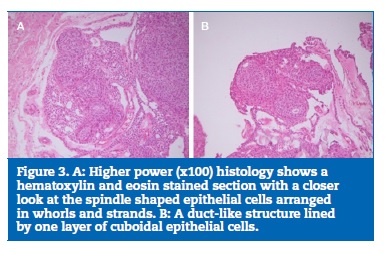
Fine needle aspiration was negative and an incisional biopsy was performed. Histological examination revealed cuboidal or spindle‑shaped epithelial cells forming aggregates or typical rosette‑ like structures with minimal connective tissue, and cuboidal or low columnar cells forming glandular duct‑like structures, confirming the diagnosis of an AOT (Figure 3).
After confirming the diagnosis, the enucleation of the lesion was performed under local anesthesia, together with the removal of the impacted canine and deciduous molars (Figure 4).
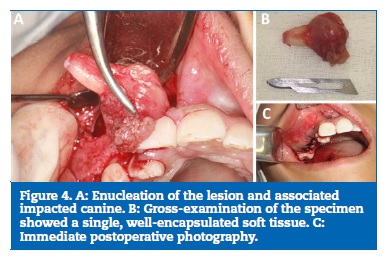
The final diagnosis of an intraosseus follicular variant of AOT was reconfirmed after the specimen had been microscopically examined.
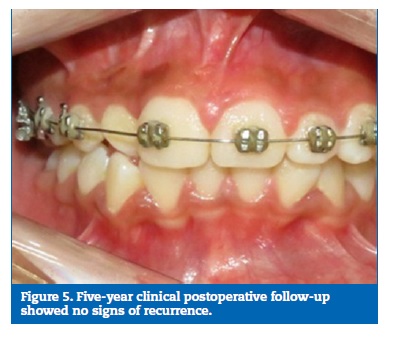
Four months later, the patient showed no signs of recurrence and was referred for orthodontic treatment. A new surgical procedure was performed to remove the gums that covered the premolars and promote their eruption.
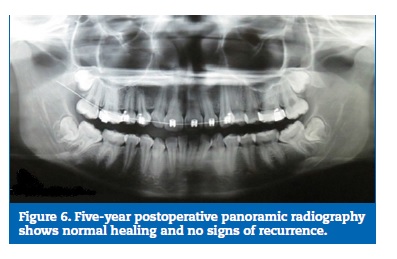
The patient underwent follow‑up and, five years after surgery, has shown no signs of recurrence (Figures 5 and 6).
Discussion
AOT is a rare, hamartomatous, epithelial lesion of odontogenic origin.46 It’s one of the most controversial lesions, due to its histopathological characteristics and similarity to ameloblastoma, thus previously receiving the name of pseudo‑adenomeloblastoma.2 When compared to ameloblastomas, the most common odontogenic tumor, AOT is a nonaggressive tumor, encapsulated with limited growth and no tendency of recurrence. It is usually associated with an unerupted permanent tooth. Radiographically, in most cases, AOT shows a unilocular radiolucency with well‑defined borders and may contain numerous dispersed radiopaque foci.4,7 Except for the absence of calcifications in the lesion, the present case presents the classic characteristics of the lesion.
Neoplastic or hamartous lesions can develop at any stage of a complex process called odontogenesis.8 In relation to the theory about the origin and pathogenesis of AOT, it seems that this tumor is derived from the odontogenic epithelium of the dental lamina complex or its cellular remnants situated in the gubernacular cord.9
The gubernacular cord is a fibrous innerved, vascularized, and lymphatic channel with epithelial cells or cell clusters from the fragmented dental lamina running in a bony channel called the gubernacular canal, which connects the pericoronal follicular tissue of the permanent tooth to the alveolar crest and the palatal gingiva of the deciduous tooth. Some authors conclude that dental lamina in the gubernacular cord of the developing permanent anterior teeth, such as incisors, canines, or premolars, seems to be an embryonic source of more than 96% of AOT.910
A critical review of all case reports of AOT described in the literature between the years of 2012 and 2017 was performed and 56 references were found. However, due to lack of data, 48 cases were included in the analysis.
This type of lesion occurs mainly in the second decade of life, and is rare in patients over 30 years of age. All lesions occurred in the second and third decades11,12 of life, except for two cases13,48 one that affected a 10‑year‑old49 and 50‑year‑old male patient.50 Women are more commonly affected than men, at a ratio of 2:1.11,12 Of all the cases evaluated, 61.9% occurred in female patients,13-34,46-48 The present report shows a case of AOT in an 11‑year‑old female patient.
This lesion is commonly located in the anterior maxilla and rarely in the mandible. It usually surrounds the crown of unerupted teeth, and 60% of the cases are associated with an impacted canine51 as was illustrated in this report. Of all the cases evaluated, only 35.7% affected mandible.13, 15-17, 21,30, 34,35, 43- 45,48 ,49, 52,53 One of these cases presented the peripheral variant of the lesion de peripheral type,53 and another was associated with a deciduous teeth.49
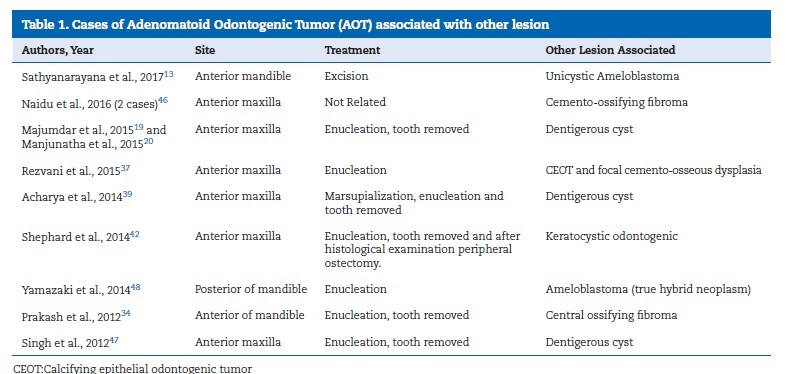
The structure of the cyst, its insertion around the wholetooth, not only in the amelocemental junction of an unerupted element, and the size of the buccal cortical expansion were not so typical of a dentigerous cyst. However, there are case reports in dental literature of AOT arising in association with other lesions (Table 1); therefore, it requires an indispensable meticulous histopathological evaluation. 54,55
The management of this tumor should be surgical. Enucleation of the lesion and removal of the impacted tooth and simple curettage is recommended, although there is a report of the preservation of the associated tooth, together with surgical and orthodontic treatment. 12 Of the cases reviewed, one was treated with marsupialization with subsequent39 enucleation and in another there was preservation of the associated tooth 15. The prognosis is excellent and the recurrence rate is 0.2%.55
Conclusion
The treatment of choice for ATO is its surgical removal by enucleation and removal of the associated tooth when present.
Despite a good prognosis and a low risk of recurrence, a clinical and radiographic follow‑up of patients should be performed.
In addition, the patient should receive multidisciplinary treatment from various dental specialties in the rehabilitation of the space caused by the lost tooth.
References
1. Gomez RS, Castro WH, Gomes CC, Loyola AM. Adenomatoid odontogenic tumor associated with odontoma: a case report and critical review of the literature. Head Face Med. 2013;9:20.
2. Khot K, Vibhakar PA. Mural Adenomatoid Odontogenic Tumor in the Mandible – A Rare Case. Int J Maxillofac Pathol. 2011;2:35-9.
3. Ide F, Muramatsu T, Ito Y, Kikuchi K, Miyazaki Y, Saito I, et al. An expanded and revised early history of the adenomatoid odontogenic tumor. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:646-51.
4. Seo WG, Kim CH, Park HS, Jang JW, Chung WY. Adenomatoid odontogenic tumor associated with an unerupted mandibular lateral incisor: a case report. J Korean Assoc Oral Maxillofac Surg. 2015;41:342-5.
5. Narayanan VS, Naidu G, Ragavendra R, Mhaske‑Jedhe S, Haldar M. Adenomatoid odontogenic tumor of the mandible with unusual radiographic features: A case report. Imaging Sci Dent. 2013;43:111-5.
6. Philipsen HP, Reichart PA, Siar CH, Ng KH, Lau SH, Zhang X, et al. An updated clinical and epidemiological profile of the adenomatoid odontogenic tumour: a collaborative retrospective study. J Oral Pathol Med. 2007;36:383-93.
7. Lee SK, Kim YS. Current concepts and occurrence of epithelial odontogenic tumors: I. Ameloblastoma and adenomatoid odontogenic tumor. Korean J Pathol. 2013;47:191-202.
8. Sandhu S V, Narang RS, Jawanda M, Rai S. Adenomatoid odontogenic tumor associated with dentigerous cyst of the maxillary antrum: A rare entity. J Oral Maxillofac Pathol. 2010;14:24-8.
9. HP, Khongkhunthiang P, Reichart PA. The adenomatoid odontogenic tumour: An update of selected issues. J Oral Pathol Med. 2016;45:394‑8.
10. Ide F, Mishima K, Kikuchi K, Horie N, Yamachika S, Satomura K, et al. Development and Growth of Adenomatoid Odontogenic Tumor Related to Formation and Eruption of Teeth. Head Neck Pathol. 2011;5:123-32.
11. Rashmi G, Santosh G, Praveen KM. Adenomatoid odontogenic tumour. Indian J Dent Adv. 2009;1:67-71.
12. Motamedi MH, Shafeie HA, Azizi T. Salvage of an impacted canine associated with an adenomaoid odontogenic tumour: a case report. Br Dent J. 2005;199:89-90.
13. Sathyanarayana VK, Srigiri H, Cheemalavagupalli M, Vankadara S, Malika G. A Rare Case of Adenomatoid Odontogenic Tumour with Unicystic Ameloblastoma. J Clin Diagn Res. 2017;11:ZJ05‑ZJ06.
14. Dhirawani RB, Pathak S, Mallikaarjuna K, Sharma A. An adenomatoid odontogenic tumor in disguise. Pan Afr Med J. 2016;34:291-3.
15. Erdur EA, Ileri Z, Ugurluoglu C, Cakir M, Dolanmaz D. Eruption of an impacted canine in an adenomatid odontogenic tumor treated with combined orthodontic and surgical therapy. Am J Orthod Dentofac Orthop. 2016;149:923-7.
16. Rosa AC, Soares AB, Furuse C, Lima SR, de Araujo VC, Passador‑Santos F. A Combined Epithelial Odontogenic Tumor? A 7‑Year Follow‑Up Case. Head Neck Pathol. 2016; Epub ahead of print. doi:10.1007/s12105‑016‑0767‑9
17. Sethi S, Kumar M, Aggarwal P, Indra Kumar HS, Sugandhi CD, Singh S. A case report and short review on changing trends in the site of occurrence of adenomatoid odontogenic tumor: Unravelling the past 15 years. Dent Res J. 2016;13:462-71.
18. Kalia V, Kalra G, Kaushal N, Sharma V, Vermani M. Maxillary adenomatoid odontogenic tumor associated with a premolar. Ann Maxillofac Surg. 2015;5:119-22.
19. Majumdar S, Uppala D, Rao AK, Talasila S, Babu M. Dentigerous Cyst Associated with Adenomatoid Odontogenic Tumour. J Clin Diagn Res. 2015;9:ZD01‑4.
20. Manjunatha BS, Mahajan A, Mody BM, Shah V. Adenomatoid Odontogenic Tumor (AOT) Arising from a Dentigerous Cyst: Literature Review and Report of a Case. J Maxillofac Oral Surg. 2015;14:393-7.
21. Jindal C, Sarkar RB, Grewal J, Grewal R, Bansal A. Mural adenomatoid odontogenic tumour as anterior mandibular swelling: a diagnostic challenge. J Clin Diagn Res. 2014;8:ZD25‑7.
22. Marrelli M, Pacifici A, Di Giorgio G, Cassetta M, Stefanelli L V, Gargari M, et al. Diagnosis and treatment of a rare case of adenomatoid odontogenic tumor in a young patient affected by attenuated familial adenomatosis polyposis (aFAP): case report and 5 year follow‑up. Eur Rev Med Pharmacol Sci. 2014;18:265-9.
23. Mohanty N, Routray S, Swain N, Ingale Y. Adenomatoid odontogenic tumor with clear cell changes. Indian J Pathol Microbiol. 2014;57:290-3.
24. Virupakshappa D, Rajashekhara BS, Manjunatha BS,
Das N. Adenomatoid odontogenic
tumour in a 20‑ 25. Angiero F, Crippa R. Adenomatoid odontogenic tumor: a case report with immunohistological
profile. Anticancer Res. 2013;33:2673-7. 26. Lavanya N, Rajeshwari MR, Bharathi R, Shaheen A. Peripheral adenomatoid
odontogenic tumour – is it
really peripheral?: a case report. J Clin Diagn Res. 2013;7:1524-6. 27. Prakasam M, Tiwari S, Satpathy M, Banda VR. Adenomatoid odontogenic tumour. BMJ
Case Rep. 2013;2013: bcr2013010212. 28. Agarwal A, Giri KY, Alam S. The
interrelationship of adenomatoid odontogenic
tumour and dentigerous
cyst: a report of a rare case and review of the literature. Case Rep Pathol. 2012;2012:358609. 29. Mutalik V, Mutalik S, Shreshtha A, Radhakrishnan R. Adenomatoid odontogenic tumor: A unique report with histological
diversity. J Oral Maxillofac Pathol. 2012;16:118-21. 30. Sharma N, Passi S, Kumar
V. Adenomatoid odontogenic tumor:
As an unusual mandibular manifestation. Contemp Clin Dent. 2012;3:29-32. 31. Shreedhar B, Ali I, Agarwal A, Alam S. A huge adenomatoid odontogenic
tumor of maxilla. Case Rep Med. 2012;2012:317341. 32. Vasudevan K, Kumar S, Vijayasamundeeswari, Vigneswari
S. Adenomatoid odontogenic
tumor, an uncommon tumor. Contemp Clin Dent. 2012;3:245-7. 33. Li B, Xie X‑Y, Jia S‑ 34. Prakash AR, Reddy PS, Bavle RM, Rajanikanth. Concomitant occurrence of cemento‑ossifying
fibroma and adenomatoid odontogenic
tumor with bilateral impacted permanent canines in the mandible. Indian
J Dent Res. 2012;23:434-5. 35. Belgaumi UI, Parkar MI, Malik NA, Suresh K V, Havewala
AM, Bhalinge PM. Follicular Adenomatoid
Odontogenic Tumor in Mandible: A Rare Case Report.
Ann Med Heal Sci Res. 2015;5:469-72. 36. Jindwani K, Paharia Y, Singh Kushwah A.
Surgical management of peripheral variant of adenomatoid
odontogenic tumor: A rare case report with review. Contemp Clin Dent. 2015;6:128-30. 37. Rezvani G, Donoghue M, Reichart PA, Pazuhi N. Case Presentation
of Concomitant and Contiguous Adenomatoid Odontogenic Tumor and Focal Cemento‑Ossifying Dysplasia. Open Dent J. 2015;9(Suppl
2: M14):340-5. 38. Grover S, Rahim AM, Parakkat NK, Kapoor S, Mittal K,
Sharma B, et al. Cystic Adenomatoid Odontogenic Tumor. Case Rep Dent. 2015;2015:2-6. 39. Acharya S, Goyal A, Rattan V, Vaiphei K,
Bhatia SK. Case Report Dentigerous Cyst or Adenomatoid Odontogenic Tumor :
Clinical Radiological and Histopathological Dilemma. Case
Rep Med. 2014;2014:1–5. 40. Krishnamurthy K, Balaji
R, Devadiga S, Prasad RG. Adenomatoid
odontogenic tumor in the maxillary antrum: A rare case entity. J Pharm Bioallied
Sci. 2014;6(Suppl 1):S196‑9 41. Moon JW. Extensive Adenomatoid
Odontogenic Tumor of the Maxilla: A Case Report of
Conservative Surgical Excision and Orthodontic Alignment of Impacted Canine. Maxillofac Plast Reconstr Surg. 2014;36:173-7. 42. Shephard M, Shepard M,
Coleman H. Simultaneous adenomatoid odontogenic and keratocystic odontogenic tumours in a patient
with Gorlin‑ Goltz syndrome. Aust Dent J. 2014;59:121-4. 43. Bhatt R, Dave J, Nalawade
TM, Mallikarjuna R. Adenomatoid
odontogenic tumour in
mandible in a 14‑year‑old boy. BMJ Case Rep. 2013;2013:
bcr2013010287. 44. Saluja R, Kaur G, Singh P. Aggressive adenomatoid
odontogenic tumor of mandible showing root resorption: A histological case report. Dent Res J. 2013;10:279-82. 45. Shivali V, Pandey A, Khanna VD, Khanna P, Singh A, Ahuja T. A
Rare Case of Extrafollicular Adenomatoid
Odontogenic Tumour in the
Posterior Region of the Mandible: Misdiagnosed as Residual Cyst. J Int Oral Heal. 2013;5:123-8. 46. Naidu A, Slater LJ, Hamao‑Sakamoto A, Waters P, Kessler HP, Wright JM. Adenomatoid
odontogenic tumor with peripheral cemento‑osseous reactive proliferation: report of 2 cases and review of the
literature. Oral Surg Oral Med Oral
Pathol Oral Radiol.
2016;122:e86‑92. 47. Singh V, Goyal S, Sheikh
S, Shambulingappa P, Singh B, Singh R. Adenomatoid odontogenic tumor
with dentigerous cyst: Report of a rare case with
review of literature. Contemp Clin Dent. 2012;3:244-7. 48. Yamazaki M, Maruyama S, Abe T, Babkair
H, Fujita H, Takagi R, et al. Hybrid ameloblastoma
and adenomatoid odontogenic
tumor: Report of a case and review of hybrid variations in the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:1-7. 49. Lee JS, Yoon SJ, Kang BC, Kim OJ, Kim YH. Adenomatoid odontogenic tumor
associated with unerupted first primary molar. Pediatr Dent. 2012;34:493-5. 50. Reddy Kundoor VK, Maloth KN, Guguloth NN, Kesidi S. Extrafollicular Adenomatoid Odontogenic Tumor: An
Unusual Case Presentation. J Dent. 2016;17:370-4. 51. Dayi E, Gurbuz G, Bilge OM, Ciftciog lu MA. Adenomatoid odontogenic tumour (adenoameloblastoma). Case report and review of the
literature. Aust Dent J. 1997;42:315-8. 52. Oliveira M, Gabrielli M, Gabrielli M, Andrade
C, Silva B, Pereira‑Filho V. Unusual Adenomatoid Odontogenic Tumor. J Craniofac Surg. 2016;27:e139-41. 53. Kumar R, Singh RK, Pandey
RK, Mohammad S. Peripheral adenomatoid odontogenic tumor: report of a rare case. J Oral Biol Craniofac Res. 2012;2:57-60. 54. Durga Sreenivas S, Sree Lalita C, Harsha
G, Rao C V. Multiple Pathology in a Single Lesion:
AOT Associated with Dentigerous Cyst. J Maxillofac Oral Surg. 2015;14(Suppl 1):215-21. 55. John JB, John RR. Adenomatoid
odontogenic tumor associated with dentigerous
cyst in posterior maxilla: A case report and review of literature. J Oral Maxillofac Pathol.
2010;14:59-62. Andrea Maria Lopez Soto E-mail address: andre17cr@hotmail.com Ethical disclosures Protection of human and animal subjects. The
authors declare that the procedures followed were in accordance with the regulations
of the relevant clinical research ethics committee and with those of the Code
of Ethics of the World Medical Association (Declaration of Helsinki). Confidentiality of data. The
authors declare that they have followed the protocols of their work center on
the publication of patient data. Right to privacy and informed consent. The
authors have obtained the written informed consent of the patients or subjects mentioned
in the article. The corresponding author is in possession of this document. Conflicts of interest The
authors have no conflicts of interest to declare. Acknowledgements We offer our deepest thanks to the institutions that
provided technical support for the development and implementation of this study. Article history: Received 11 April 2017 Accepted 26 June 2017 Available online 6 July 2017
