
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial | 2023 | 64 (4) | 170-180
Case report
Facial asymmetry correction with surgical-orthodontic treatment: Challenges of the surgical and postsurgical phases
Tratamento ortodôntico-cirúrgico na correção da assimetria facial: Desafios das fases cirúrgica e pós-cirúrgica
a Department of Orthodontics, School of Dentistry, University of Lisbon, Lisbon, Portugal
Sara Palmares - sarapalmares.ortodontia@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 64
Issue - 4
Case report
Pages - 170-180
Go to Volume
Article History
Received on 19/07/2023
Accepted on 03/12/2023
Available Online on 30/01/2024
Keywords
Clinical Case Report
Facial asymmetry correction with surgical-orthodontic treatment: Challenges of the surgical and postsurgical phases
Tratamento ortodôntico-cirúrgico na correção da assimetria facial: Desafios das fases cirúrgica e pós-cirúrgica
Sara Palmares1* 0000-0001-9711-2858
Rui Pereira1 0000-0002-6544-5786
1 Department of Orthodontics, School of Dentistry, University of Lisbon, Lisbon, Portugal
Article history:
Received 19 July 2023
Accepted 3 December 2023
Available online 30 December 2023
Abstract
Asymmetry is commonly diagnosed in orthodontic clinical practice and is more or less perceived depending on its severity. In more severe cases, orthodontic-surgical treatment is the only treatment option. Although presurgical orthodontics is fundamental, occasionally, the occlusion obtained after surgery is far from that planned, and the orthodontist must decide between surgical re-intervention or orthodontic finishing. This clinical report describes the case of an 18-year-old man, presenting a severe facial asymmetry with class III malocclusion, who underwent a surgical-orthodontic treatment. One week after orthognathic surgery, the patient was reoperated because the intercuspation was different from the one obtained at the end of surgery. However, after the second surgery, the intercuspation was still far from what was planned. Despite that, at the end of treatment, a functional and stable occlusion was obtained, associated with a significant improvement in facial harmony and function.
Keywords: Class III,Facial asymmetry,Orthodontics,Orthognathic surgery
Resumo
A assimetria facial é diagnosticada frequentemente na prática clínica ortodôntica, sendo mais ou menos percecionada consoante a severidade. Nos casos severos, o tratamento ortodôntico-cirúrgico é a única possibilidade terapêutica. Uma correta preparação ortodôntica é fundamental, contudo, ocasionalmente o resultado obtido com a cirurgia não é o programado e o clínico tem de decidir entre a re-intervenção cirúrgica ou o acabamento ortodôntico. Este trabalho descreve o caso de um paciente com 18 anos de idade, com classe III e assimetria mandibular severa, que foi submetido a um tratamento
ortodôntico-cirúrgico. Uma semana após a cirurgia ortognática, o paciente foi re-intervencionado por a oclusão não ser a obtida no pós-operatório imediato. Contudo, mesmo após a segunda intervenção, a oclusão não foi a esperada. No entanto, no final do tratamento obteve-se uma oclusão funcional e estável, associada a uma melhoria significativa da harmonia facial e da função.
Palavras-chave: Classe III, Assimetria facial,Ortodontia,Cirurgia ortognática
Introduction
Asymmetry is commonly diagnosed in orthodontic clinical practice and is more or less perceived depending on its severity.
It has been reported that all individuals have some craniofacial asymmetry, including those perceived as “normal”.1
Particularly, mandibular and chin point asymmetry are potentially important factors in the perception of facial attractiveness.2, 3 Deviations in the mandible are known as the most striking characteristic of disharmony, particularly the lateral displacement of the chin from the midsagittal plane.4 These deviations can have important psychological, functional, and aesthetic implications for patients, potentially affecting their self-esteem and quality of life.5, 6
The accurate diagnosis of asymmetries is fundamental and must be based on clinical examination, photographic analysis, and radiographs. Traditionally, two-dimensional cephalometric radiographs were used.7 Nowadays, diagnosis and treatment planning of facial asymmetry can be performed through quantitative measurement of three-dimensional computed tomography (CT) images.2, 8
Small facial asymmetries are common, and conventional orthodontic treatment is generally effective in correcting them. However, orthodontic-surgical treatment is needed in more severe cases to ensure better functional and aesthetic results.9 – 12
Occasionally, the occlusion obtained after surgery is far from that planned, and the orthodontist must decide between surgical re-intervention or orthodontic finishing, as reported in this case.
Case report
An 18-year-old man visited the Orthodontic Department at the University of Lisbon, in Portugal, referred by a maxillofacial surgeon, with chief complaints of facial asymmetry. He reported no problems in his medical history but mentioned left temporomandibular joint (TMJ) clicking and an episode of right TMJ locking, without indicating pain. The patient said he was run over by a car when he was 5 years old and suffered multiple traumas.
Examination and pretreatment facial photographs showed a facial asymmetry with chin deviation to the left side, an increased lower facial height, and a straight profile (Figure 1). A counterclockwise (CCW) canting of the occlusal plane and transversal and vertical asymmetry of oral commissures were also observed. The maxillary dental midline deviated 2.0 mm to the right from the facial midline, and the mandibular dental midline deviated 9.0 mm to the left from the facial midline. No discrepancies between centric relation and centric occlusion were detected.

Figure 1. Pretreatment facial photographs.
Intraoral photographs and study casts (Figures 2 and 3) showed moderate crowding in the maxillary arch and severe crowding in the mandibular arch, and a molar and canine Class III relationship (-7 mm and -2 mm from the Class I position on the right and left sides, respectively). The overjet and overbite were -1 to 1 mm. Despite excessive lingual crown torque of the mandibular left posterior teeth, there was a posterior crossbite on the left side. An anterior crossbite was also present. Regarding the intra-arch sagittal symmetry, there was a mesial positioning of the left posterior teeth in the maxilla and a mesial positioning of the right posterior teeth in the mandible. In relation to the transversal symmetry, the left maxillary hemiarch was wider than the right hemiarch.

Figure 2. Pretreatment intraoral photographs.

Figure 3. Pretreatment study casts.
There was left TMJ clicking during mouth opening. Several interferences on the working and non-working sides were detected due to the absence of canine guidance. All teeth, except the maxillary right first molar, were present. Maxillary third molars were fully erupted, and the mandibular ones were partially erupted and impacted on the distal side of the mandibular second molars. No caries or other pathologies were observed, and the periodontal tissues were healthy.
The CT images showed the extent of the mandibular skeletal asymmetry, which involved a chin deviation of 9.0 mm to the left (Figure 4). The lateral cephalometric analysis indicated a skeletal Class III pattern, resulting from both a slight retrognathic maxilla and a prognathic mandible, and a hyperdivergent pattern (Figure 5; Table 1). The proclined maxillary and retroclined mandibular incisors represented a typical dentoalveolar compensation for a skeletal Class III malocclusion. The panoramic radiograph (OPG) showed an asymmetry in shape between the left and right temporomandibular joints (Figure 6). No family history of maxillary deficiency or mandibular prognathism was reported.

Figure 4. Pretreatment computed tomography images.

Figure 5. Pretreatment radiograph: lateral cephalogram.
Table 1. Cephalometric analysis at pretreatment and Posttreatment

Ui – Upper incisor; Li – Lower incisor; SD – standard deviation.

Figure 6. Pretreatment radiograph: panoramic radiograph.
The following treatment objectives were established: 1) correct the maxilla and mandible discrepancy to obtain a harmonious and pleasant facial appearance, 2) correct the maxillary canting and mandibular asymmetry to achieve facial symmetry, 3) reduce lower anterior facial height, 4) achieve a Class I canine occlusion with a normal overjet and overbite, 5) achieve coincident skeletal and dental midlines, 6) coordinate the maxillary and mandibular arch forms, 7) resolve crowding and align the teeth, and 8) achieve occlusal stability and normal function. Because of the severe mandibular asymmetry, surgical
jaws correction was the only valid treatment approach for achieving these objectives. Therefore, the treatment plan consisted of orthodontic treatment with three premolars extraction, incisors and lateral segments decompensation, and a two-jaw surgery approach: a LeFort 1 osteotomy with maxillary advancement and asymmetric impaction on the frontal plane and a bilateral sagittal split ramus osteotomy (BSSO) with asymmetric setback of the mandible.
An orthodontic treatment without orthognathic surgery would not successfully correct the skeletal discrepancy, the functional balance, and the facial asymmetry. Therefore, bimaxillary orthognathic surgery was inevitable. Since the facial asymmetry affected both the mandible and the maxilla, the possibility of having single-jaw surgery with only a mandibular setback was rejected. The premolar extraction was planned due to crowding and sagittal asymmetry of both arches. The extraction of the mandibular first molars was rejected due to the lower third molars’ inclination and the extended treatment time that would be required to close the space and upright these molars.
The initial phase of treatment involved bonding of 0.018-in slot fixed orthodontic appliances on all teeth (Figure 7) and extraction of teeth 25, 35, 45, 28, and 38. Orthodontic alignment and leveling of the maxillary and mandibular dental arches were performed with 0.014-in and 0.016-in nickel-titanium archwires. Subsequently, 0.016 x 0.022-in stainless-steel archwires were placed, and space was created for teeth 12, 32, and 33 with nickel-titanium open coils (Figure 8). The remaining spaces were closed with power chains. Class II intermaxillary elastics were used to prevent retroinclination of the lower incisors
when closing spaces and to increase the surgical movement’s magnitude (Figure 9). Arch coordination was evaluated through progress study casts (Figure 10).

Figure 7. Presurgical intraoral photographs of treatment progress (bonding appointment).

Figure 8. Presurgical intraoral photographs of treatment progress (routine appointment number 4).

Figure 9. Presurgical intraoral photographs of treatment progress (routine appointment number 11).

Figure 10. Presurgical study casts simulating postsurgical occlusion.
After 14 appointments, the patient was referred for orthognathic surgery (Figures 11, 12, and 13). The surgical procedure included a 2-mm maxillary advancement with asymmetric maxillary impaction (4 mm and 2 mm on the right and left side, respectively), and a BSSO with an asymmetric setback of the mandible (10 mm ostectomy on the right side) was performed.
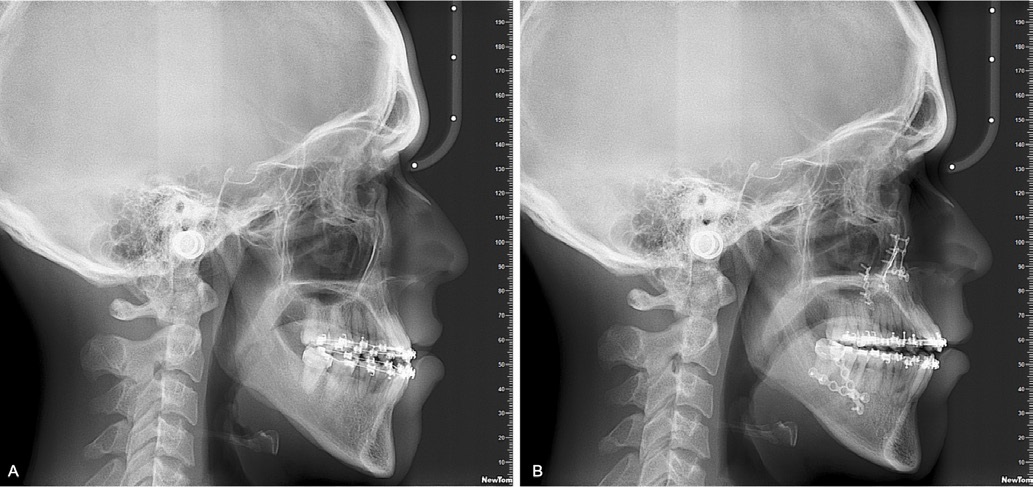
Figure 11. Lateral cephalograms: A) at the end of the presurgical phase; B) after the second orthognathic surgery.

Figure 12. Presurgical facial photographs (patient ready for surgical phase).

Figure 13. Presurgical intraoral photographs (patient ready for surgical phase).
Four days after the surgery (Figure 14), the surgical team decided to reoperate the patient because the intercuspation was different from the one obtained at the end of surgery.

Figure 14. Postsurgical intraoral photograph of treatment progress (after the first surgery).
However, one week after the second surgery, the intercuspation was still far from the study casts’ simulated occlusion (Figure 10). Moreover, the patient presented a 2-mm anterior open bite (Figure 11) with no contacts from cuspid to cuspid, a 2-mm deviation of the mandible to the previous asymmetry, and a 2-mm Class III relationship on the right side. He was asked to use vertical intermaxillary elastics on both sides and Class III elastics on the right side (Figure 15). A few weeks later, his occlusion showed improvement. Finishing and detailing were done with intermaxillary elastics and springs on 0.016 x 0.022-in stainless-steel wires (Figure 16). Before the end of the treatment, the patient returned to surgery to remove the mandibular right fixation plate due to discomfort, and a genioplasty was performed at the same time.
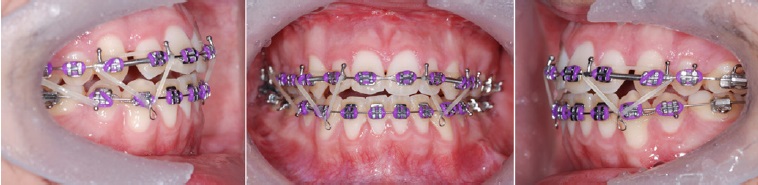
Figure 15. Postsurgical intraoral photographs of treatment progress (after the second surgery).

Figure 16. Postsurgical intraoral photographs of treatment progress (routine appointment number 27).
After 34 appointments of active treatment, fixed appliances were removed (Figures 17 and 18). Maxillary and mandibular fixed retainers were fabricated with 0.0215-in coaxial wire and bonded from the left lateral incisor to the right lateral incisor and from the left canine to the right canine, respectively. The maxillary arch was also retained with a Hawley-type removable appliance, and the patient was instructed to use it for 12 hours in the first six months and then only at night. At the end of active treatment, aesthetic and functional results were achieved. The occlusion was finished with Class I canine on both sides, Class III molar on the right, and Class I molar on the left (Figures 17 and 18). Overbite and overjet were ideal, and maxillary and mandibular dental midlines coincided with the facial midline. The patient’s facial appearance improved significantly with symmetrical smile, oral commissures, and mandible (Figure 19).

Figure 17. Posttreatment intraoral photographs.
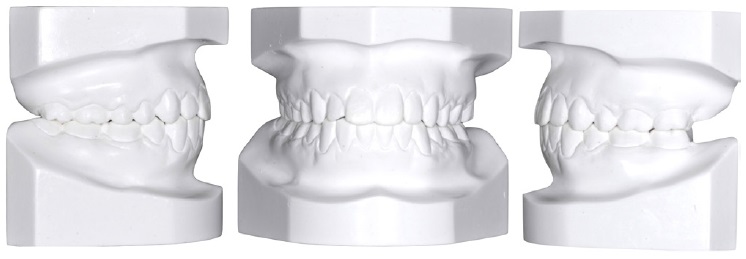

Figure 19. Posttreatment facial photographs.
Cephalometric measurements (Table 1) showed that skeletal and dental objectives were achieved. Cephalometric superimpositions (Figure 20) of pretreatment and posttreatment radiographs showed that, at surgery, the maxillary impaction occurred only anteriorly, promoting a CCW rotation of the palatal plane and a skeletal open bite.
On the posttreatment OPG, external apical root resorptions (EARRs) were detected on maxillary and mandibular anterior teeth (Figure 21). There were no clinical symptoms or signs regarding the TMJ.
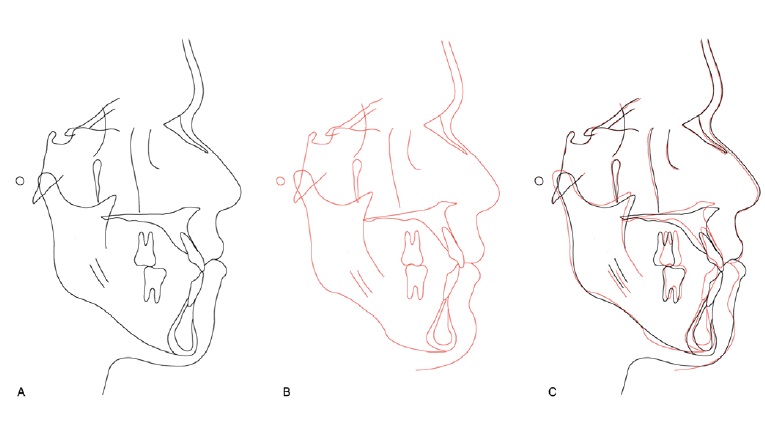
Figure 20. Tracing and superimposition of lateral cephalograms at pretreatment (black) and posttreatment (red): A) initial tracing; B) final tracing; C) superimposition of A and B.

Figure 21. Posttreatment panoramic radiograph.
Discussion and conclusions
The patient presented maxillary and mandibular dental and arch compensations on both sagittal and transverse planes, the first due to the skeletal Class III and the second probably due to the development of asymmetry during his growth.7, 10, 13
The primary goal of presurgical orthodontic treatment is to eliminate dental compensations for the skeletal deformity,7, 10, 14, 15 thus achieving a stable occlusal relationship and ensuring stability after surgery.7, 15 If the preoperative orthodontic treatment does not correct the transverse dental compensation, the facial asymmetry will remain, even if the surgery produces satisfactory occlusion.10, 16, 17 The patient facial asymmetry was more pronounced in the mandible than the maxilla, which agrees with the study by Haraguchi.4
In orthognathic surgery, various intraoperative and postoperative complications may occur. Unfortunately, predicting which patients will experience a specific complication is impossible.18 In this case report, at the end of the surgery, there was an anterior open bite and the increased lower facial height remained. This situation led to extending the postsurgical phase by months. Postsurgical malocclusion is not uncommon and becomes readily evident in the early postoperative period.
Minimal early relapsing can often be managed by intermaxillary elastics and/or orthopedic appliances. A more significant recurrence of the initial preoperative occlusion requires a new surgery. In most circumstances, early relapse occurs as a result of one or more of the following: inadequate mobilization of the repositioned jaws; bony interferences and instability not appreciated during the repositioning; condyles dislodged from the glenoid fossa at the time of fixation; and failure of the internal plate/screw fixation systems.19
On posttreatment OPG, EARRs were detected on maxillary and mandibular anterior teeth, probably due to the increased treatment time,20 or individual susceptibility.21, 22 It is important to highlight that OPG has been shown to overestimate the amount of tooth loss by 20% or more compared with periapical radiographs.23
All skeletal and dental parameters seem to suggest stability, except for overbite, which is expected to decrease slightly due to the orthodontic postsurgical extrusion of the incisors in order to adjust the occlusion.24
Despite the occlusion obtained after surgery, the final intercuspation was excellent, and the patient was very satisfied with his appearance and normal oral function.
References
1. McAvinchey G, Maxim F, Nix B, Djordjevic J, Linklater R, Landini G. The perception of facial asymmetry using 3-dimensional simulated images. Angle Orthod. 2014;84:957-65.
2. Hwang HS, Hwang CH, Lee KH, Kang BC. Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop. 2006;130:779-85.
3. Naini FB, Donaldson ANA, McDonald F, Cobourne MT. Assessing the Influence of Asymmeftry Affecting the Mandible and Chin Point on Perceived Attractiveness in the Orthognathic Patient, Clinician, and Layperson. J Oral Maxillofac Surg. 2012;70:192-206.
4. Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002;72:28-35.
5. Macgregor FC. Social and psychological implications of dentofacial disfigurement. Angle Orthod. 1970;40:231-3.
6. Shackelford TK, Larsen RJ. Facial asymmetry as an indicator of psychological, emotional, and physiological distress. J Pers Soc Psychol. 1997;72:456-66.
7. Tyan S, Park HS, Janchivdorj M, Han SH, Kim SJ, Ahn HW. Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism. Angle Orthod. 2016;86:421-30.
8. Nur RB, Çakan DG, Arun T. Evaluation of facial hard and soft tissue asymmetry using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2016;149:225-37.
9. Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod. 1994;64:89-98.
10. Burstone CJ. Diagnosis and treatment planning of patients with asymmetries. Semin Orthod. 1998;4:153-64.
11. Tai K, Park JH, Ikeda K, Nishiyama A, Sato Y. Severe facial asymmetry and unilateral lingual crossbite treated with orthodontics and 2-jaw surgery: 5-year follow-up. Am J Orthod Dentofacial Orthop. 2012;142:509-23.
12. Lisboa CO, Borges MS, Medeiros PJD, Motta AT, Mucha JN. Orthodontic-surgical retreatment of facial asymmetry with occlusal cant and severe root resorption: A 3-year follow-up. Am J Orthod Dentofacial Orthop. 2017;152: 268-80.
13. Kusayama M, Motohashi N, Kuroda T. Relationship between transverse dental anomalies and skeletal asymmetry. Am J Orthod Dentofacial Orthop. 2003;123:329-37.
14. Proffit WR, White RP Jr. Surgical-Orthodontic Treatment. St Louis: Mosby Year Book; 1991.
15. Sekiya T, Nakamura Y, Oikawa T, Ishii H, Hirashita A, Seto K. Elimination of transverse dental compensation is critical for treatment of patients with severe facial asymmetry. Am J Orthod Dentofacial Orthop. 2010;137:552-62.
16. Epker BN, Stella JP, Fish LC. Dentofacial Deformities: Integrated Orthodontic and Surgical Correction. 2nd ed. St Louis: Mosby; 1999.
17. Posnick JC. Craniofacial and Maxillofacial Surgery in Children and Young Adults. 1st ed. Philadelphia: W.B. Saunders; 2000.
18. Bays RA, Bouloux GF. Complications of orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2003;15:229-42.
19. Morris DE, Lo LJ, Margulis A. Pitfalls in Orthognathic Surgery: Avoidance and Management of Complications. Clin Plast Surg. 2007;34:e17-e29.
20. Roscoe MG, Meira JBC, Cattaneo PM. Association of orthodontic force system and root resorption: A systematic review. Am J Orthod Dentofacial Orthop. 2015;147:610-26.
21. Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138-46.
22. Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 1. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:62-6.
23. Sameshima GT, Asgarifar KO. Assessment of root resorption and root shape: periapical vs panoramic films. Angle Orthod. 2001;71:185-9.
24. Janson G, Valarelli FP, Henriques JFC, de Freitas MR, Cançado RH. Stability of anterior open bite nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2003;124:265-76.
Sara Palmares
E-mail address: sarapalmares.ortodontia@gmail.com
CRediT authorship contribution statement
Sara Palmares: Conceptualization, Data curation, Resources, Writing – original draft, Writing – review & editing. Rui Pereira: Conceptualization, Writing – original draft, Writing – review & editing, Validation, Supervision.
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed their work center protocols on access to patient data and for its publication.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
1646-2890/© 2023 Sociedade Portuguesa de Estomatologia e Medicina Dentária. Published by SPEMD.
This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
