
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD | 2019 | 60 (3) | 130-136
Original research
Effect of surface treatment and the use of mouthwashes on repaired composite bond strength
Efeito do condicionamento de superfície e do uso de elixires orais na resistência adesiva de compósito reparado
a Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b Oral and Biomedical Sciences Research Unit (UICOB), Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
Ana Filipa Chasqueira - filipach@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 3
Original research
Pages - 130-136
Go to Volume
Article History
Received on 29/07/2019
Accepted on 21/10/2019
Available Online on 04/11/2019
Keywords
Original research
Effect of surface treatment and the use of mouthwashes on repaired composite bond strength
Efeito do condicionamento de superfície e do uso de elixires orais na resistência adesiva de compósito reparado
Inês Pinheiroa, Gonçalo Barragana, Ana Filipa Chasqueirab,*, Sofia Arantes-Oliveirab, Jaime Portugalb
a Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
b Oral and Biomedical Sciences Research Unit (UICOB), Faculdade de Medicina Dentária, Universidade de Lisboa, Lisbon, Portugal
http://doi.org/10.24873/j.rpemd.2019.11.462
Abstract
Objectives: The purpose of this study was to evaluate the effect of mouthwashes on composite Knoop microhardness, and to assess the influence of the contact with mouthwashes and mechanical surface treatment on the shear bond strength of repaired composite resins.
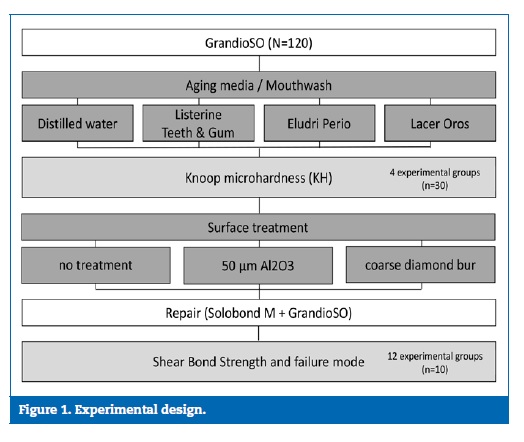
Methods: One hundred twenty composite resin (GrandioSO) specimens were prepared and randomly divided into four experimental groups, according to the used mouthwash (distilled water; Listerine Teeth & Gum; Eludril Perio; Lacer Oros). After a period of 5 days in water (37oC), during which the specimens were submitted to twelve cycles of 2 hours of immersion in the respective mouthwash, the Knoop microhardness was determined. Then, each group was divided into three subgroups based on the mechanical surface treatment performed (no treatment; 50-μm Al2O3 sandblasting; abrasion with diamond bur), the repair protocol was performed (Solobond M and GansdioSO) and specimens were submitted to shear bond strength tests until failure. Data were analyzed using ANOVA followed by Student-Newman- Keuls post-hoc tests (α=0.05).
Results: The group of specimens aged in distilled water presented a significantly harder surface than the other experimental groups (p<0.05). No statistically significant differences were found (p>0.05) between other groups. Neither the immersion media (p=0.214) nor the mechanical surface treatments (p=0.165) had a significant effect on the bond strength.
Conclusions: Although the hardness of the composite was negatively affected by contact with the mouthwashes used in this study, the bond strength of composite repair was not affected.
Keywords: Bond strength, Composite resin, Microhardness, Mouthwashes, Repair
Resumo
Objetivos: O objetivo deste estudo foi avaliar o efeito de elixires orais na microdureza Knoop na superfície de compósito, e avaliar a influencia do contato com elixires orais e condicionamento mecânico na resistência ao corte de resinas compostas reparadas.
Métodos:Cento e vinte espécimes de resina composta (GrandioSO) foram preparados e divididos aleatoriamente em 4 grupos experimentais, de acordo com o elixir utilizado (água destilada; Listerine Dentes & Gengivas; Eludril Perio; Lacer Ouros). Apos um periodo de 5 dias em água (37oC), durante os quais foram submetidos a 12 ciclos de 2 horas de imersão no respetivo elixir, foi determinada a microdureza Knoop. Em seguida, cada grupo foi dividido em 3 subgrupos com base no condicionamento mecânico da superfície do compósito (sem tratamento; jateamento com 50 μm Al2O3; abrasão com broca diamantada) e, apos o protocolo de reparação (Solobond M e GansdioSO), os espécimes foram submetidos a testes de resistência a tensões de corte. Os dados foram analisados usando ANOVA seguido por testes post-hoc segundo SKN (
Resultados: O grupo de espécimes envelhecidos em água destilada apresentou uma maior dureza que os demais grupos experimentais (p<0,05). Nao foram encontradas diferenças estatisticamente significativas (p>0,05) entre os demais grupos. Nem o contacto com elixir (p=0,214), nem o condicionamento mecânico de superfície (p=0,165) tiveram efeito significativo sobre a resistência adesiva.
Conclusões:Apesar da dureza do compósito ter sido afetada negativamente pelo contato com os elixires orais utilizados neste estudo, a resistência adesiva do composto reparado não foi afetada.
Palavras-chave: Resistencia adesiva, Resina composta, Microdureza, Elixires orais, Reparação
Introduction
The use of composite resins in restorative dentistry has significantly increased over the last years, due to the rising demand for esthetic dental restorations and the improvement of physical and chemical properties of these materials.1, 3
However, composite resins have a limited life-span due to clinical variables related to patients and materials, and also to the quality and technique of the operator.3, 6
The main reasons reported for restorations failure are secondary caries, fracture of the filling or the tooth itself, marginal deterioration, loss of anatomic form, wear, discoloration and pigmentation.6, 7 After the first 7 years in function, half of the composite resin restorations are estimated to require clinical intervention, and the clinician may choose to replace or repair them.2, 8
Replacement of defective restorations represents the major part of restorative dentistry in general dental practice and consists in the removal of the entire restoration followed by the placement of a new one.9 When a restoration is replaced, there is a loss of healthy dental tissue, increasing the size of the cavity to restore.8, 10 Furthermore, this technique is more time-consuming and costly, and more likely to cause damage to the pulp.7, 11,
Repair consists in the removal of part of the restoration together with the localized defect, followed by repairing only the prepared defect, allowing the preservation of part of the original restoration.9 This technique is more conservative, simple and time-saving.8, 11, 12 Several studies have demonstrated the good clinical performance of repaired restorations, including life spans similar to new restorations, thus making the repair a valid treatment option. Nevertheless, replacement of defective restorations still is the most common treatment in general dental practice.8, 13
In the repair approach, the material of the original restoration, which was exposed to the oral environment, may have undergone several changes in its surface and structure that may influence the success of a subsequent repair.14, 17 Mouthwashes, which often have a high alcohol content and a low pH, can contribute to this degradation process and consequently to the reduction of the mechanical properties of the repaired composite restoration.18, 19
Knowing that the bond strength between an old composite and a new composite is frequently lower than the cohesive strength of the material, the prior mechanical and/or chemical conditioning of the surface of the aged composite has been proposed to increase the bond strength between the two increments.15, 20 - 23 Nevertheless, the relationship between the repair bond strength and the surface changes resulting from aging and/or applied treatments remains unclear, and there is no consensus on the results obtained with different procedures.
Therefore, the present study aimed to investigate composite microhardness and composite repair bond strength after immersion in mouthwashes, according the following hypotheses: 1) mouthwashes do not affect the composite microhardness; 2) exposing the composite resin to mouthwashes does not influence its repair bond shear; and 3) mechanical surface treatment of aged composite does not influence shear bond strength between the two increments of the repaired composite restoration.
Material and methods
The sample size (n=10) was estimated, based on a pilot study, with a power analysis in order to provide a statistical significance (α=0.05) at 80% power.24, 25
One hundred twenty specimens were fabricated using a silicon mold with 2 mm of depth and 6 mm of diameter. The mold was placed on a glass slide, with an acetate strip placed between them, and a single increment of a nanohybrid composite was applied (GrandioSO, shade A3, VOCO). A new acetate strip was placed, and slight pressure with another glass slide was applied to ensure that the surfaces of the specimens remained flat. After removing the glass slide, the specimens were light-polymerized through the upper acetate strip (Ortholux Curing Light LED, 3M Unitek; 900 mW/cm2) for 10 seconds.
The surface nearest the light source was identified as the top of the specimen. The sample was randomly divided into four groups (n=30), according to the aging media: distilled water (control group); Listerine Teeth & Gum (Johnson & Johnson); Eludril Perio (Pierre Fabre); and Lacer Oros (Lacer). After an initial storage period of 24 hours with all specimens immersed in distilled water (37oC), the specimens were submitted to twelve cycles of 2 hours of immersion in the respective aging media. The aging media was renewed for each cycle, and the specimens were stored in distilled water between cycles (37oC).
The Knoop hardness (KH) of the top of the specimens was determined using a microhardness tester (Duramin Struers) with a load of 245 mN applied for 10 seconds. Three indentations were made on each specimen: one in the center and the other two on each side of the first indentation at a distance of 1.5 mm. The mean of the three measurements was used as the hardness value for each specimen.
Then, each group was randomly divided into three subgroups based on the mechanical surface treatment performed.
One-third of the specimens were sandblasted with 50-μm aluminum oxide (Al2O3) particles (Microetcher II, Danville Engineering) perpendicular to the top composite surface (0.25 MPa pressure, 5 seconds, 5-mm distance). Another third of the specimens were abraded with a coarse diamond bur (DZ Diamant, 806.314) by making two passes perpendicular between them, with the axis of the bur parallel to the top surface of the composite.
The remain specimens received no surface treatment and were used as control. Consequently, twelve experimental groups were set, according to the several possible combinations between mouthwash and surface treatment (Figure 1).
After the specimens were washed in current water and dried, an adhesion area of 3 mm in diameter was defined in the top surface of each specimen, with a perforated adhesive tape. The adhesive system (Solobond M, VOCO) was applied to the adhesion area, left undisturbed for 30 seconds, dried with a gentle airstream for 5 seconds, and light-polymerized for 20 seconds. Two 2-mm increments of composite (GrandioSO, shade A3) were then applied and light-polymerized for 10 seconds each. After a storage period of 24 hours in water (37oC), the repaired specimens were submitted to shear bond strength (SBS) tests, performed with a single-plane lap device in a universal testing machine (Instron Model 4502, Instron Ltd.), with a 1 kN load cell and at a crosshead speed of 1 mm/min, until fracture.25
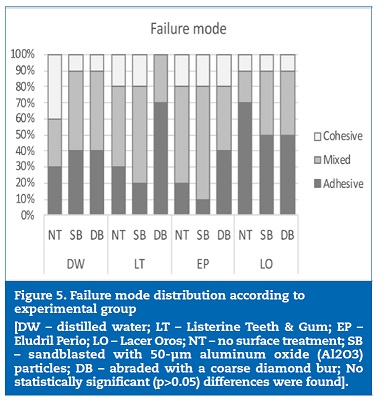
The mode of failure was evaluated using a stereomicroscope (EMZ-8TR, Meiji Techno Co.) at 20x magnification. It was classified as adhesive if the failure occurred at the adhesive interface between the aged and the repair composite resins, as cohesive if it occurred in the composite resin, and as mixed when a combination of the two previous types was observed.
Data were analyzed using the IBM SPSS Statistics for Macintosh, version 25.0 (IBM Corp.). The microhardness data were submitted to one-way ANOVA, followed by Student-Newman-Keuls multiple comparison post-hoc tests. SBS data were analyzed with a two-way ANOVA and the mode of failure with chi-square tests. Statistical significance was defined at the level of 5% (α=0.05).
Results
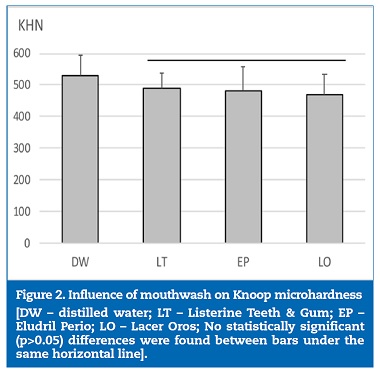
Microhardness mean values ranged between 469.4 KHN, in the specimens aged in Lacer Oros, and 530.3 KHN, in the specimens that were not exposed to mouthwashes (Table 1). Microhardness was significantly (p=0.002) influenced by the aging media (Figure 2). Specimens aged in distilled water presented a significantly (p<0.05) harder surface then specimens aged in all the other aging media. No statistically significant (p>0.05) differences were found between mouthwashes.
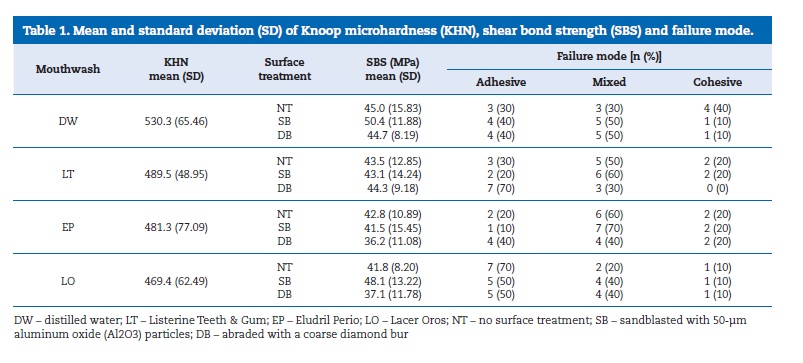
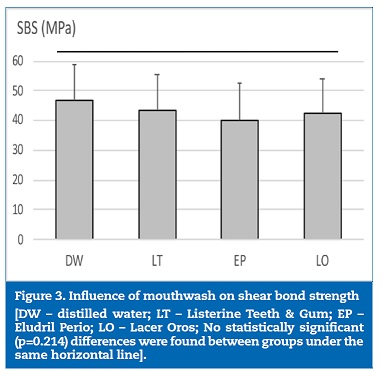
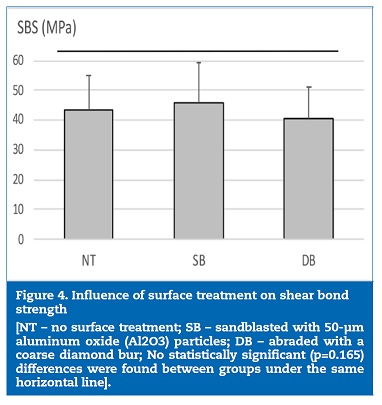
Descriptive statistics of SBS and failure mode are illustrated in Table 1. SBS was not significantly influenced either by mouthwashes (p=0.214; Figure 3) or the mechanical surface treatment (p=0.165; Figure 4), and no significant (p=0.740) interaction was found between factors. Failure mode was predominantly mixed and adhesive. Chi-square tests did not detect statistically significant differences (p>0.05) on failure mode (Figure 5).
Discussion
One of the purposes of this study was to analyze the effect of mouthwashes on the microhardness of composite resins, not only because they are widely used by population, but also because several studies indicate that the properties of these materials are significantly affected by immersion in acidic and alcoholic solutions.18 26 - 30 Therefore, artificial aging of the specimens was performed with immersion cycles in mouthwashes in order to simulate 1 year of daily mouthwash. To minimize the oxygen inhibition layer, which may influence the results, the composites were cured against an acetate strip.
In the present study, exposing the composite resin to each of the three mouthwashes tested resulted in lower microhard-ness than when this restorative material was exposed to water, which is in agreement with the results obtained in previous studies.30, 33 Mouthwashes are capable of diffusing through the polymeric matrix, expanding the polymer chains and causing chemical softening with loss of constituents, thus leading to the deterioration of the properties of the composite resin.14, 15
Alcohol is a good methacrylate solvent, and may swell the polymeric matrix of the resin composites, increasing the amount of unreacted monomers and oligomers that diffuse out of materials.18 However, specimens exposed to mouthwash with alcohol (Listerine Teeth & Gum) had similar hardness to those immersed in the mouthwash with no alcohol (Eludril Perio and Lacer Oros).
The pH of the tested solutions provides another potential preponderant factor for the composite matrix degradation.(30) According to the manufacturers’ information, each of the tested mouthwashes has other components (such as benzoic and citric acid) that may also have a deleterious effect on the composite resin, and this needs to be taken into consideration.
Compared to distilled water (pH=5.5), the higher acidity of the mouthwashes may have altered the polymeric matrix of the resin composites by catalysis of ester groups from dimethacrylate monomers present in their compositions. The hydrolysis of these ester groups may have formed molecules capable of accelerating the degradation of the composite resin.30 On the other hand, the low pH may have also caused the erosion in the surface of the filler particles, accelerating their debonding.16
Bonding between an aged composite resin and added fresh composite resin can be affected by several factors, such as surface roughness, adhesive system, repairing material and aging period.34 When performing a conventional composite restoration using the incremental technique, the presence of an oxygen-inhibited unpolymerized layer ensures the bonding between two composite increments.23 However, bonding new composite material to an aged composite restoration presents a different and harder challenge, as there are few or no unreacted methacrylate groups remaining.35 In order to overcome this limitation, several techniques have been recommended to improve the composite-composite bond strength, such as chemical and mechanical conditioning of the aged restoration surface.36, 37 Mechanical surface treatment aims to remove the superficial layer, increase the surface energy and area, roughen it, and promote mechanical interlocking.38 However, roughening the composite surface may decrease the bond strength as a consequence of filler exposure.35 As observed in previous studies, 35, 39 in the present study, the surface treatment did not influence the bond strength. The use of a chemically compatible adhesive system is an important factor in adhesion.21, 34
However, creating a synergistic effect between mechanical treatment and adhesive system might be the main rule for achieving effective and durable adhesion between the two composite increments of a repaired composite restoration.35, 36
Since the use of bonding agents may mask the effect of mechanical treatments, these effects could have been better evaluated if a negative control group (without bonding agent) had been added to the study.35
In the present study, no differences were found in failure mode, which is consistent with bond strength results.
Conclusions
Exposure to mouthwashes decreased the microhardness of the composite resin but did not affect the composite repair bond strength. The shear bond strength and failure mode were not influenced by surface treatment.
References
1. Bayne SC, Ferracane JL, Marshall GW, Marshall SJ, van Noort R. The evolution of dental materials over the past century: silver and gold to tooth color and beyond. J Dent Res. 2019;98:257-65.
2. Sharif MO, Catleugh M, Merry A, Tickle M, Dunne SM, Brunton P, et al. Replacement versus repair of defective restorations in adults: resin composite. Cochrane Database Syst Rev. 2014:CD005971.
3. Ferracane JL. Resin composite – State of the art. Dent Mater. 2011;27:29-38.
4. Dahl JE, Stenhage ISR. Optimizing quality and safety of dental materials. Eur J Oral Sci. 2018;126(S1):102-5.
5. Ozcan M, Barbosa SH, Melo RM, Galhano GA, Bottino MA. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent Mater. 2007;23:1276-82.
6. Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitao J, DeRouen TA. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138:775-83.
7. Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87-101.
8. Moncada G, Martin J, Fernandez E, Hempel MC, Mjor IA, Gordan VV. Sealing, refurbishment and repair of Class I and Class II defective restorations: a three-year clinical trial. J Am Dent Assoc. 2009;140:425-32.
9. Blum IR, Lynch CD, Wilson NH. Teaching of direct composite restoration repair in undergraduate dental schools in the United Kingdom and Ireland. Eur J Dent Educ. 2012;16:e53-8.
10. Lynch CD, Blum IR, Frazier KB, Haisch LD, Wilson NH. Repair or replacement of defective direct resin-based composite restorations: Contemporary teaching in U.S. and Canadian dental schools. J Am Dent Assoc. 2012;143:157-63.
11. Brunton PA, Ghazali A, Tarif ZH, Loch C, Lynch C, Wilson N, et al. Repair vs replacement of direct composite restorations: a survez of teaching and operative techniques in Oceania. J Dent. 2017;59:62-7.
12. Rinastiti M, Ozcan M, Siswomihardjo W, Busscher HJ. Immediate repair bond strengths of microhybrid, nanohybrid and nanofilled composites after different surface treatments. J Dent. 2010;38:29-38.
13. Fernandez EM, Martin JA, Angel PA, Mjor IA, Gordan VV, Moncada GA. Survival rate of sealed, refurbished and repaired defective restorations: 4-year follow-up. Braz Dent J. 2011;22:134-9.
14. Bagheri R, Tyas MJ, Burrow MF. Subsurface degradation of resin-based composites. Dent Mater. 2007;23:944-51.
15. Fawzy AS, El-Askary FS, Amer MA. Effect of surface treatments on the tensile bond strength of repaired wateraged anterior restorative micro-fine hybrid resin composite. J Dent. 2008;36:969-76.
16. Ferracane JL. Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 2006;22:211-22.
17. Jaffer F, Finer Y, Santerre JP. Interactions between resin monomers and commercial composite resins whit human saliva derived esterase. Biomaterials. 2002;23:1707-19.
18. Almeida GS, Poskus LT, Guimaraes JG, da Silva EM. The effect of mouthrinses on salivary sorption, solubility and surface degradation of a nanofilled and a hybrid resin composite. Oper Dent. 2010;35:105-11.
19. Ferracane JL, Marker VA. Solvent degradation and reduced fracture toughness in aged composites. J Dent Res. 1992;71:13-9.
20. Rodrigues SA Jr, Ferracane JL, Della Bona A. Influence of surface treatments on the bond strength of repaired resin composite restorative materials. Dent Mater. 2009;25:442-51.
21. Padipatvuthikul P, Mair LH. Bonding of composite to water aged composite with surface treatments. Dent Mater. 2007;23:519-25.
22. Loomans BA, Cardoso MV, Roeters FJ, Opdam NJ, De Munck J, Huysmans MC, et al. Is there one optimal repair technique for all composites? Dent Mater. 2011;27:701-9.
23. Oliveira SA, Bernardo M, Portugal J, Leitao J. Reparação imediata de restaurações directas em resina composta utilizando sistemas adesivos self-etching. Rev Port Estomatol Cir Maxilofac 2005;46:197-202.
24. Rosca B, Ramalho S, Sampaio-Fernandes JC, Portugal J. Reparability of two different CAD/CAM polymer materials using light-cured composite and universal adhesive. Rev Port Estomatol Cir Maxilofac. 2016;57:189-96.
25. Mendes M, Portugal J, Arantes-Oliveira S, Mesquita P. Shear bond strength of orthodontic brackets to fluorosed enamel. Rev Port Estomatol Med Dent Cir Maxilofac. 2014;55:73-7.
26. Silva PF, Barragan G, Chasqueira F, Oliveira SA, Portugal J. Efeito do envelhecimento em ácido cítrico na microdureza e resistencia a flexão de resinas compostas. Rev Port Estomatol Med Dent Cir Maxilofac. 2012;53:227-32.
27. Valinoti AC, Neves BG, da Silva EM, Maia LC. Surface degradation of composite resins by acidic medicines and pH-cycling. J Appl Oral Sci. 2008;16:257-65.
28. Yap AU, Tan SH, Wee SS, Lee CW, Lim EL, Zeng KY. Chemical degradation of composite restoratives. J Oral Rehabil. 2001;28:1015-21.
29. Franscisconi LF, Honorio HM, Rios D, Magalhaes AC, Machado MAAM, Buzalaf MAR. Effect of erosive pH cycling on different restorative materials and on enamel restored With these materials. Oper Dent. 2008;33:203-8.
30. Miranda DA, Bertoldo CE, Aguiar FH, Lima DA, Lovadino JR. Effects of mouthwashes on Knoop hardness and surface roughness of dental composites after different immersion times. Braz Oral Res. 2011;25:168-73.
31. Al-Samadani KH. Surface hardness of dental composite resin restorations in response to preventive agents. J Contemp Dent Pract. 2016;17:978-84.
32. Penugonda B, Settembrini L, Scherer W, Hittelman E, Strassler H. Alcohol-containing mouthwashes: effect on composite hardness. J Clin Dent. 1994;5:60-2.
33. Weiner R, Millstein P, Hoang E, Marshall D. The effect of alcoholic and nonalcoholic mouthwashes on heat-treated composite resin. Oper Dent. 1997;22:249-53.
34. Zhang Y, Xu J. Effect of immersion in various media on the sorption, solubility, elution of unreacted monomers, and flexural properties of two model dental composite compositions. J Mater Sci Mater Med. 2008;19:2477-83.
35. Yesilyurt C, Kusgoz A, Bayram M, Ulker M. Initial repair bond strength of a nano-filled hybrid resin: effect of surface treatments and bonding agents. J Esthet Restor Dent. 2009;21:251-60.
36. Brosh T, Pilo R, Bichacho N, Blutstein R. Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 1997;77:122-6.
37. Rathke A, Tymina Y, Haller B. Effect of different surface treatments on the composite-composite repair bond strength. Clin Oral Invest. 2009;13:317-23.
38. Soderholm K-JM, Roberts MJ. Variables influencing the repair strength of dental composites. Scand J Dent Res. 1991;99:173-80.
39. Melo MA, Moyses MR, Santos SG, Alcantara CE, Ribeiro JC. Effects of different surface treatments and accelerated artificial aging on the bond strength of composite resin repairs. Braz Oral Res. 2011;25:485-91.
Ana Filipa Chasqueira
E-mail address: filipach@gmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflict of interest
The authors have no conflicts of interest to declare.
Article history:
Received 22 July 2019
Accepted 21 October 2019
Available online 4 November 2019
