
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2019 | 60 (2) | 85-89
Case report
Mandibular traumatic bone cyst: case report
Cisto ósseo traumático mandibular: relato de caso
a Metropolitan Union for Education and Culture – UNIME. Lauro de Freitas, Bahia
b CTBMF Service at Clériston Andrade Hospital – SESAB
c State University of Feira de Santana – UEFS
Sheinaz Farias Hassam - sheinazhassam@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 60
Issue - 2
Case report
Pages - 85-89
Go to Volume
Article History
Received on 10/03/2019
Accepted on 07/08/2019
Available Online on 04/09/2019
Keywords
Case report
Mandibular traumatic bone cyst: case report
Cisto osseo traumatico mandibular: relato de caso
Fabiana Sadya, Sheinaz Farias Hassama,*, Antonio Varela Canciob, Juliana Andrade Cardosoa, Jener Gonçalves de Fariasa,c
a Metropolitan Union for Education and Culture – UNIME. Lauro de Freitas, Bahia.
b CTBMF Service at Clériston Andrade Hospital – SESAB.
c State University of Feira de Santana – UEFS.
http://doi.org/10.24873/j.rpemd.2019.09.450
Abstract
The traumatic bone cyst belongs to a group of lesions of maxillomandibular bones and is considered as a pseudocyst by the World Health Organization. It is usually diagnosed through a routine radiographic examination. Lucas defined it in 1929 with unclear pathogenesis; meanwhile, the trauma-hemorrhage theory has been the most defended by pathologists. Due to not having a definite cause, this lesion has several names: “simple bone cyst,” “solitary bone cyst,” “hemorrhagic bone cyst” or “unicameral bone cyst.” The aim of this study is to report a clinical case of a traumatic bone cyst in the jaw region in a female patient, describing its pathogenesis and radiographic, clinical and histopathological aspects. Diagnosis was confirmed by surgical exploration, which is considered as the only method for a more precise diagnosis. The patient was treated by curettage of the bone cavity and has been observed annually, not showing any clinical or radiographic signs of recurrence.
Keywords: Bone cysts,Oral surgery,Therapeutics
Resumo
O cisto ósseo traumático pertence ao grupo das lesões ósseas dos ossos maxilares, considerado um pseudocisto pela Organização Mundial de Saúde (OMS), geralmente diagnosticado em exames radiográficos de rotina. Definido por Lucas em 1929, sua etiopatogenia até então não foi esclarecida, contudo, a teoria trauma-hemorragia é a mais defendida pelos patologistas. Devido à ausência de uma causa definida, ela pode ser denominada de cisto ósseo simples, cisto ósseo solitário, cisto ósseo hemorrágico e cisto ósseo unicameral. O presente trabalho tem como objetivo apresentar um caso clínico de cisto ósseo traumático em região de mandíbula, acometendo paciente do sexo feminino, abordando etiopatogenia, aspectos radiográficos, clínicos e histopatológicos. O diagnóstico foi confirmado através da exploração cirúrgica. único método de confirmação para um melhor diagnóstico até o momento. O tratamento foi realizado com curetagem da loja óssea e a paciente vem sendo observada anualmente sem sinais clínicos e imaginológicos de recidiva.
Palavras-chave: Cistos ósseos,Cirurgia bucal, Tratamento
Introduction
The lesions associated with maxillomandibular bones are part of a group of bone pathologies that includes one hundred rare diseases caused by the histologic, anatomical and functional complexity of the bone tissue. The classification of these pathologies includes a diverse range of lesions such as neoplasms, cement‑bone dysplasia, fibro‑osseous lesions and pseudocysts. The group of pseudocysts in particular, which differ from true cysts due to the absence of an internal epithelium, includes, among others, the aneurysmal bone cyst and the traumatic bone cyst.1
The traumatic bone cyst (TBC) is an uncommon intra‑osseous lesion that is considered by the World Health Organization (WHO) as a non‑neoplastic pseudocyst, in which the cavity can be found empty or filled with cystic liquid.2, 3 The first case was reported in 1832 in large bones,3 and, in 1929, Lucas defined these lesions in the maxillary region.2, 3 Several synonyms are found in the literature to nominate this pathology, such as “simple bone cyst,” “solitary bone cyst,” “hemorrhagic bone cyst” and “idiopathic cavity.”1, 4
The traumatic bone cyst is rare, corresponding to 1‑2% of maxillary cysts, and its diagnosis is usually based on a routine panoramic radiograph or orthodontic records.5 It frequently occurs in young male adults in the second decade of life and shows no predilection for ethnic groups.6, 7
Clinically, the lesion is asymptomatic. The absence of boné growth can be observed in approximately 92% of the patients, showing the potential of the lesion to develop in narrow spaces.
Its location in the maxillomandibular complex is almost exclusively in the mandible, which suggests a possible connection with the pathogenesis of the lesion, since the cortical bone in that region cannot be associated with the trauma‑hemorrhage theory because of the lower repair capacity of the mandible when compared to the maxilla.8
The vitality of the teeth involved is not affected, and their roots do not show absorption. The radiographic image shows a well‑defined radiolucent lesion that can be unilocular or multilocular, and the differential diagnosis is made with dentigerous cysts and odontogenic tumors such as the keratocyst and the ameloblastoma.2, 8 ‑10
The diagnosis of traumatic bone cyst is obtained by exploring the lesion surgically because the material collected for histological analysis in most cases is scarce due to the absence of the epithelial membrane. In the surgical exploration, the dentist usually comes across an empty cavity, although blood, serum or both may be present.10
The aim of this article is to report a rare case of traumatic bone cyst in a young female patient, emphasizing the methods of diagnosis and surgical treatment and comparing it with the current literature.
Case report
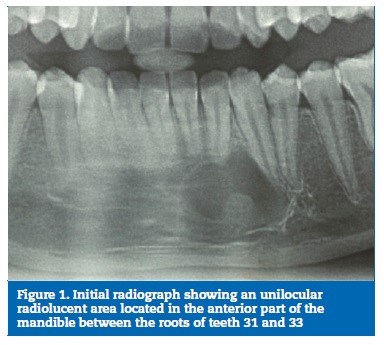
A 16‑year‑old white female patient was referred to the Post‑Graduation in Oral Surgery at UNIME (Lauro de Freitas – BA) by her orthodontist. In her orthodontic records, a radiographic image showed a well‑defined radiolucent, unilocular area that extended across the anterior part of the mandible to the roots of teeth 3.1 to 3.3 (Figure 1). During the anamnesis, no systemic disorders were found, and the patient did not report any injury in the region.
In the intraoral examination, a bulged area without symptoms was observed. The hypothetical diagnosis of a traumatic bone cyst was established, based on the clinical and radiographic records. Thus, surgical exploration with direct visualization of the lesion was proposed to help the diagnosis, with the possibility of an incisional biopsy if a capsule was observed during surgery.
Under local anesthesia, a straight incision was made further down the attached gingiva to obtain a full gingival flap. It was displaced, giving access to the cortical part, which appeared slightly bulged. Before reaching the lesion, a small bone cavity was made with a surgical drill, under saline irrigation, to puncture the lesion and determine its internal contents, thereby discarding vascular lesions, such as hemangioma and aneurysmal cyst, as the origin (Figures 2‑3).
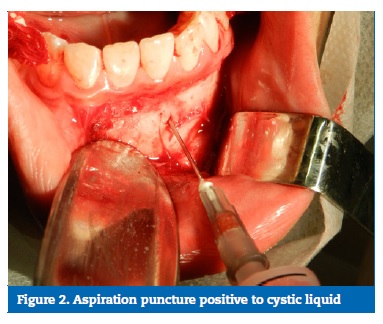
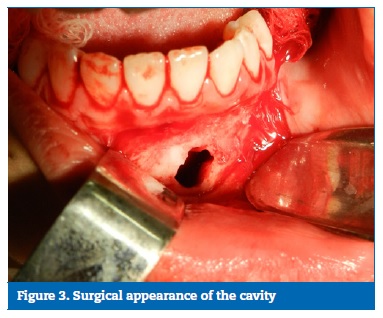
The puncture was positive for cystic fluid and, thus, an osteotomy was performed, expanding the access to the lesion.
Since the lesion had no capsule, and surgically it was only an empty cavity, the surgical diagnosis was conclusive for traumatic bone cyst. The vestibular access was extended, and the interior of the surgical cavity was curetted in all its walls to induce bleeding and enable bone formation. Then, the soft tissues were sutured with a 4‑0 silk thread (SHALON®) (Figures 4‑5).


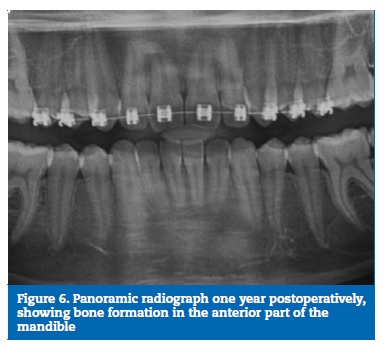
Six months after the surgery, the panoramic radiography for postoperative control showed new bone formation at the site in response to the induced bleeding during the surgery.
The patient has been followed annually, and the radiographic images show a successful treatment with bone formation in the anterior part of the mandible (Figure 6).
Discussion and conclusions
A large number of cases of intra‑osseous lesions without symptomatology can be diagnosed based on the results of panoramic radiography,6 particularly those that are requested for orthodontic treatment. In this case, the patient’s lesion in the mandible was detected in a panoramic radiograph that had been requested for planning orthodontic therapy.
The literature reports the highest incidence of TBC in the first and third decades of life and, although gender preference is still unclear, approximately 3 out of 5 cases occur in men.6
In this case, the patient was 16 years old, which is in agreement with the age groups most affected by TBC. The cause of these lesions is still controversial, yet the trauma‑hemorrhage theory has many supporters.6 In the present case, the patient did not report any history of trauma to the face.
Most authors consider the mandible bone as the most common anatomical location for the TBC.2 The patient in this report had a lesion in the anterior part of the mandible, thus confirming what has been observed in the literature.
Regarding clinical findings, the lesion usually presents itself without symptoms, and a few patients demonstrate an increased volume of the affected area. The teeth involved are vital and show no evidence of root resorption.2,6 In the presented case, the patient had an increased vestibular cortical bone without painful symptoms. The pulpal sensitivity tests in nearby teeth associated with the lesion were positive, suggesting pulpal vitality.
The image analysis of lesions suspected to be traumatic bone cysts enables the estimation of the extension and limits of the lesion and adjacent structures.6 Radiographically, the cyst appears as a radiolucent area, usually unilocular, variable in size and with well‑defined limits. In this case, and agreeing with published findings, the radiographic image shows the lesion as a radiolucent unilocular, well‑defined image.
Surgical exploration is the most recommended curative therapy, as well as the best way to close the diagnosis of traumatic bone cyst.6, 9, 10 After that procedure, the new bone formation is considerably fast.1 In the present case, curettage of the walls of the surgical cavity was performed to stimulate new bone formation. There was no need to collect tissue samples for histopathological analysis due to the absence of an epithelial membrane.
The traumatic bone cyst is clinically characterized as an asymptomatic benign lesion, but it requires an immediate diagnosis to differentiate it from other aggressive lesions such as the ameloblastoma and the odontogenic keratocyst. A thorough anamnesis, a well‑done physical examination and a complete radiographic analysis are required to obtain the final diagnosis.
The treatment consists of lesion removal and curettage of the bone cavity walls. In addition, clinical and radiographic monitoring is needed to certify the complete healing of the cyst. The case reported was successfully treated and an annual monitoring period of 3 years was established. During this time, no clinical and radiographic signs of lesion recurrence occurred.
References
1. Sudha SG, Thomas S, Nair VV. Simple bone cyst presenting as an incidental finding in pretreatment orthodontic radiograph: A case report. J Indian Acad Oral Med Radiol. 2017;29:53‑5.
2. Kumar LKS, Kurien N, Thaha KA. Traumatic Bone Cyst of Mandible. J Maxillofac Oral Surg. 2015;14:466‑69.
3. Oliveira AN, Santos JM, Assis A, Reis SRA, Medrado AP. Cisto ósseo simples: Relato de caso clínico. Journal of Dentistry and Public Health. 2014;5:167‑73.
4. Paiva LCA, Menezes FS, Porto GG, Cerqueira PRF. Cisto Ósseo Simples – Relato de Caso. Rev Cir Traumatol Buco‑Maxilo‑Fac. 2011;11:15‑20.
5. Ramos Júnior JM, Carneiro LS, Ferraz TM, Cunha CR. Cisto ósseo simples em mandíbula com abordagem conservadora. Revista Ciências e Odontologia RCO. 2018;2:39‑
6. Flores IL, Hamilton ME, Baldissera EFZ, Vasconselos ACU, Tarquínio SBC, Gomes APN. Simple and aneurysmal bone cyst: Aspects of jaw pseudocysts based on an experience of Brazilian pathology service during 53 years. Med Oral Patol Oral Cir Bucal. 2017;22:64‑9.
7. Velho FMT. Cisto Ósseo Traumático na Região da Sínfise Mandibular: Relato de caso. Monografia [Especialização em Radiologia e Imaginologia]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2015.
8. Martins‑Filho PRS, Santos TS, Araújo VLC, Santos JS, Andrade ESS, Silva LCF. Traumatic bone cyst the mandible: a review of 26 cases. Braz J Otorhinolaryngol. 2012;78:16‑21.
9. Dominguette AAS, Felizardo HMA, Dominguette MHL, Matos BHF, Oliveira LR, Dominguette PR. Cisto Ósseo em Mandíbula: relato de caso. Revista da Universidade Vale do Rio Verde. 2012;10:308‑13.
10. Toledo GL, Marzola, C, Toledo Filho JL, Capelari MM, Moura LA. Cisto ósseo traumático: Caso clínico. Rev Port Estomatol Med Dent Cir Maxilofac. 2009;50:237‑41.
Sheinaz Farias Hassam
E-mail address: sheinazhassam@hotmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interest
The authors have no conflicts of interest to declare.
Article history:
Received 10 March 2019
Accepted 7 August 2019
Available online 4 September 2019
