
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (3) | 169-173
Case report
Lingual frenotomy of a patient with Juvenile Idiopathic Arthritis and Attention Deficit Hyperactivity Disorder
Frenectomia lingual num paciente com Artrite Idiopática Juvenil e Transtorno de Déficit de Atenção e Hiperatividade
a Department of Dentistry, Unicsul, São Paulo, Brazil
b School of Dentistry, University of São Paulo, São Paulo, Brazil
c Department of Dentistry, Persons with Disabilities Division, Unicsul, São Paulo, Brazil
d Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of São Paulo, São Paulo, Brazil
Gabriela M. Gutierrez - gabrielamancia@hotmail.comgabrielamancia@hotmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 3
Case report
Pages - 169-173
Go to Volume
Article History
Received on 14/05/2018
Accepted on 20/11/2018
Available Online on 20/11/2018
Keywords
Case report
Lingual frenotomy of a patient with Juvenile Idiopathic Arthritis and Attention Deficit Hyperactivity Disorder
Frenectomia lingual num paciente com Artrite Idiopática Juvenil e Transtorno de Déficit de Atenção e Hiperatividade
Gabriela M. Gutierreza,b,*, Fernanda S. Delmondesb, Carlos F. Bonacinaa,b, Maria Teresa B.R. Santosc, Mariana Bragab,d, Adriana L. Ortegab,c
a Department of Dentistry, Unicsul, São Paulo, Brazil.
b School of Dentistry, University of São Paulo, São Paulo, Brazil.
c Department of Dentistry, Persons with Disabilities Division, Unicsul, São Paulo, Brazil.
d Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of São Paulo, São Paulo, Brazil.
http://doi.org/10.24873/j.rpemd.2018.11.235
Abstract
The aim of this paper is to describe the management of a clinical case of a teenager with Juvenile Idiopathic Arthritis (JIA), Attention Deficit Hyperactivity Disorder (ADHD) and ankyloglossia. A 12-year-old female using methotrexate and etanercept for the treatment of JIA, without the use of ADHD medication, presented tongue-tie and limited mouth opening. Frenectomy under local anesthesia was performed; antibiotic coverage was provided 24 hours before the procedure and maintained for one week after. After the surgical procedure, the patient was referred to a speech therapist to improve chewing and swallowing functions. It was concluded that the knowledge of dentist about the oral manifestations of JIA, knowing the risk of infection of these patients when submitted to surgical procedures and, in cases of ankyloglossia, to observe the need for the patient to perform speech therapy after surgical intervention.
Keywords: Ankyloglossia Attention Deficit Hyperactivity Disorder Juvenile Idiopathic Arthritis
Resumo
O objetivo deste estudo é descrever um caso clínico de uma adolescente com Artrite Idiopática Juvenil (AIJ) e Transtorno de Déficit de Atenção e Hiperatividade (TDAH) com quadro de anquiloglossia. Paciente do género feminino, 12 anos de idade, fazendo uso de Metotrexato e Etanercepte para o tratamento da AIJ, sem uso de medicação para o TDAH, apresentava anquiloglossia e limitação de abertura bucal. Foi realizada frenectomia lingual, sob anestesia local com cobertura antibiótica iniciada 24h antes e mantida por uma semana. Após procedimento cirúrgico a paciente fez terapia fonoaudiológica para melhorar as funções de mastigação e deglutição. Concluiu-se que é importante o conhecimento do médico dentista sobre as características clínicas da AIJ, uma vez que há risco de infeção quando esses pacientes são submetidos a procedimentos cirúrgicos e sobre a necessidade, nos casos de anquiloglossia, de se realizar fonoterapia após a correção cirúrgica.
Palavras-chave: Freio lingual Artrite Idiopática Juvenil Transtorno do Deficit de Atenção e Hiperatividade
Introduction
Juvenile Idiopathic Arthritis (JIA) is the most common, chronic, rheumatic childhood disease and is characterized by onset before 16 years of age and unknown etiology. The prevalence varies between 16 to 150 per 100,000; females are much more frequently affected. 1 When undiagnosed, JIA has the potential to cause permanent sequelae and impair the growth of affected.2 The clinical manifestations of JIA heterogeneous. Large joints are the most commonly affected, but the temporomandibular joint (TMJ) can be affected,2 the symptoms are: pain, articular noise, difficulty in chewing, limited opening and facial growth disturbances.3 Condylar alterations are frequent, and patients may be asymptomatic even in the presence of severe TMJ changes. 4, 5
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder beginning in childhood and is defined by harmful levels of inattention, motor hyperactivity and impulsivity. 6The estimated prevalence in children is 3.4% (95% CI 2.6 - 4.5) according to the most recent meta-analysis7 and is more common in males. 6, 8 This disorder it is characterized as a multifactorial.6, Treatment enables the child to behave satisfactorily through psychotherapy and medication use in some cases.9 Studies have shown that children with ADHD have a higher risk of developing caries10 and have a higher plaque index.11 Their behavior and its influence on oral health suggest the need for the development and implementation of specific strategies for the prevention and treatment of oral diseases.12
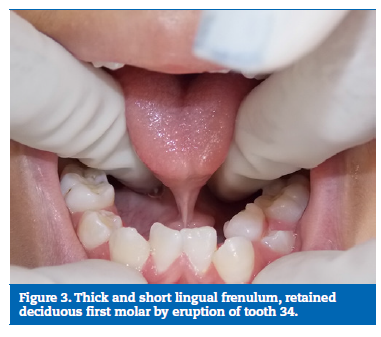
Ankyloglossia is a congenital anomaly in tongue development in which the lingual frenulum is shorter, resulting in the limitation of its movement.13 The prevalence varies greatly from 0.1% to 10.7%.14 The different diagnostic criteria used in the studies could explain the variation in prevalence.13 The frenectomy is the treatment of this condition and when performed brings anatomical and mobility gains to the tongue.15 However, functional changes may remain after the intervention requiring speech therapy in some cases.4
In the literature, there is no correlation between JIA and ADHD and ankyloglossia. In other words, the two conditions are not directly related to the etiopathogenesis of ankyloglossia, which may be a nonspecific morphological alteration. The purpose of this paper was to describe the surgical management of an adolescent with JIA, ADHD and ankyloglossia.
Case report
A 12-year-old female patient was referred to the Pediatric Dentistry Specialization Course of the University of São Paulo (USP), Brazil with the main complaint of ankyloglossia. During the first consultation, there was below-average intellectual development as well as childish and anxious behavior. The patient did not use medication for ADHD, but used medications for JIA including Methotrexate, Folic acid, Omeprazole, Vitamin D3 and Etanercept.
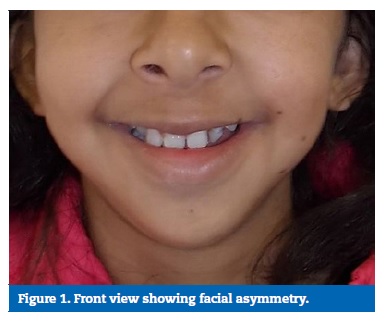
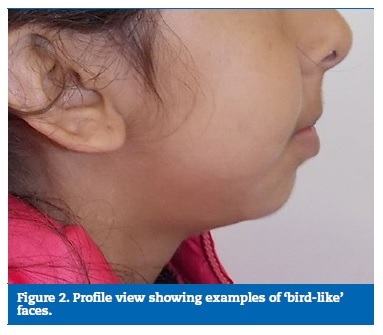
The extraoral examination findings reported the phenotypic face of JIA: a ‘bird-face’3 appearance, retrognathia and facial asymmetry (Figures 1 and 2). Intraoral examination revealed ankyloglossia, as well as prolonged retention of tooth 74 and the presence of tooth 34 (Figure 3). Plaque accumulation was observed in the cervical margins of the teeth, especially in the anterior region associated with gingival inflammation. The maximum voluntary opening of the mouth was limited, measuring 28.0 mm, without articular sound, and the patient did not report orofacial pain or discomfort, including in the TMJ region. The panoramic radiograph (Figure 4) showed agenesis of the teeth 22, 32 and 42; and that the bilateral condylar head was flattened.

The treatment plan consisted of providing oral health education to the patient and her mother, followed by a lingual frenectomy and extraction of tooth 74. The two surgical procedures were performed in one session. Since patients with JIA are at an increased risk for infection,16 and to avoid secondary infection associated with immunosuppression, antibiotic therapy was prescribed. The protocol established was 375 mg of amoxicillin given 24 hours before the procedure and continued for seven days, every 8 hours, and it was established in agreement with the patient’s rheumatologist.
Due to the patient’s mouth opening limitation and poor cooperation, a mouth opener made of wooden spatulas was used during all stages of the surgical procedures. The frenectomy was performed following conventional surgery. Under local anesthesia, the tongue was raised toward the palate with a grooved director (Figure 5) and an incision was made with a scissors (Figure 6) leaving a diamond-shaped wound.


The wound margins were undermined with the tips of blunt-ended dissecting scissors. The modification of the conventional technique in this case was the choice of the 3-0 absorbable suture. The fact that it was absorbable would avoid a new clinical intervention for suture removal since the child presented noncompliant behavior.
The patient underwent six months of speech therapy after the frenectomy and returned for follow-up (Figure 7). From the functional perception of the Pediatric Dentistry clinic, the patient’s lingual motor functions were not corrected and a second opinion was requested. The second speech therapist evaluation was done by an expert linked to the USP.

This second speech therapist assessment was performed on the patient 14 months after surgery. Evaluating the functional tests, the speech therapist concluded that the patient had no alteration in speech even though the mobility of the tongue was impaired. However, chewing was considered inefficient for solid foods, and the functional difficulty of the patient was clear even after the favorable morphology of the tongue was established. The patient returned to perform speech therapy to improve chewing.
Discussion and conclusions
The clinical manifestations of JIA heterogeneous, the TMJ may be affected by JIA,2 and as a consequence, patients may present pain, noise, difficulty in chewing and limitation of oral opening.3Studies have found that more than 70% of the patients evaluated have structural condylar alterations in radiographic examinations, but not all have clinical signs.5 The patient in this case report had a controlled disease, with no complaint of pain in any joint. Approximately 50% of the children with JIA have the active disease in adult life.2 In the physical examination, the patient showed a maximum mouth opening of 28.0 mm and the limiting sign of the mouth opening is at <40 mm.17 This limitation may lead to greater difficulty in practicing correct oral hygiene, as this has been observed clinically and seen in other studies.3
The patient had difficulty performing correct oral hygiene with some specific points of plaque accumulation and gingivitis. However, there were no carious lesions. Lower gingival index, plaque index10 11 and gingival bleeding index18 were observed in individuals with JIA. The caries experienced did not show statistically significant differences between children with JIA and controls. 18,19
Although the pathogenesis of JIA is still not well understood, it is believed that all subtypes have autoimmune and inflammatory components. 1 Consequently, JIA is often treated with immunosuppressive agents. These therapeutic agents, as well as the disease process itself, may predispose children with JIA to a higher risk of infection than children without JIA.16 Therefore, the protocol recommended by the rheumatologist for antibiotic therapy, 24 hours before surgery for seven days, was used to perform the surgical procedure in the patient.
The patient was diagnosed with ADHD at the age of seven years, with no delay in school development, but an infantilized behavior was observed that was inappropriate for her age. Dental surgeons must be prepared for the care of children and adolescents with ADHD as they will cooperate less during dental treatment requiring more attention from the surgeon.19 20
Although this clinical case is of a girl, the sex most commonly affected by this disorder is the male sex. 8, 11,12 However, some believe girls are under-diagnosed for having more symptoms of inattention than hyperactivity.10
As previously mentioned, the patient presented deficiency in oral hygiene performance, most likely due to ADHD since her upper limbs were not affected by JIA. It was agreed among authors who advocate preventive dental care, that with regular dental visits and preventive measures, such as fluorotherapy, sealants, oral hygiene instruction and dietary guidelines for patients with ADHD 10 -12 that preventive dental care should remain during adolescence.8
There is a consensus that chewing, swallowing, and speech production are functions that may be influenced more by the ankyloglossia. 14, 21
In some situations, a surgical intervention is repeated to achieve successful mobility of the tongue.21 In the clinical case, after six months, although visually the lingual frenulum was not fully released, a speech therapist evaluated that it performs all the functional movements. Therefore, in addition to the surgical procedure, it is often necessary to complement the treatment with speech therapy.4
The multidisciplinary planning and execution of the clinical case was extremely important to maintain and preserve oral health without harming the patient’s systemic health.
Based on this case report, we can conclude that a dental surgeon’s knowledge about the oral manifestations of JIA is important. A greater attention to condylar alterations, radiographic examination and limitation of mouth opening is needed, and surgeons should know the risk of infection for these patients when undergoing surgical procedures. The behavioral characteristics of ADHD patients and their influence on oral health suggests the need for preventive strategies along with a reinforcement of oral hygiene until adolescence. In cases of ankyloglossia, the need for some patients to perform speech therapy after surgical procedure should be observed.
References
1. Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369:767-78.
2. Boros C, Whitehead B. Juvenile idiopathic arthritis. Aust Fam Physician. 2010;39:630-6.
3. Bhatt KH, Karjodkar FR, Sansare K, Patil D. Juvenile idiopathic arthritis. Contemp Clin Dent. 2014;5:89-91.
4. Bhattad MS, Baliga MS, Kriplani R. Clinical guidelines and management of ankyloglossia with 1-year followup: report of 3 cases. Case Rep Dent. 2013;2013:185803.
5. Abramowicz S, Kim S, Prahalad S, Chouinard AF, Kaban LB. Juvenile arthritis: current concepts in terminology, etiopathogenesis, diagnosis, and management. Int J Oral Maxillofac Surg. 2016;45:801-12.
6. Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387:1240-50.
7. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345-65.
8. Chau YC, Lai KY, McGrath CP, Yiu CK. Oral health of children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2017;125:49-54.
9. Modesto-Lowe V, Charbonneau V, Farahmand P. Psychotherapy for Adolescents with Attention- Deficit Hyperactivity Disorder: A Pediatrician’s Guide. Clin Pediatr (Phila). 2017;56:667-74.
10. Blomqvist M, Ahadi S, Fernell E, Ek U, Dahllöf G. Dental caries in adolescents with attention deficit hyperactivity disorder: a population- based follow-up study. Eur J Oral Sci. 2011;119:381-5.
11. Hidas A, Noy AF, Birman N, Shapira J, Matot I, Steinberg D, et al. Oral health status, salivary flow rate and salivary quality in children, adolescents and young adults with ADHD. Arch Oral Biol. 2011;56:1137-41.
12. Bimstein E, Wilson J, Guelmann M, Primosch R. Oral characteristics of children with attention- deficit hyperactivity disorder. Spec Care Dentist. 2008;28:107-10.
13. Jamilian A, Fattahi FH, Kootanayi NG. Ankyloglossia and tongue mobility. Eur Arch Paediatr Dent. 2014;15:33-5.
14. Suter VG, Bornstein MM. Ankyloglossia: facts and myths in diagnosis and treatment. J Periodontol. 2009;80:1204-19.
15. Walsh J, Links A, Boss E, Tunkel D. Ankyloglossia and lingual frenotomy: National trends in inpatient diagnosis and management in the United States, 1997- 2012. Otolaryngol Head Neck Surg. 2017;156:735-40.
16. Hurd A, Beukelman T. Infectious complications in juvenile idiopathic arthritis. Curr Rheumatol Rep. 2013;15:327.
17. Ortega AOL, Guimarães AS, Ciamponi AL, Marie SKN. Frequency of temporomandibular disorder signs in individuals with cerebral palsy. J Oral Rehabil. 2008;35:191- 5.
18. Santos D, Silva C, Silva M. Oral health and quality of life of children and adolescents with juvenile idiopathic arthritis according to their caregivers’ perceptions. Spec Care Dentist. 2015;35:272-8.
19. Feres de Melo AR, Ferreira de Souza A, de Oliveira Perestrelo B, Leite MF. Clinical oral and salivary parameters of children with juvenile idiopathic arthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2014;117:75- 80.
20. Carrillo DM, Marqués ML, Maroto EM, Cardoso SC, Barbería LE. Trastornos de la conducta en el niño y repercusión en la atención odontopediátrica. J Am Dent Assoc (edicion espanõla). 2009;4:250-5.
21. Klockars T, Pitkaranta A. Pediatric tongue- tie division: indications, techniques and patient satisfaction. Int J Pediatr Otorhinolaryngol. 2009;73:1399-401.
Gabriela Mancia de Gutierrez
E-mail address: gabrielamancia@hotmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Article history:
Received 14 May 2018
Accepted 20 November 2018
Available online 28 November 2018
