
Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (1) | 10-17
Original research
Characterization of recurrent aphthous stomatitis in a young population
Caracterização da estomatite aftosa recorrente numa população infantojuvenil
a Faculty of Dental Medicine, University of Porto, Porto, Portugal
Otília Pereira-Lopes - tilialopes@gmail.com
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 1
Original research
Pages - 10-17
Go to Volume
Article History
Received on 17/08/2017
Accepted on 14/06/2018
Available Online on 28/06/2018
Keywords
Original research
Characterization of recurrent aphthous stomatitis in a young population
Caracterização da estomatite aftosa recorrente numa população infantojuvenil
Maria João Oliveira, Filipe Coimbra, Pedro Mesquita, João Carvalho, Otília Pereira-Lopes*
Faculty of Dental Medicine, University of Porto, Porto, Portugal
http://doi.org/10.24873/j.rpemd.2018.06.222
Abstract
Aim: To characterize recurrent aphthousstomatitis in a young population and investigate the association between these lesions and predisposing factors, as well as potential modifications in children’s daily routines.
Methods: The data was collected by delivering a questionnaire to students attending S. Miguel Primary School, in Vizela, as well as to their parents/guardians. A literature review was conducted, using scientific databases such as PubMed, Cochrane and the Virtual Library of the University of Porto.
Results: A common prevalence of aphthousulcers was found in 53.0% of the sample. Most participants reported a number of lesions between 1 and 5, located in the jugal/labial mucosa, healing within 4 to 7 days. About 46.4% of the participants had a family history of this disease, mainly on the mother’s side. About 29.6% of the students associated aphthaewith traumatic events in the oral mucosa, while 9.8% associated them with stress. A significant association was found only between the frequency of aphthaeand gastrointestinal disorders, and not with other factors. A significant use of topical medications was detected, and the pharmacist was the most consulted healthcare professional.
Conclusion: This study’s findings were in line with previous data on the clinical characteristics of aphthaeand confirm the negative impacts of this disease on children’s quality of life, reporting its association with gastrointestinal disorders.
Keywords: Aphthae, Aphthous, Oral medicine, Recurrence, Stomatitis, Young
Resumo
Objetivo: Caracterizar a estomatite aftosa recorrente numa população infantojuvenil, averiguando a sua relação com fatorespredisponentes e possíveis modificações nas rotinas diárias das crianças.
Métodos: Os alunos da Escola Básica de S. Miguel, Vizela, e respetivosencarregados de educação foram submetidos a um questionário. Foi também realizada uma revisão da literatura nas bases de dados PubMed, Cochranee Biblioteca Virtual da Universidade do Porto.
Resultados: Foi determinada uma prevalência de aftas em 53,0% dos participantes, sendo que a maioria referiu um número de lesões entre 1 e 5, com localização na mucosa jugal/labial e com período de cicatrização de 4 a 7 dias. Cerca de 46,4% da amostra apresentou história familiar, tendo sido a mãe o progenitor mais indicado. Cerca de 29,6% dos inquiridos associaram a presença de aftas com eventos traumáticos na mucosa oral, enquanto 9,8% associaram com o stress. Foi apenas encontrada uma associação significativa entre a frequência de aftas e alterações gastrointestinais, não se verificando o mesmo com outros fatores. Verificou-se ainda uma utilização acentuada de medicamentos tópicos, sendo o farmacêutico o profissional de saúde mais consultado.
Conclusões: Os resultados deste estudo estão de acordo com a literatura quanto às características clínicas das aftas e quanto ao impacto negativo desta doença na qualidade de vida das crianças, verificando-se a relação com alterações gastrointestinais.
Introduction
The recurrent aphthousstomatitis (RAS) is the most common ulcerous disease of the oral mucosa. 1, 2 It usually onsets in childhood and affects about 25% of the world population. 3 - 6
Its typical lesions are well-circumscribed rounded ulcers surrounded by a peripheral halo of erythema, with a white/yellowish fibromembranous center. It has three main presentations: minor, major and herpetiform, of which the minor is the most common. In the minor presentation, the aphthaegenerally heal in 4 to 7 days without leaving a scar, while in the major presentation aphthaeneed a larger period and might leave a scar.3 - 6
The etiopathogeny of RAS is still unknown and is often multifactorial. Several factors have been suggested as triggering agents, including local factors, such as local trauma, which is considered an etiological agent of RAS in susceptible patients. 1, 7, 8
Regarding systemic factors, the infection by H. pylori has been reported as an etiological factor of RAS.9 The ulcerous colitis and the Crohn’sdisease have also been associated with the appearance of oral ulcers similar to the ones of RAS.1 Some authors state that patients with RAS have a higher prevalence of celiac disease and that RAS may be their first complaint. 10 - 13
The role of genetic factors is also important in the etiology of RAS, as it is thought that at least 40% of patients with RAS have a family history of that condition. These patients tend to develop RAS at an earlier age, with more-severe symptoms and frequent episodes. 4 - 6, 14, 15,
It is thought that some allergies can cause RAS. Hypersensitivity to some food components and oral microbial agents are considered potential etiological factors. 1, 16, 17
The association between RAS and some nutritional and blood deficits has been studied, and patients with RAS have been proved to present iron, B12 vitamin, folic acid and hemoglobin deficits more frequently.18 The fact that 5-10% of patients with RAS present low blood levels of folate, zinc, iron, and B1, B2, B6 and B12 vitamins may suggest these nutritional deficits as potential causes. 1, 19, 20
Stress-causing events were also subjectively found to be strongly associated with RAS episodes, but not with these episodes’ duration. Furthermore, it was demonstrated that experiencing a stress-inducing situation raises almost three times the odds of RAS occurring.21
Lastly, RAS treatment acts mainly on symptoms’ relief, and a topical approach is effective in most patients. Nevertheless, systemic treatment should be considered in patients with multiple episodes of minor RAS or patients with major RAS.1
The present work aims to characterize RAS in a young population, according to its frequency, location, painful symptomatology, applied therapies and time of healing. It also aims to study these lesions’ association with predisposing factors and potential changes in children’s daily routines.
Materials and methods
Information was obtained using a questionnaire that was completed by children from 3 to 11 years old who attended the S. Miguel Primary School (EscolaBásicade S. Miguel), in Vizela, and another questionnaire that was completed by the corresponding parents/guardians for validation of the answers.
To create the data extraction form and write the paper, the authors conducted a comprehensive literature review using the PubMed and Cochrane databases, as well as the Virtual Library of the University of Porto, introducing and combining the following keywords “recurrent aphthousstomatitis” , “gastrointestinal”, “trauma”, “questionnaire”, “inquiry” and “questions”. The following inclusion criteria were defined for the selection of the articles: full text available, publication in the last 5 years, and article written in English, Portuguese or Spanish. Subsequently, studies essential for a better understanding of the subject were found in the references of the articles obtained in the first selection, and were included due to their relevance and extreme importance for the correlation between the results obtained and the existing knowledge in the literature.
A meeting was held with the Board of the Schools Group of Infias(which includes the S. Miguel Primary School), in which the whole study was explained, and the authors were authorized to conduct it. Then, the questionnaires were delivered to the students, under the researcher’s guidance. Considering that the children’s answers could be difficult to assess, certain instruments were included in the questionnaire elaboration to simplify the understanding of the questions, such as cards with illustrative images (including examples of aphthae in the oral cavity and foods such as green vegetables and legumes) and an adapted pain scale22 to aid its interpretation.
Later, with the teachers’ help, the questionnaires were handed to the parents or guardians of each participating child, who were asked to complete them at home and then deliver them at the school. After every questionnaire had been delivered to the school, they were all handed to the researcher.
This research was approved by the Ethics Committee of the Faculty of Dental Medicine of the University of Porto. Every data were collected after obtaining written consent for participation in the study, as established by the Declaration of Helsinki.
Statistical analysis was conducted using the IBM SPSS 23.0 and the Microsoft Office Excel 2013 software. After applying the Cronbach’salpha test, seven questions used in both questionnaires were validated for reliability (α > 0.8). The chi-square test was used to analyze the association between certain variables (association between aphthaeand predisposing factors such as gastrointestinal disorders, allergies, daily toothbrushingfrequency, use of orthodontic appliance, placement of pens/pencils in the oral cavity and consumption of some foods). A significance level of 5% was used in every test.
Results
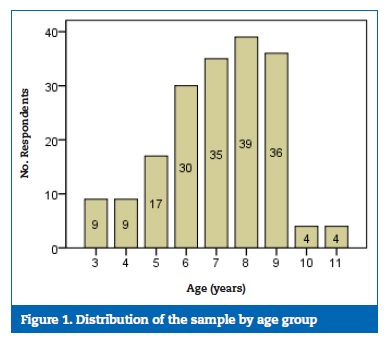
This study included 183 children (91 male and 92 female) aged between 3 and 11 years (Figure 1).
The children’s responses were found to be in agreement with their parents’ responses, since the Cronbach’s alpha test gave alpha values higher than 80% for the seven questions that allowed this validation.
A prevalence of aphthae was found in 53.0% of the participants (Table 1), showing an odds ratio of 1.33 (0.743;2.378).

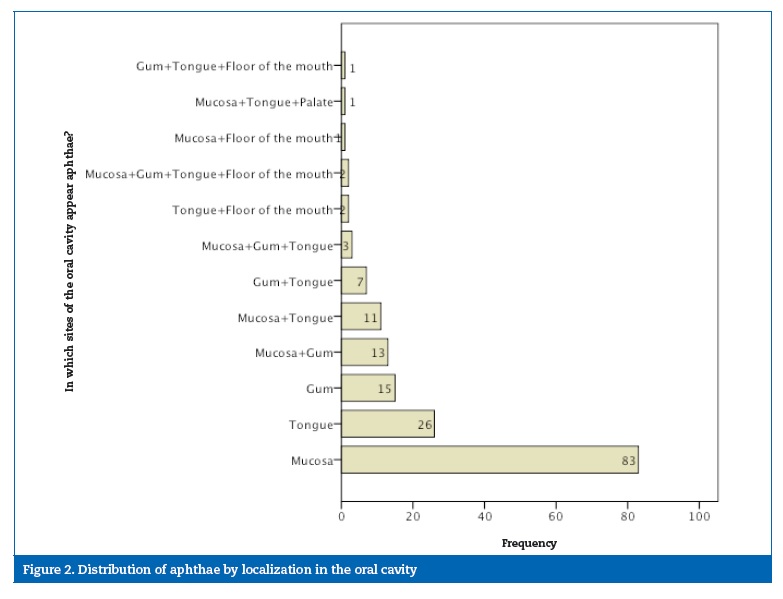
Girls had aphthaemore often than boys, with most of them reporting 1 to 5 lesions (95.8%), located in the jugal/labial mucosa (67.3%) (Figure 2) and taking 4 to 7 days to heal (92.8%).
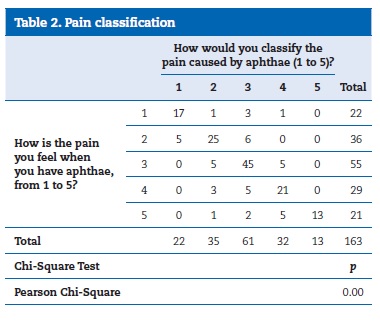
The most frequent answer (33.7% of children; 37.4% of parents) to the pain scale used in the questionnaire was number 3 – moderate pain (Table 2). The chi-square test was used to analyze the association between the children’s and parents’ answers, which were in agreement (p-value <0.01%).
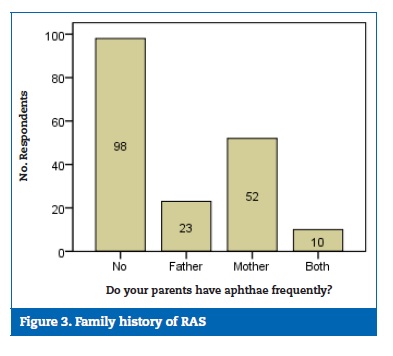
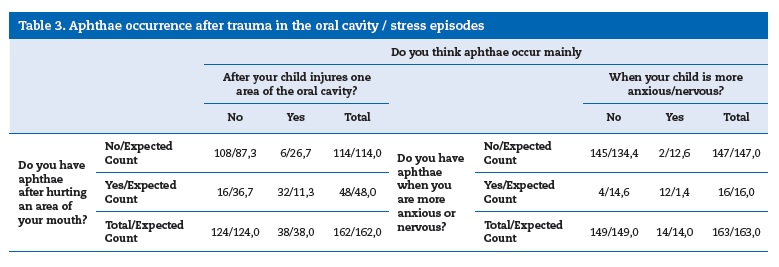
Approximately 46.4% of participants had a family history of RAS (Figure 3), mainly on the mother’s side. Around 29.6% of the students associated the presence of aphthaewith traumatic events on the oral mucosa (Table 3), showing an odds ratio of 36.0 (13.010;99.617), i.e., the likelihood of parents perceiving aphthaeas occurring in children after an injury to the oral cavity was 36 times higher when their children also considered it compared to when they did not. On the other hand, 9.8% associated aphthaewith stress-causing events (Table 3), showing an odds ratio of 217.55 (36.076;1311.309), i.e., the likelihood of parents considering that aphthae appeared in their children when they were anxious/nervous was manifestly superior when their children also considered it comparing to those who did not.
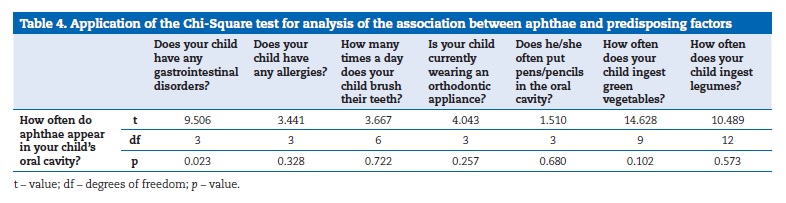
A significant association was found between the frequency of aphthae and gastrointestinal disorders (p = 0.023). However, the aphthae’sassociation with allergies or other factors such as daily toothbrushingfrequency, use of orthodontic appliance, placement of pens/pencils in the oral cavity and consumption of some foods (vegetables, legumes) was not statistically significant (Table 4).
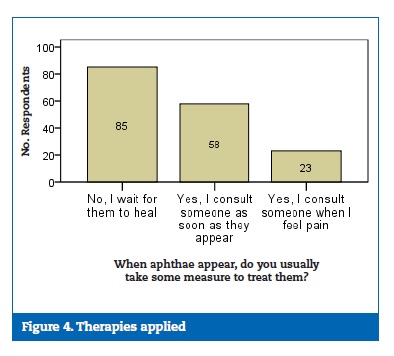
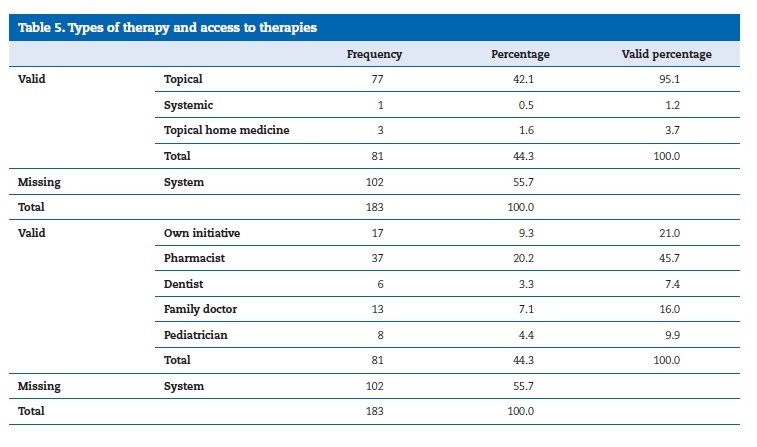
Although most of the respondents referred not applying any treatment (Figure 4), a marked use of topical drugs was found, with the pharmacist being the most consulted healthcare professional (Table 5).
Discussion
In this study, 97 children (53.0% of the study population) stated having aphthaeregularly. Although this is not a real prevalence, the obtained percentage for aphthaeoccurrence is similar to the one described by Rogers,23who indicates that the prevalence of RAS may vary between 5% and 50%, depending on the studied population. According to the same author, females are more affected by this condition.23 Nevertheless, no association was found between aphthaeoccurrence and gender in the present study.
Most of this research’s participants stated that the number of lesions in each RAS episode was between 1 and 5. Moreover, most of them also indicated a time of healing of 4 to 7 days.
These results suggest that the majority of the participants probably had a minor manifestation of RAS, which, according to Rogers,24 is the most common one and is characterized by a number of lesions between 1 and 5. The corresponding time of healing is also consistent with the literature.25 Regarding the lesions’ localization, this study revealed that RAS appeared in any area of the oral cavity and that the most frequent localization was the jugaland labial mucosa, which is consistent with other studies published by several authors. 3 - 5, 26
In the study by Gavicet al.,27 a pain scale of 0 to 10 (with 0 corresponding to slight pain/burn and 10 corresponding to extreme pain) was applied, with 7 being the most indicated number, which is close to extreme pain. In the young population of this study, using a simplified pain scale (from 1 to 5, with 1 corresponding to no pain and 5 to intense pain), the most indicated response by the children was number 3 (Table 2). These results suggest that in younger age groups the pain felt in the presence of these lesions is considered moderate.
Krisdapong etal.28 concluded that RAS has an impact on oral hygiene and dietary habits. The same was verified in this study, as approximately 60 of the parents/guardians claimed that their children avoided brushing the areas affected by aphthae.
This finding suggests that children do not brush their teeth effectively in the areas near the lesions, so as to avoid the pain. Furthermore, 60.9% of the parents/guardians stated that their children had difficulty chewing food. These findings are consistent with the literature, where RAS is described as painful and capable of creating difficulties in daily activities such as talking, laughing and chewing. 4, 28, 29
In this research, 46.4% of the students had a family history of RAS. This percentage is higher than the one presented by Gurkan et al.,15where 35.8% of the patients had a family history of RAS. This difference might be explained by the fact that the studied age groups were more limited in the present research (3-11 years) in comparison with the ones studied by Gurkanetal.15 (2-17 years). The present study also revealed that, of both parents, the mother seemed to contribute more to the family history of this condition.
In the young population of this study, 48 participants (29.6% of the sample) reported episodes of RAS associated with a previous trauma in the oral cavity. The percentage obtained in this regard was lower than the one detected by Wray etal.8 (43.3%). On the other hand, only 9.8% of the participants reported episodes of stress associated with the occurrence of aphthae. This result reflects an association between stress and RAS less frequent than the one presented by Bratel and Hakeberg,30in whose study 15.8% of the patients indicated stress as a potential etiological factor for aphthaedevelopment.
These results may be explained by the fact that the studies found in the literature included samples that were essentially composed of adults, whereas the present study focuses on a markedly younger population.
In the present study, a significant association was found between the frequency of aphthaeand gastrointestinal disorders.
However, the aphthae’sassociation with allergies, daily toothbrushingfrequency, useof orthodontic appliance, placement of pens/pencils in the oral cavity and consumption of some foods (green vegetables and legumes) were not statistically significant. Only 6.0% of the studied sample presented some gastrointestinal disorders. This percentage is inferior to the one reported in the study by Diaz et al.,31where 35.8% of the studied cases showed gastrointestinal disorders (namely, gastroenteritis, malabsorptionsyndrome, ulcerous colitis and giardiasis). However, it is important to note that the study by Diaz etal.31 included adult patients, whereas the present research focused on a much younger population.
Regarding the therapies used, most of the parents/guardians indicated that they did not apply any type of treatment and waited for the lesions to heal spontaneously. These actions may result from the fact that there is not yet a definitive treatment protocol for RAS.32 According to Ranganath and Pai,32this situation is explained by the lack of clinical trials and the differences in response between different patients.
Nevertheless, it may also be explained by the fact that the exact etiology of RAS is still unknown.23
Of the group who stated applying some therapy, most used topical drugs (namely, drugs including hyaluronic acid), which is consistent with the existing literature, where topical drugs are described as the therapy of choice for most patients with RAS. 3, 33
Regarding the access to these drugs, many of the respondents had consulted a pharmacist. Only 7.4% of the participants reported having consulted the dentist, which is a lower percentage than what was expected, considering that the dentist is the healthcare professional with the most adequate knowledge for the diagnosis and treatment of this type of lesions.
One of this study’s limitations was the fact that the information was obtained only using a questionnaire, without any complementary clinical observation. Furthermore, it was not possible to distinguish between aphthae(clinical situations of RAS) and traumatic ulcers. There is a need for more studies that include evaluating the influence of the predisposing factors in the development of RAS. More studies about how this condition affects the daily routines and the quality of life, as well as the therapies usually used, are also required to allow a more effective action to understand this condition.
Conclusions
This study’s results are consistent with the literature regarding aphthae’sclinical features. The previously referred association between aphthaeand gastrointestinal disorders was shown in this study.
An association between traumatic events in the oral mucosa or stress episodes and the development of aphthae was also found, although in a less frequent proportion than in other previous studies.
A marked percentage of family history was detected, mainly on the mother’s side, thus reinforcing the pertinence of further exploring this line of research. This research also allowed to reinforcethe information in the literature about the negative impact of this condition on the quality of life, as well as the preference for topical therapies.
References
1. AkintoyeSO, GreenbergMS. Recurrent aphthous stomatitis. Dent Clin North Am. 2014;58:281-97.
2. Porter SR, Scully C, Pedersen A. Recurrent aphthousstomatitis. CritRev Oral BiolMed. 1998;9:306-21.
3. LandovaH, DanekZ, GajdziokJ, VetchyD, StembirekJ. Oral mucosa and therapy of recurrent aphthousstomatitis. Ceska SlovFarm.2013;62:12-8.
4. Scully C, Porter S. Oral mucosal disease: recurrent aphthousstomatitis. Br J Oral Maxillofac Surg. 2008;46:198-206.
5. JurgeS, KufferR, Scully C, Porter SR. Mucosal disease series. Number VI. Recurrent aphthousstomatitis. Oral Dis. 2006;12:1-21.
6. ChavanM, Jain H, DiwanN, KhedkarS, SheteA, DurkarS. Recurrent aphthousstomatitis: a review. J Oral Pathol Med. 2012;41:577-83.
7. HulingLB, BaccagliniL, ChoquetteL, FeinnRS, LallaRV. Effect of stressful life events on the onset and duration of recurrent aphthousstomatitis.J Oral PatholMed. 2012;41:149-52.
8. Wray D, GraykowskiEA, NotkinsAL. Role of mucosal injury in initiating recurrent aphthousstomatitis. Br Med J (ClinRes Ed). 1981;283(6306):1569-70.
9. Gomes CC, GomezRS, Zina LG, Amaral FR. Recurrent aphthous stomatitis and Helicobacter pylori. Med Oral Patol Oral CirBucal. 2016:e187-e91.
10. Ferguson R, BasuMK, Asquith P, Cooke WT. Jejunalmucosal abnormalities in patients with recurrent aphthousulceration. Br Med J. 1976;1(6000):11-3.
11. Ferguson MM, Wray D, Carmichael HA, Russell RI, Lee FD. Coeliac disease associated with recurrent aphthae. Gut.1980;21:223-6.
12. JokinenJ, Peters U, Maki M, MiettinenA, Collin P. Celiac spruein patients with chronic oral mucosal symptoms. J ClinGastroenterol. 1998;26:23-6.
13. deFreitas IN, SipahiAM, DamiaoAO, de Brito T, Cancado EL, LeserPG, etal.Celiac disease in Brazilian adults. J ClinGastroenterol. 2002;34:430-4.
14. KoybasiS, ParlakAH, SerinE, YilmazF, SerinD. Recurrent aphthousstomatitis: investigation of possible etiologic factors. Am J Otolaryngol.2006;27:229-32.
15. GurkanA, OzluSG, Altiaylik-OzerP, KurtulBE, KaracanCD, SenelS. Recurrent Aphthous Stomatitis in Childhood and Adolescence: A Single-Center Experience. Pediatr Dermatol. 2015;32:476-80.
16. Wray D, VlagopoulosTP, SiraganianRP. Food allergens and basophil histamine release in recurrent aphthousstomatitis. Oral SurgOral Med Oral PatholOral RadiolEndod.1982;54:388-95.
17. HasanA, ShinnickT, MizushimaY, van der Zee R, LehnerT. Defining a T-cell epitope within HSP 65 in recurrent aphthousstomatitis. ClinExpImmunol. 2002;128:318-25.
18. Sun A, Chen HM, Cheng SJ, Wang YP, Chang JY, Wu YC, et al. Significant association of deficiencies of hemoglobin, iron, vitamin B12, and folic acid and high homocysteine level with recurrent aphthousstomatitis. J Oral PatholMed. 2015;44:300-5.
19. Dar-OdehNS, AlsmadiOM, BakriF, Abu-HammourZ, ShehabiAA, Al-OmiriMK, et al. Predicting recurrent aphthous ulceration using genetic algorithms-optimized neural networks. AdvApplBioinforma Chem. 2010;3:7-13.
20. KozlakST, Walsh SJ, LallaRV. Reduced dietary intake of vitamin B12 and folatein patients with recurrent aphthousstomatitis.J Oral PatholMed. 2010;39:420-3.
21. Keenan AV, Spivakovksy S. Stress associated with onset of recurrent aphthous stomatitis. J EvidBased Dent Pract. 2013;14:25.
22. Buchanan H, NivenN. Validation of a Facial Image Scale to assess child dental anxiety. IntJ PaediatrDent. 2002;12:47-52.
23. Rogers RS 3rd. Recurrentaphthousstomatitis: clinical characteristics and associated systemic disorders. SeminCutan Med Surg. 1997;16:278-83.
24. Rogers RS, 3rd. Recurrent aphthousstomatitis: clinical characteristics and evidence for an immunopathogenesis. J Invest Dermatol. 1977;69:499-509.
25. Cui RZ, Bruce AJ, Rogers RS 3rd. Recurrentaphthousstomatitis. ClinDermatol. 2016;34:475-81.
26. Ship JA. Recurrent aphthousstomatitis.An update. Oral SurgOral Med Oral PatholOral RadiolEndod.1996;81:141-7.
27. GavicL, CigicL, BiocinaLukendaD, GrudenV, GrudenPokupecJS. The role of anxiety, depression, and psychological stress on the clinical status of recurrent aphthousstomatitis and oral lichen planus.J Oral Pathol Med. 2014;43:410-7.
28. KrisdapongS, SheihamA, TsakosG. Impacts of recurrent aphthousstomatitis on quality of life of 12- and 15-year-old Thai children. QualLife Res. 2012;21:71-6.
29. Greenberg M. Ulceration, vesicular and bullous lesions. In M. Greenberg & M. Glick (Eds.), Burket’scheck spelling oral medicine.Diagnosis and treatment (pp. 63–65).2003;Ontario: BC Decker Inc.
30. BratelJ, HakebergM. Anamnestic findings from patients with recurrent aphthousstomatitis. Swed Dent J. 2014;38:143-9.
31. Diaz A, Pereira-Lopes O, Barbosa E, MesquitaP, Coimbra F. Behavior of the recurrent aphthousstomatitis as a dental urgency at Vedado’sUniversity Polyclinic. Rev Port Estomatol Med Dent Cir Maxilofac.2015;56:144-8.
32. RanganathSP, PaiA. Is Optimal Management of Recurrent AphthousStomatitis Possible? A Reality Check.J ClinDiagnRes. 2016;10(10):ZE08-ZE13.
33. Belenguer-GuallarI, Jimenez-Soriano Y, Claramunt-Lozano A. Treatment of recurrent aphthousstomatitis. A literature review.J ClinExpDent.2014;6:e168-74.
Otilia Pereira-Lopes
Correio eletronico: tilialopes@gmail.com
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgments
The collaboration of the Board of the Schools Group of Infiasand every pre-school and primary education teacher of the S. Miguel Primary School’s, who contributed significantly in the process of distributing and collecting the questionnaires, made this work possible, and we express our sincere gratitude to all of them.
Appendices
Supplementary content associated with this article can be found, in the online version, at http://doi.org/10.24873/j.rpemd.2018.06.222.
Article history:
Received 17 August 2017
Accepted 14 June 2018
Available online28 June2018
