Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial
SPEMD - Rev Port Estomatol Med Dent Cir Maxilofac | 2018 | 59 (1) | 24-29
Original research
Concordance analysis between two questionnaires of self-reported bruxism
Analise de concordância entre dois questionários para auto relato de bruxismo
a Clínica privada, Porto Alegre, RS, Brasil
b Faculdade de Odontologia, Universidade Luterana do Brasil, Torres, RS, Brasil
c Faculdade de Odontologia, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brasil
Rosemary Sadami Arai Shinkai - rshinkai@pucrs.br
Article Info
Rev Port Estomatol Med Dent Cir Maxilofac
Volume - 59
Issue - 1
Original research
Pages - 24-29
Go to Volume
Article History
Received on 14/02/2018
Accepted on 24/05/2018
Available Online on 21/06/2018
Keywords
Original research
Concordance analysis between two questionnaires of self-reported bruxism
Analise de concordância entre dois questionários para auto relato de bruxismo
Helena LenzPiúmaa, Gustavo FrainerBarbosab, Eduardo AydosVillarinhoc, Rosemary SadamiArai Shinkaic,*
aClínica privada, Porto Alegre, RS, Brasil
bFaculdade de Odontologia, Universidade Luterana do Brasil, Torres, RS, Brasil
cFaculdade de Odontologia, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS, Brasil
http://doi.org/10.24873/j.rpemd.2018.06.219
Abstract
Objectives: Consensus has not been reached regarding the diagnosis of bruxism. The present study analyzed the agreement between two self-reporting questionnaires for the diagnosis of possible bruxism.
Methods: A non-probabilistic consecutive sample was selected among adult patients treated with implant-supported fixed prosthesis from 2010 to 2016. The sample consisted of 65 patients (42 women) undergoing oral rehabilitation with fixed implant-supported prostheses, who answered two structured questionnaires (Q1 and Q2) for the diagnosis of bruxism. Data were tested for agreement between both questionnaires using the Cohen’s kappa coefficient.
Results: The results showed a fair agreement (kappa = 0.356) between the two self-reporting questionnaires. Only 50% of the patients with a positive bruxism diagnosis in Q1 had the same diagnosis in Q2 and 46% with a positive diagnosis in Q2 had a similar result in Q1. Regarding the negative diagnosis of bruxism, 87% of patients with a negative diagnosis in Q1 also had a negative diagnosis in Q2, and 88% with a negative diagnosis in Q2 had a similar diagnosis in Q1.
Conclusion: The results suggest that, although the use of self-reporting questionnaires for bruxism is a clinically easy method to apply in research and dental practice, this method presents limitations for obtaining a precise diagnosis of possible bruxism.
Keywords: Agreement, Bruxism, Diagnosis
Resumo
Objetivo: Ainda não há um consenso sobre a fisiopatogeniae o diagnóstico de bruxismo. Este estudo analisou a concordância entre dois questionários de auto-relato para diagnóstico de “possível” bruxismo.
Métodos: Uma amostra consecutiva não probabilística foi constituída por pacientes reabilitados com prótese fixas sobre implantes de 2010 a 2016. A amostra foi constituída por dados de 65 pacientes (42 mulheres) em tratamento para reabilitação com próteses sobre implantes, que responderam dois questionários padronizados para diagnóstico de bruxismo. Os dados foram analisados de forma descritiva e por teste de concordância com coeficiente Kappa.
Resultados: Observou-se que 50% dos pacientes com diagnóstico positivo em Q1 também tiveram no Q2. Um total de 46,1% dos pacientes que tiveram diagnóstico positivo em Q2 também tiveramno Q1. Para o diagnóstico negativo de bruxismo, 86,79% dos pacientes com diagnóstico negativo em Q1 também tiveram no Q2 e 88,46% dos pacientes com diagnóstico negativo em Q2 também tiveram no Q1. Os resultados mostraram uma baixa-moderada concordância (Kappa= 0,356) entre os dois questionários de auto-relato.
Conclusões: Os resultados sugerem que, embora o uso de questionários de auto-relato de bruxismo seja um método de fácil aplicação clínica, os instrumentos são limitados para um preciso diagnóstico “possível” de bruxismo.
Palavras-chave: Concordância, Bruxismo, Diagnóstico
Introduction
Bruxism is a repetitive muscle activity characterized by the grinding and/or clenching of the teeth when awake or sleeping.1 Sleep bruxism is an unconscious activity of grinding and/or tightening the teeth while the individual is sleeping, while diurnal bruxism is a semi-voluntary activity of the mandible characterized by the act of clenching both dental arches.1, 2, 3 Bruxism is considered a potential factor of temporomandibular disorders, muscle pain, dental wear, failure of restorations and dental prostheses, and loss of periodontal support.1 In addition, excessive occlusalload has been suggested to lead to peri-implant bone loss or even failure of dental implants and increased rates of complications.3
It is still controversial whether bruxism should be categorized as a habit, a disorder, or a risk factor for other disorders. Although an international consensus on the subject was published in 2013,1 other authors argue that there is insufficient evidence supporting the notion that bruxism is a disease per se or a risk factor for other disorders.4 The prevalence of bruxism is also unclear, but it is believed to be present in 6%-20% of the general population, affecting 14%-20% of children under 11 years, 5%-8% of the adult population,7 and as low as 3% of individuals over 60 years,8 thus showing a decreasing trend over time.
The methods for diagnosing bruxism include self-reporting, clinical examination of dental wear,and examination with specific devices in sleep laboratories (polysomnography). Electrophysiologic monitoring systems enable a definitive diagnosis and are used in sleep clinics or as portable devices. 8 - 10 Laboratory recording methods include electroencephalogram (EEG), electromyography (EMG), electrocardiogram (ECG), and thermal sensors with simultaneous audio-video recordings. 8, 9
However, these methods also have their limitations, including the necessity for the patient to leave their habitual environment and spend the night in sleep laboratories.10 On the other hand, the use of portable devices does not allow simultaneous audio-video recordings, thus causing bruxism to be confused with other orofacial activities (sighs, cough, speech).8
On clinical examination, the presence of tooth wear may indicate that the patient suffers from bruxism.8, 9 Such wear and tear must be differentiated from that of individuals with other harmful habits and/or excessively acidic diets. Although dental wear may aid in the clinical diagnosis of bruxism, it is usually considered a secondary factor.9 Itmay indicate that the patient has a history of bruxism but not necessarily that they currently suffer from bruxism. Also, about 40% of the population without bruxism developdental wear and tear over time.11 Hypertrophy of the masseter muscle can also be considered a secondary factor and should be differentiated from inflammatory edema, tumors, and other syndromes.8
Several different instruments have been developed for the diagnosis of sleep and diurnal bruxism, such as self-reporting questionnaires. Self-reporting questionnaires are a practical method for large-scale use; however, their highly subjective nature is a limitation.1 Todate, there is no consensus on which questionnaire would be the most appropriate for the diagnosis of bruxism or for comparative studies of different self-reporting instruments. Consistency between the existing self-reporting questionnaires on bruxism may allow this method to provide potentially useful information for research and daily clinical practices. Therefore, this study aimed to compare two self-reporting questionnaires for diagnosing bruxism, by testing if there is agreement between the two questionnaires.
Materials and methods
This cross-sectional and correlational study used a database derived from two clinical research projects on implant-supported prostheses, which were approved by the institutional ethics committee of the Pontifical Catholic University of Rio Grande do Sul, in Porto Alegre, Brazil, and registered in a National System of Information on Ethics for Researchin Humans.
The non-probabilistic consecutive sample was selected among adult patients treated from 2010 to 2016. Data from 65 adult patients (42 women) were obtained from the database and used for this study. Bruxism data were collected using two self-reporting questionnaires on bruxism (Figures 1 and 2). 2, 12
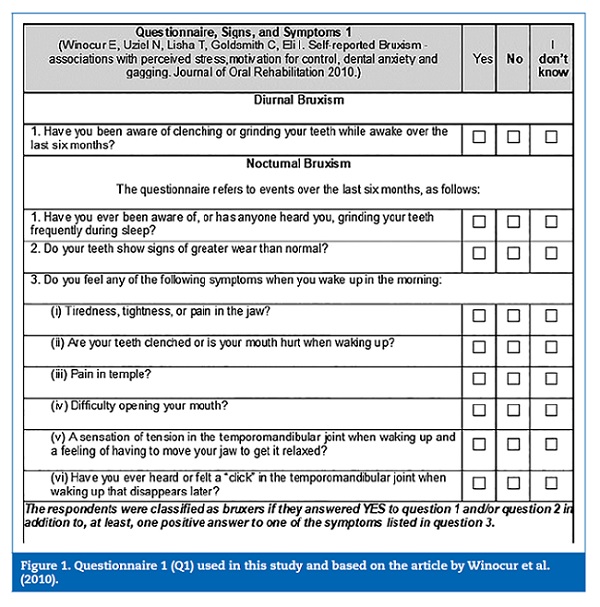
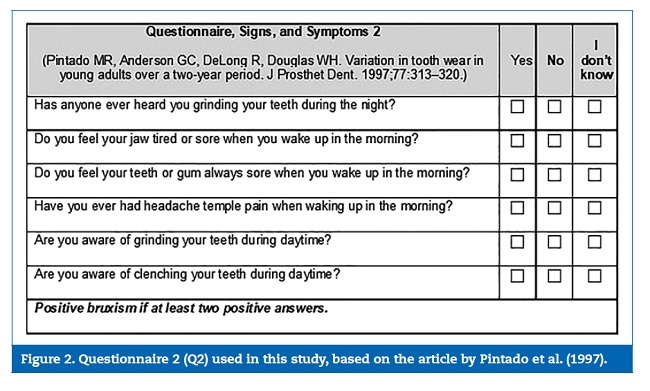
The patients’ categorical responses (“yes,” “no,” “I do not know”) to each question of the two questionnaires were computed as described in the original papers. The criteria established in each of the questionnaires were used to determine the presence or absence of bruxism. In Q1,12 the result was positive for bruxism when the patient responded positively to question 1 and/or question 2 and gave at least one positive response to one of the symptoms listed in question 3. In Q2,2 the result was positive for bruxism when the answer was positive to two out of the four existing questions.
Two diagnoses of “possible” bruxism were obtained for each patient using Q1 and Q2. The number of patients with a positive diagnosis, the number of patients with a negative diagnosis, and the number of patients with the same diagnosis in both questionnaires were calculated. The questionnaires were translated from English into the local language (Portuguese) and revised by a language expert (Appendixes 1 and 2).
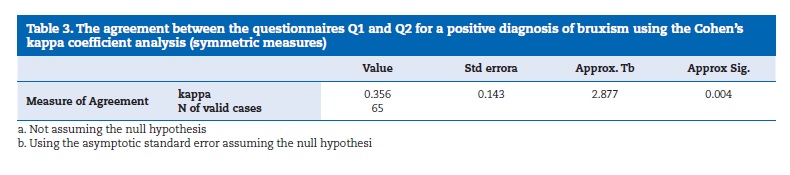
Data were statistically analyzed by descriptive statistics, and Cohen’s kappa coefficient was used to assess agreement between Q1 and Q2. The Cohen’s kappa coefficient result was interpreted as follows: values ≤ 0 as indicating no agreement and 0.01-0.20 as none to slight, 0.21-0.40 as fair, 0.41-0.60 as moderate, 0.61-0.80 as substantial, and 0.81-1.00 as almost perfect agreement. 13, 14
Results
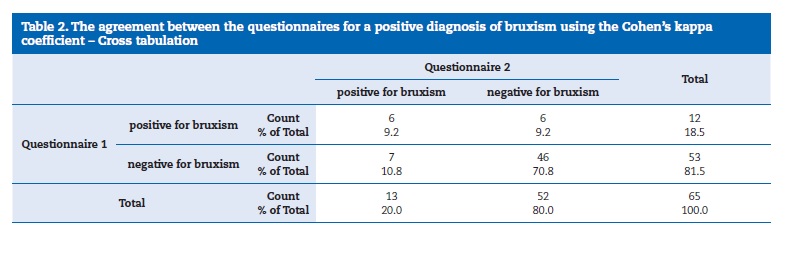
Nineteen out of 65 patients had a positive diagnosis of bruxism in at least one of the questionnaires (Table 1). However, only six of these 19 patients (9%) had a positive diagnosis in both questionnaires, while the other 13 had a positive result in only one of the questionnaires. In total, twelve patients (18%) had a positive diagnosis for bruxism in Q1 and 13 patients (20%) in Q2. Thus, 46 patients (71%) had a negative diagnosis of bruxism in both questionnaires.
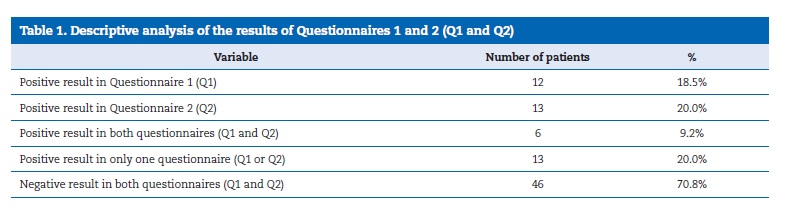
Considering the number of patients with a positive diagnosis of bruxism in each questionnaire and comparing the number of patients who had a positive diagnosis in both questionnaires, 50% of patients with a positive diagnosis in Q1 also had a positive diagnosis in Q2. On the other hand, 46% of patients with a positive diagnosis in Q2 also had a positive diagnosis in Q1. Regarding the negative diagnosis of bruxism, 87% of patients with a negative diagnosis in Q1 also had a negative diagnosis in Q2, and 88% of patients with a negative diagnosis in Q2 had similar results in Q1.
The agreement between the questionnaires for a positive diagnosis of bruxism using the Cohen’s kappa coefficient (Tables 2 and 3) was 0.356.
Discussion
The two self-reporting questionnaires on bruxism analyzed in this study showed a fair-to-low agreement. The questionnaires presented a higher agreement for the absence than for the presence of bruxism. Only six out of 65 patients (9%) had a positive diagnosis of bruxism in both questionnaires. Similarly, it has been reported that 6 to 20% of the general population is estimated to have bruxism.7
It was surprising that the two tested questionnaires with similar questions raised such a low agreement. A different understanding of the questions or lack of attention may have potentially influenced individual responses. One of the questions asked whether someone had already reported hearing the patient grinding their teeth, but this information may not be available for patients who sleep alone or cannot ask another person. Another limiting factor of this type of methodology is the individual’s perception of the symptoms, since waking up with a headache may be associated with other pathologies and, in addition, such symptoms may already be part of the patient’s routine.8
The results may have also been influenced by the possibility of answering “I do not know,” in addition to the dichotomous “yes” or “no” answer. The possibility of answering “I do not know” may have generated a biased response by encouraging the patients’ noncompliance and by not encouraging them to give the topic a thorough thought. Mathematically, when only the dichotomous “yes/no” option is available, the probability of a positive response is 50%, while with three options,this probability drops to 33%.
An international consensus has proposed bruxism to be classified as “possible,” “probable,” or “definitive,” and self-reported bruxism to be considered as a “possible” diagnosis of bruxism.1 Although the self-reporting questionnaire is a practical instrument for large-scale studies, its subjective nature carries the risk of overestimating or underestimating the presence of bruxism. 1, 4 However, most studies on bruxism and temporomandibulardisorders have used this method. 15, 17
In a meta-analysis18 conducted to validate different forms of diagnosing sleep bruxism – questionnaires, clinical assessment and portable diagnostic devices, these three methods were compared to the reference standard method polysomnography.
Based on the available evidence at the time, that meta- analysis concluded that questionnaires and clinical assessment could be used as screening methods to identify a negative diagnosis of sleep bruxism but were not that good in identifying a positive one. Despite not being very recent, the following diagnostic criteria for sleep bruxism of the American Academy of Sleep Medicine19 are still very much cited: a) the patient has a complaint of tooth-grinding or tooth-clenching during sleep; b) one or more of the following occurs: abnormal wear of the teeth, sounds associated with bruxism and/or jaw muscle discomfort; c) polysomnographicmonitoring demonstrates both of the following: jaw muscle activity during the sleep period and absence of associated epileptic activity; d) no other medical or mental disorders (e.g., sleep-related epilepsy, accounts for the abnormal movements during sleep); e) other sleep disorders (e.g., obstructive sleep apnea syndrome, can be present concurrently). The minimal criteria for a positive diagnosis of bruxism isA plus B.
Because of its multifactorial nature, bruxism may frequently appear in a patient’s daily life, and a longer follow-up of the case is considered important. Accordingly, some studies have suggested the use of an interview instead of a questionnaire, as the first provides more complex responses, and a sleep diary, which can be useful for assessing individual cases and the corresponding treatment.17 Enquiringthe patient about the presence or absence of tooth wear does not seem reliable. Currently, approximately 40% of the population without bruxism shows similar wear patterns, thus indicating a history of bruxism. 8, 11 Also, this wear only differs between people with and without bruxism after two years.2
For a “probable” diagnosis of bruxism to be obtained,1 besides conducting a clinical examination, it is necessary to apply an easy-to-understand questionnaire that will reach the population homogeneously and has few questions or even only one question requiring a categorical yes/no response. This way, it is possible to identify a patient with bruxism more promptly without the need for tests that require more time and increased patient availability, such as the polysomnography.15 In addition, the polysomnographypresents several methodological limitations.
When evaluating both the questionnaires and the findings of this study, some questions may be considered as having higher “possible” diagnostic value for bruxism. Among them is the question of whether the patient remembered feeling orofacialmuscle fatigue upon waking up and whether they were aware of grinding or clenching their teeth during the day or while sleeping. Regarding the first question, since bruxism is characterized by an involuntary movement of the mandible caused by contractions of the masticatory muscles, it is believed that there would be painful sensitivity in the masseter region and difficulty opening the mouth upon awakening.3 However, masseter muscle hypertrophy should be differentiated from inflammatory edema, tumors, and other syndromes,8 which should be discarded during the anamnesis. The second question is frequently found in self-report questionnaires of bruxism since noise production during sleep is a common sign of bruxism.
However, the response to this question may be compromised in cases where the patient sleeps alone or removes the prosthesis to sleep, or where their partner is a deep sleeper.8
Conclusions
The two self-reporting questionnaires analyzed showed fairto-low agreement, which indicates limitations in their use to diagnose “possible” bruxism. Although questionnaires are a simple and easy method to apply in research and dental practice, the outcome depends heavily on the understanding and truthfulness of the patient in answering the questions. Further research is required to refine self-reported bruxism questionnaires to attain a simple and more predictable method to diagnose“possible” bruxism.
References
1. LobbezooF, AhlbergJ, GlarosAG, Kato T, KoyanoK, LavigneGJ, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40:2-4.
2. PintadoMR, Anderson GC, Delong R, Douglas WH. Variation in tooth wear in young adults over a two-year period.J Prosthet Dent.1997;77:313-20.
3. Kato T, Yamaguchi T, Okura K, Abe S, LavigneGJ. Sleep less and bite more: Sleep disorders associated with occlusal loads during sleep. J ProsthodontRes. 2013;57:69-81.
4. Raphael QG, Santiago V, LobbezooF.Is bruxism a disorder or a behaviour? rethinkingthe international consensus on defining and grading of bruxism. J Oral Rehabil.2016;43:791-8.
5. LobbezooF, BrouwersJEIG, CuneMS, NaeijeM. Dental implants in patients with bruxinghabits. J Oral Rehabil.2006;33:152-9.
6. ChrcanovicBR, KischJ, AlbrektssonT, WennerbergA. Bruxism and dental implant treatment complications: a retrospective comparative study of 98 bruxerpatients and a matched group. ClinOral ImplRes. 2017;28:1-9.
7. LobbezooF, LavigneGJ, TanguayR, MontplaisirJY. The effect of catecholamine precursor L-dopa on sleep bruxism: a controlled clinical trial. MovDisord. 1997;12:73-8.
8. Kato T, ThieNMR, MontplaisirJY, LavigneGJ. Bruxism and Orofacial Movements DuringSleep. Dent Clin North Am. 2001;45:657-84.
9. KoyanoK, TsukiyamaY, IchikiR, KuwataT. Assessment of the Bruxism in the Clinic. J. Oral Rehabil. 2008;35:495-508.
10. CarraMC, Huynh N, LavigneGJ. Diagnostic accuracy of sleep bruxism scoring in absence of audio-video recording: a pilot study. Sleep Breath. 2015;19:183-90.
11. KlasserGD, Nathalie R, Lavigne GJ. Sleep Bruxism Etiology: The evolution of a Changing Paradigm. J Can Dent Assoc. 2015;81:f2.
12. WinocurE, UzielN, LishaT, Goldsmith C, Eli I. Self-reported Bruxism – associations with perceived stress,motivation for control, dental anxiety, and gagging. J Oral Rehabil.2010;38:3-11.
13. CastroflorioT, BargelliniA, Rossini G, CugliariG, Deregibus A, ManfrediniD. Agreement between clinical and portable EMG/ECG diagnosis of sleep bruxism. J Oral Rehabil.2015;42:759-64.
14. Landis J. R., Koch G. G. The measurement of observer agreement for categorical data.Biometrics.1977;33:159-74.
15. Raphael KG, JanalMN, SiroisDA, DubrovskyB, KlausnerJJ, Krieger AC, LavigneGJ. Validity of self-reported sleep bruxism among myofascialtemporomandibulardisorder patients and controls.J Oral Rehabil.2015;42:751-8.
16. ManfrediniD, LobbezooF. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral SurgOral Med Oral PatholOral RadiolEndod.2010;109:26-50.
17. SommerI, et al. Review of self-reported instruments that measure sleep dysfunction in patients suffering from temporomandibular disorders and/or orofacialpain. Sleep Med. 2015;16:27-38.
18. CasettE, EusJCR, Stuginski-Barbosa J, Porporatti AL, CarraMC, Peres MA, De Luca Canto G, ManfrediniD. Validity of different tools to assess sleep bruxism: a meta-analysis. J Oral Rehabil. 2017;44:722-34.
19. American Academy of Sleep Medicine. International classification of sleep disorders, revised: Diagnostic and coding manual. Chicago, Illinois: American Academy of Sleep Medicine, 2001.
Rosemary SadamiArai Shinkai
Correio eletronico: rshinkai@pucrs.br
Ethical disclosures
Protection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interest
The authors have no conflicts of interest to declare.
Appendices
Supplementary content Supplementary data associated with this article can be found, in the online version, at http://doi.org/10.24873/j.rpemd.2018.06.219
Article history:
Received 14 February 2018
Accepted 24 May 2018
Availableonline 22 June2018